Abstract
Transthyretin-related (ATTR) cardiac amyloidosis is currently lacking a disease-modifying therapy. Despite demonstration of effectiveness in halting amyloid deposition, no study focused on epigallocatechin-3-gallate (EGCG) impact on patient survival. We sought to explore prognostic impact of EGCG in a cohort of lone cardiac ATTR patients. From the Florence Tuscan Regional Amyloid Centre database, we retrospectively selected ATTR patients treated with EGCG (675mg daily dose) for a minimum of 9 months, between March 2013 and December 2016. As a control group, we selected ATTR patients who received guideline-directed medical therapy alone. End point of the study was time to all cause death or cardiac transplantation. Sixty-five patients (30 treatment groups vs. 35 control groups) had a median follow-up of 691 days. There were no differences in baseline characteristics between groups. Five deaths occurred in EGCG group versus eight in control group; one patient underwent effective cardiac transplantation in EGCG group. There was no difference in survival estimates between EGCG and control group (60 ± 15% vs. 61 ± 12%, p = 0.276). EGCG was well tolerated, without major safety concerns. In a real-world cohort of ATTR patients with lone cardiac involvement, EGCG was a safe therapeutic option, but was not associated with survival improvement.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Amyloidoses are rare diseases characterized by extracellular deposition of insoluble protein-derived fibrils in various tissues and organs, including the heart [1]. According to precursor protein, the two most relevant etiologies of cardiac amyloidosis are light-chain amyloidosis (AL), in which misfolded proteins are derived from a clonal expansion of immunoglobulin-producing plasma cells, and transthyretin-related amyloidosis (ATTR). The latter can be further classified as wild-type amyloidosis (ATTRwt), which results from the aggregation of a structurally normal transthyretin protein, and mutant-ATTR (ATTRm), an inheritable form due to a mutation that results in a precursor protein prone to misfolding and deposition. While in the past several years, several therapeutic schemes proved their efficacy in AL treatment, changing disease progression and modifying life expectancy [2]; few drugs are available for ATTR, with unclear effect on survival [3]. Diflunisal, a nonsteroidal anti-inflammatory drug, despite promising results in slowing familiar amyloid polyneuropathy (FAP) progression [4], is encumbered by gastric and renal side effects that often lead to drug discontinuation. Doxycycline plus taurodeoxycholic acid were able to stabilize disease for at least 1 year in a small TTR amyloidosis cohort [5], but larger studies are lacking and doxycycline is also encumbered by gastric and cutaneous side effects. Tafamidis (Vyndaquel ®, Pfizer U.S.A.) has been approved by European Medicines Agency (EMA) for treatment of stage 1 familiar amyloid polyneuropathy, but its efficacy in the treatment of ATTR cardiac involvement is still under investigation [6]. Small interfering RNA (siRNA) agents, such as Patisiran (Alnylam ®, Cambridge MA), may in the future be a promising therapeutic option, as demonstrated by serum TTR protein reduction in a phase 2 trial [7]; their efficacy in treating FAP patients is currently under investigation in a phase 3 trial (Apollo NCT01960348) [8]. None of the above-mentioned drugs have been tested in a cohort of lone ATTR cardiac involvement.
An effective and well-tolerated therapy to treat ATTR cardiac amyloidosis is a major clinical need.
Several reports suggest that epigallocatechin-3-gallate (EGCG), a green tea extracted catechin, is able to inhibit fibrils formation from both AL and TTR precursor proteins. It also is effective in converting existing fibril aggregates into soluble non-fibrillar structures both in vitro and in mice models [9,10,11,12]. Other clinical reports suggest that EGCG is able to reduce cardiac disease progression both in patients with TTR and AL amyloidosis [13,14,15,16], without major safety concerns, but no data on survival improvement are available.
Therefore, in our regional amyloidosis referral center, ECGC was tested in the past few years as a potential off-label treatment option in cardiac ATTR patients.
The aim of our study is to evaluate the prognostic impact of ECGC on a cohort of cardiac ATTR patients.
Methods
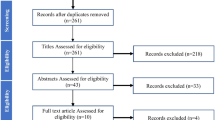
From the Florence Tuscan Regional Amyloid Centre database, we retrospectively evaluated all the ATTR patients treated with EGCG, on top of heart failure medical therapy. As the control group, from the same dataset, we identified all ATTR patients receiving heart failure medication alone, diagnosed and managed in the same time lapse of the EGCG cohort.
Patients were eligible for analysis if EGCG was administered for a minimum of 9 months without interruption, and if they were not on contemporary treatment with tafamidis, diflunisal, or doxycycline.
The end point of the study was time to all cause death or heart transplantation, whichever came first. Time to event was calculated from the date of ATTR diagnosis, and follow-up was closed by phone interview on 1st November 2017.
Baseline and 1-year follow-up characteristics were recorded using the comprehensive tools of transthoracic echocardiography and biohumoral markers.
The treatment scheme consisted in administration of five capsules a day of Epinerve® (Sifi Spa, Italy), a 90% dry extract of Camellia sinensis with 135 mg of EGCG for each capsule (total EGCG daily dose = 675 mg). Drug administration was started at the time of the definite diagnosis, when the baseline evaluation was made. Due to warnings on liver toxicity after high-dose administration (1500 mg/kg) of EGCG in mice [17], all patients administered with EGCG were asked to have periodic liver enzyme levels tested.
Diagnosis of ATTR amyloidosis was based on tissue biopsy with anti-TTR antibody staining (irrespectively of bone-tracer cardiac uptake at scintigraphy), or, in the absence of positive tissue biopsy, according to Gillmore et al. [18], by a Perugini grade 2 or 3 cardiac uptake on a bone-tracer radionuclide scintigraphy, in the absence of a detectable monoclonal protein, in a patient with echocardiogram or MRI suggestive of amyloidosis. Diagnosis of ATTRm or ATTRwt was made according to the presence or absence of mutation at genotyping. To define a patient’s baseline prognosis, we applied the staging system developed by Gillmore et al. [19].
All patients gave written informed consent for their clinical records to be used for research purposes, in accordance with Institutional Review Board guidelines.
Echocardiography evaluation
Two-dimensional targeted M-mode echocardiography was derived from the longitudinal parasternal view to ensure optimal angulation of the ultrasonic beam. LV internal dimensions, posterior wall, and interventricular septum thicknesses were analyzed according to the standards of the American Society of Echocardiography [20]. LV mass was calculated according to Devereux’s formula and was indexed to body surface area. Transmitral flow velocity in early (E) and late (A) diastoles was measured by conventional pulsed Doppler in the apical 4-chamber view. E/E’ ratio was also assessed as an index of LV diastolic function. Tricuspid annular plane systolic excursion (TAPSE) and pulmonary artery systolic pressure (PASP) were also recorded.
Statistics
Continuous variables are expressed as mean values and standard deviation or median and inter-quartile range [IQR], as appropriate, and categorical variables as frequencies and percentages. Multiple comparisons for continuous variables were performed with ANOVA; categorical variables were compared by mean of Chi-square test. Echocardiographic and biohumoral characteristic comparison between baseline and 1-year follow-up in both groups was performed with a general linear model repeated measure analysis. Survival curves were plotted according to Kaplan–Meier survival estimate, and significance was tested with the log-rank test. All statistical analyses and comparisons were performed with SPSS 23 Version IBM Package, and we considered statistical significance with p value < 0.05.
Results
According to the above mentioned criteria, we identified 35 ATTR patients treated with EGCG, diagnosed between March 2013 and December 2016. Among them, three patients were excluded due to the simultaneous administration of tafamidis, diflunisal, or doxycycline. Two patients discontinued EGCG after 2 months due to diarrhea that resolved after drug interruption, and were therefore excluded. In the 30 remaining patients, EGCG was the drug of first choice in 26, while 4 patients were shifted to EGCG after acute gastric intolerance to diflunisal (2 subjects) or doxycycline (2 subjects). Mean treatment duration was 18.2 months (median = 16, IQR = 10–38).
From the same centre dataset, we identified 35 ATTR patients, diagnosed between March 2013 and December 2016, who were treated with heart failure supportive therapy alone, as control group.
Table 1 shows baseline characteristics of the two groups. No statistically significant differences were observed in clinical and echocardiographic parameters. Biomarker levels were also similar in the two groups. All patients showed clear cardiac amyloidosis with heart retention at HMDP scintigraphy and mean wall thickness > 12 according to organ involvement in systemic amyloidosis current guideline [21]. According to etiology, 9/30 pts (30%) in ECGC group suffered from ATTRm (6 patients Val122Ile, 3 patients Ile68Leu), while 5/35 patients (14%) in the control group showed a TTR-gene mutation (2 patients Val122Ile, 3 patients Ile68Leu) (p = ns). No a priori selection of TTR-gene mutation was performed, the mutation distribution reflects the expected geographical TTRm admixture previously described by our referral centre [22,23,24].
At 1-year evaluation, echocardiographic and NT-proBNP data were available in 48 patients (25 in the EGCG and 23 in the control group Table 2).
After the first year of treatment, no significant difference is observed in disease progression between EGCG and control group (Table 2). In fact a slight increase in LV wall thickness with a LV cavity reduction and RV systolic function worsening are observed in both groups.
After a median follow-up of 691 days (IQR = 201–1730 days), 13 deaths occurred, 5 in patients on EGCG (16.6%) and 8 in patients in the control group (22.8%). Twelve deaths were in patients with ATTRwt and one in patients with ATTRm (Val122Ile). One ATTRwt patient on EGCG required heart transplantation due to refractory heart failure. Twelve out of 13 deaths (92%) were cardiac related. One patient in the control group died because of metastatic prostate cancer.
Kaplan–Meier survival curves according to treatment group are reported in Fig. 1. There is no statistically significant difference in survival between treatment and control group (62 ± 14% vs. 61 ± 12%, respectively, p = 0.232).
Due to an imbalance, despite being non-statically significant, in ATTRm distribution between groups, we also performed a Kaplan–Meier survival analysis focusing on the ATTRwt population (21 patients in EGCG group, 30 in the control group). No significant difference is recorded in baseline characteristics between ATTRwt population and control group (Table 3 supplement material). The subgroup analysis does not show any survival benefit in EGCG arm compared to control group (44 ± 17% vs. 60 ± 13%, respectively, p = 0.695) (Fig. 2).
No major safety issues emerged at follow-up. Except for the two patients who discontinued EGCG due to diarrhea, no significant adverse events were caused by EGCG, nor were significant liver test abnormalities reported.
Discussion
To the best of our knowledge, this is the first report considering the effect of EGCG on survival in a cohort of ATTR patients. Despite a small favorable numerical difference for EGCG (20% deaths or heart transplantations vs. 22.8% in the control group, p = ns) data suggest that in a real-world setting, no survival benefit can be expected with EGCG-based therapy in the ominously poor prognosis of ATTR cardiac amyloid patients. Moreover, our data demonstrate that after 1 year of treatment, if compared to a control group, EGCG does not provide a significant improvement in echocardiographic performance parameters or NT-proBNP plasma values (Table 2).
Since Professor Hunstein’s self-administration report [25], several studies suggest that EGCG is able to interfere with amyloid disease progression [8,9,10,11,12,13,14,15]. Kristen AV et al. demonstrated in a cohort of ATTR patients that no progression of LV wall thickness and LV mass, as indicators of amyloid deposition, is observed after 1 year of EGCG treatment. Furthermore, cardiac MRI studies from the same investigators suggest a trend toward LV myocardial mass reduction in patients with cardiac TTR-related amyloidosis undergoing EGCG treatment [14, 15]. These studies suggest that EGCG might be effective in halting cardiac amyloid disease progression, without adding much information about its prognostic impact.
Our study tries to add some more data to fill this gap in knowledge. Our results show, in a relatively small but homogenous cohort, that the treatment for a mean of 18 months with a 675 mg daily dose of EGCG is not associated with improved survival. Furthermore, our data suggest that no significant improvement is achieved after 12 months of treatment in echocardiographic parameters and in NT-proBNP plasma values.
At the same time, ECGC is a safe and well-tolerated treatment with no serious adverse events reported at the administered dose.
In the absence of proven effective treatments for ATTR cardiac amyloidosis and with severe side effects from other drugs tested, EGCG remains an appealing option due to its low cost, easy availability, and absence of severe side effects. We have not stopped EGCG treatment in the surviving patients, and hope that this inconclusive registry will prompt further investigation with an adequately powered placebo controlled study performed before definitively admitting defeat over this therapeutic option.
Limitations
Several limitations should be considered in the interpretation of our study. First of all, it is a retrospective, non-placebo controlled study: thus, it should be considered as hypothesis generating. No definite assumption can be made about a causative relation between treatment and outcome. Due to the non-randomized nature of the registry, we cannot exclude that residual confounders could have influenced the results. The small sample size could have resulted in inadequate statistical power in detecting differences between groups. Moreover, echocardiographic and biohumoral data at 1-year follow-up were available only in a portion of the baseline population. Due to the progressive nature of heart failure in cardiac amyloidosis and the assumption that ECGC mainly acts by halting disease progression, maybe a longer follow-up is needed to find an outcome difference between treated and untreated patients. Cardiac MRI is not regularly performed as a part of clinical evaluation; therefore, subtle cardiac function improvement not evidenced at echocardiographic evaluation could have been missed.
Conclusions
In a real-world cohort of ATTR patients with lone cardiac involvement, EGCG is well tolerated, without major safety concerns, but is not associated with survival improvement.
References
Perfetto F, Cappelli F, Bergesio F, Ciuti G, Porciani MC, Padeletti L (2013) Moggi Pignone A cardiac amyloidosis: the heart of the matter. Intern Emerg Med 8:191–203
Wechalekar AD, Gillmore JD, Hawkins PN (2016) Systemic amyloidosis. Lancet 387(10038):2641–2654
Grogan M, Scott CG, Kyle RA, Zeldenrust SR, Gertz MA, Lin G, Klarich KW, Miller WL, Maleszewski JJ, Dispenzieri A (2016) Natural history of wild-type transthyretin cardiac amyloidosis and risk stratification using a novel staging system. J Am Coll Cardiol 68(10):1014–1020
Berk JL, Suhr OB, Obici L, Sekijima Y, Zeldenrust SR, Yamashita T et al (2013) Repurposing diflunisal for familial amyloid polyneuropathy a randomized clinical trial. JAMA 310:2658–2667
Obici L, Cortese A, Lozza A, Lucchetti J, Gobbi M, Palladini G, Perlini S, Saraiva MJ, Merlini G (2012 Jun) Doxycycline plus tauroursodeoxycholic acid for transthyretin amyloidosis: a phase II study. Amyloid 19(Suppl 1):34–36
Maurer MS, Elliott P, Merlini G, Shah SJ, Cruz MW, Flynn A, Gundapaneni B, Hahn C, Riley S, Schwartz J, Sultan MB, Rapezzi C (2017) ATTR-ACT study investigators. Design and rationale of the phase 3 ATTR-ACT clinical trial (Tafamidis in transthyretin cardiomyopathy clinical trial). Circ Heart Fail. https://doi.org/10.1161/CIRCHEARTFAILURE.116.003815
Suhr OB, Coelho T, Buades J, Pouget J, Conceicao I, Berk J, Schmidt H, Waddington-Cruz M, Campistol JM et al (2015) Efficacy and safety of patisiran for familial amyloidotic polyneuropathy: a phase II multi-dose study. Orphanet J Rare Dis 10:109
Adams D, Suhr OB, Dyck PJ, Litchy W, Leahy RG, Chen J, Gollob J (2017) Coelho T Trial design and rationale for APOLLO, a phase 3, placebo-controlled study of patisiran in patients with hereditary ATTR amyloidosis with polyneuropathy. BMC Neurol 17:181
Ehrnhoefer DE, Bieschke J, Boeddrich A, Herbst M, Masino L, Lurz R, Engemann S, Pastore A (2008) Wanker EE EGCG redirects amyloidogenic polypeptides into unstructured, offpathway oligomers. Nat Struct Mol Biol 15:558–566
Ferreira N, Cardoso I, Domingues MR, Vitorino R, Bastos M, Ba G, Saraiva MJ, Almeida MR (2009) Binding of epigallocatechin- 3-gallate to transthyretin modulates) its amyloidogenicity. FEBS Lett 19(583):3569–3576
Ferreira N, Saraiva MJ (2012) Almeida MR epigallocatechin-3-gallate as a potential therapeutic drug for TTR-related amyloidosis: ‘‘in vivo’’ evidence from FAP mice models. PLoS ONE 7(1):e29933
Ferreira N, Saraiva MJ, Almeida M (2012) Natural polyphenols as modulators of TTR Amyloidogenesis in vitro and in vivo evidences towards therapy. Amyloid 19(S1):39–42
Kristen AV, Lehrke S, Buss S, Mereles D, Steen H, Ehlermann P, Hardt S, Giannitsis E, Schreiner R, Haberkorn U, Schnabel PA, Linke RP, Rocken C, Wanker EE, Dengler TJ, Altland K, Katus HA (2012) Green tea halts progression of cardiac transthyretin amyloidosis: an observational report. Clin Res Cardiol 101(10):805–813
Mereles D, Buss SJ, Hardt SE, Hunstein W, Katus HA (2010) Effects of the main green tea polyphenol epigallocatechin-3-gallate on cardiac involvement in patients with AL amyloidosis. Clin Res Cardiol 99:483–490
Aus dem Siepen F, Buss SJ, Andre F, Seitz S, Giannitsis E, Steen H, Katus HA, Kristen AV (2015) Extracellular remodeling in patients with wild-type amyloidosis consuming epigallocatechin-3-gallate: preliminary results of T1 mapping by cardiac magnetic resonance imaging in a small single center study. Clin Res Cardiol 104(8):640–647
Aus dem Siepen F, Bauer R, Aurich M, Buss SJ, Steen H, Altland K, Katus HA, Kristen AV (2015) Green tea extract as a treatment for patients with wild-type transthyretin amyloidosis: an observational study. Drug Design Dev Therapy 9 6319–6325
Lambert JD, Kennett MJ, Sang S, Reuhl KR, Ju J, Yang CS (2010) Hepatotoxicity of high oral dose (-)-epigallocatechin-3-gallate in mice. Food Chem Toxicol 48(1):409–416
Gillmore JD, Maurer MS, Falk RH, Merlini G, Damy T, Dispenzieri A et al (2016) Nonbiopsy diagnosis of cardiac transthyretin amyloidosis. Circulation 133(24):2404–2412
Gillmore JD, Damy T, Fontana M, Hutchinson M, Lachmann HJ, Martinez-Naharro A, Quarta CC, Rezk T, Whelan CJ, Gonzalez-Lopez E, Lane T, Gilbertson JA, Rowczenio D, Petrie A, Hawkins PN (2017) A new staging system for cardiac transthyretin amyloidosis. Eur Heart J. https://doi.org/10.1093/eurheartj/ehx589
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt JU (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28(1):1–39.e14
Gertz MA, Comenzo R, Falk RH et al (2005) Definition of organ involvement and treatment response in immunoglobulin light chain amyloidosis (AL): a consensus opinion from the 10th international symposium on amyloid and amyloidosis. Am J Hematol 79:319–328
Cappelli F, Frusconi S, Bergesio F, Grifoni E, Fabbri A, Giuliani C, Falconi S, Bonifacio S, Perfetto F (2016) The Val142Ile transthyretin cardiac amyloidosis: not only an afro American pathogenic variant? A single center Italian experience. J Cardiovasc Med 2016 17(2):122–5.44
Rapezzi C, Quarta CC, Obici L, Perfetto F, Longhi S, Salvi F, Biagini E, Lorenzini M, Grigioni F, Leone O, Cappelli F, Palladini G, Rimessi P, Ferlini A, Arpesella G, Pinna AD, Merlini G, Perlini S (2013 Feb) Disease profile and differential diagnosis of hereditary transthyretin-related amyloidosis with exclusively cardiac phenotype: an Italian perspective. Eur Heart J 34(7):520–528
Perfetto F, Cappelli F, Bergesio F (2011 Jun) Asymptomatic homozygous gene carrier in afamily with Ile68Leu ATTR amyloidosis: a new endemic region in northern Tuscany? J Cardiovasc Med (Hagerstown). 12(6):450–451
Hunstein W (2007) Epigallocathechin-3-gallate in AL amyloidosis: a new therapeutic option? Blood 110:2216
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Cappelli, F., Martone, R., Taborchi, G. et al. Epigallocatechin-3-gallate tolerability and impact on survival in a cohort of patients with transthyretin-related cardiac amyloidosis. A single-center retrospective study. Intern Emerg Med 13, 873–880 (2018). https://doi.org/10.1007/s11739-018-1887-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-018-1887-x