Abstract
Emergency department (ED) overcrowding remains a significant problem in many hospitals, and results in multiple negative effects on patient care outcomes and operational metrics. We sought to test whether implementing a quality improvement project could decrease ED LOS for trauma patients requiring an ICU admission from the ED, specifically by directly admitting critically ill trauma patients from the ED CT scanner to an ICU bed. This was a retrospective study comparing patients during the intervention period (2013–2014) to historical controls (2011–2013). Critically ill trauma patients requiring a CT scan, but not the operating room (OR) or Interventional Radiology (IR), were directly admitted from the CT scanner to the ICU, termed the “One-way street (OWS)”. Controls from the 2011–2013 Trauma Registry were matched 1:1 based on the following criteria: Injury Severity Score; mechanism of injury; and age. Only patients who required emergent trauma consult were included. Our primary outcome was ED LOS, defined in minutes. Our secondary outcomes were ICU LOS, hospital LOS and mortality. Paired t test or Wilcoxon signed rank test were used for continuous univariate analysis and Chi square for categorical variables. Logistic regression and linear regressions were used for categorical and continuous multivariable analysis, respectively. 110 patients were enrolled in this study, with 55 in the OWS group and 55 matched controls. Matched controls had lower APACHE II score (12 vs. 15, p = 0.03) and a higher GCS (14 vs. 6, p = 0.04). ED LOS was 229 min shorter in the OWS group (82 vs. 311 min, p < 0.0001). The time between CT performed and ICU disposition decreased by 230 min in the OWS arm (30 vs. 300 min, p < 0.001). There was no difference in ED arrival to CT time between groups. Following multivariable analysis, mortality was primarily predicted by the APACHE II score (OR 1.29, p < 0.001), and not ISS, mechanism of injury, or age. After controlling for APACHE II score, there was no difference in mortality between the two cohorts (OR = 0.49, p = 0.28). Expedited admission of critically ill trauma patients immediately following CT imaging significantly reduced ED LOS by 3.82 h (229 min), without a change in ICU LOS, hospital LOS, or mortality. Further studies are needed to assess the impact of expedited admission on morbidity and mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Emergency department (ED) overcrowding is a major problem in many hospitals [1], with multiple studies documenting that overcrowding results in delays in care and increased mortality [2–5]. Last year in our ED we received 108, 436 ED visits and 486 trauma activations, the majority (63 %) being critical. 189 needed an ICU transfer, 103 an operation and 16 died in the ED. Critically ill patients requiring an intensive care unit (ICU) admission who board in the ED have increased hospital length of stay (LOS). Our median length of stay in the ED for admitted patients is 7.6 h (mean 9.7 h), and we have an estimated 55 boarder patients per day, that board in the ED for an average of 5 h. This delay in care or overcrowding has the potential to worsen multi-organ failure, and increase mortality both in the ICU and hospital [6–8].
This might be especially true for the trauma patients, where a short delay in responding to their critical needs can have instantaneous adverse effects [9].
To address this issue at our institution, our American College of Surgeons level-one verified trauma center began a quality improvement project to decrease ED LOS for trauma patients requiring ICU admission. A multidisciplinary team with representation from multiple departments, including Emergency Medicine, Intensive Care, Trauma Surgery and Radiology, created a new protocol that would admit a critically ill trauma patient directly from the ED Computed Tomography (CT) scanner to the ICU (Fig. 1). The new protocol was called One-way street (OWS). The primary goal of this study was to evaluate if implementation of OWS reduced ED LOS when compared to previous practice. Secondary outcomes included in-hospital mortality, ICU LOS and hospital LOS.
Methods
Patient selection
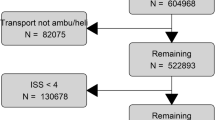
This was a retrospective, case–control, IRB-approved study (IRB #2013P000382) comparing the intervention period (2013–2014) to historical controls (2011–2013). Starting April 2013 all critically ill trauma patients requiring a CT scan, but not the operating room (OR) were directly admitted from the CT scanner to the ICU. These patients were prospectively followed by the quality improvement area in the trauma division between 2013 and 2014. Historical controls (2011–2013) were identified using the Trauma Registry. The matched controls had to be patients who went from the ED to the CT scanner and then back to the ED before their final transfer to the ICU. OWS patients were matched 1:1 to historical controls based on the following criteria: Injury Severity Score (±5); mechanism of injury (±5); and age (±5). Only patients who required an emergent trauma consult (Trauma Activation) were included in the study (Fig. 2). Exclusion criteria included the following: patients aged less than 16 years; who went directly to the OR from the ED; who died in the ED, or who required a delayed trauma consult that required an ICU admission.
Data collection and definitions
General demographics, hospital and ICU LOS, ISS, transfer from outside hospital status for both cohorts were retrospectively collected from the trauma registry. All other data were collected from our electronic medical records and nursing paper documentation. ED length of stay was defined as time elapsed from ED arrival to arrival in ICU, and calculated as time from ED arrival to CT plus time from CT ICU arrival; data were obtained from the EMR and ICU nursing flow sheets. Time from ED to CT was defined as ED arrival to ED CT, and calculated from ED Nursing Documentation and radiology documentation. Similarly, time from CT to ICU was then calculated from the first CT completion time to the time of arrival to the ICU.
Outcomes
Our primary outcome was ED LOS, defined in minutes. Our secondary outcomes were ICU LOS, hospital LOS and mortality. Hospital and ICU LOS were defined in days.
Statistical analysis
The Shapiro–Wilk test was used to test the data for normality. Normally distributed, continuous variables were reported as means and standard deviations. Non-normally distributed data were reported as medians with interquartile ranks. Categorical variables were reported as percentages. For univariate analysis, we used either a paired t test or Wilcoxon signed rank test for continuous variables and Chi square for categorical variables. For multivariate analysis a logistic regression was performed to identify independent predictors of mortality. For continuous outcomes, a linear regression was performed to identify the independent predictors of hospital LOS, ED LOS and ICU LOS. All analysis were performed using STATA software, version 13.1MP (StataCorp, College Station, TX).
Results
Study population
One hundred and ten patients were enrolled in this study, with 55 in the OWS group and 55 matched controls. These 55 OWS patients represented 35 % of all SICU admissions for trauma during the study time (55/155). The remaining 100 SICU trauma admissions either did not require trauma team activation, or were directly admitted from the OR. Patient demographics are summarized in Table 1. Matched controls were overall healthier upon arrival in the ED as noted by their lower APACHE II score (12 vs. 15, p = 0.03) and a higher GCS (14 vs. 6, p = 0.04).
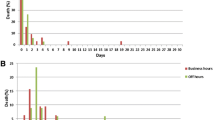
ED length of stay
Outcomes are summarized on Table 2. ED LOS was 229 min shorter in the OWS group (p < 0.0001). This difference is explained by a shorter time between CT and ICU in the OWS arm (30 vs. 300 min, p < 0.001). Time spent in the ED before CT scan did not differ between groups. After controlling for GCS, APACHE II score and transfer status, ED LOS was still statistically significant (Table 3).
Secondary outcomes
Univariate analysis of mortality finds that the mortality is higher among the OWS group when compared to historical controls (25.5 vs. 10.9 %, p = 0.05). However, the multivariate analysis finds that the mortality is primarily predicted by the APACHE II score (OR 1.29, p < 0.001) and not ISS, mechanism of injury, nor age. After controlling for APACHE II score, there is no difference in the mortality between the two cohorts (OR = 0.49, p = 0.28) (Table 4).
As shown on Table 2, ICU LOS is similar in both groups and hospital LOS is shorter in the OWS cohort (8 vs. 11 days, p = 0.03). Further subgroup analysis of only survivors finds that hospital LOS is the same between the two groups (10 vs. 8 days, p = 0.46) (Table 5).
Discussion
Our study finds that a protocol for expedited admission of critically ill trauma patients to the ICU significantly reduces ED LOS by 3.82 h (229 min), without a change in ICU LOS, hospital LOS and mortality. There are multiple potential explanations for this result, but this study demonstrates that it is both feasible and effective to prioritize expedited admissions, and that focusing on a process improvement intervention that reduces waste and delays can pay significant dividends. In addition, while non-value added delays in the original process likely contributed to the effect size of our intervention, this study further highlights the importance of focusing on efficiency in the admission process, reducing and eliminating process steps and waits, and effectively utilizing limited resources (e.g., ICU and ED bed capacity).
However, the obvious risk in more rapidly admitting a cohort of critically ill trauma patients is that eliminating their post-CT ED stay may be associated with worsening, rather than improved, patient outcomes. We find that while unadjusted mortality is higher among our intervention group, this is fully accounted for by APACHE II, and despite adjustment for ISS, mechanism of injury, and age. These increased acuity in the intervention group is well documented in not only higher APACHE II scores, but also need for endotracheal intubation. This could be potentially explained by a few reasons. First, our cohort of trauma patients were different from the original studies that validated ISS [10, 11] in trauma, and as a result a physiologic or comorbidity index might be a better predictor of mortality than ISS [12]. Second, patients who would have otherwise died in the ED were more rapidly transferred to the ICU faster in the OWS group, and thus more frequently died in the ICU instead of the ED. Clearly, this patient population would be included in the OWS cohort but not in the matched controls. Third, there could be epiphenomenon with improving health care that changed our trauma population. For example, despite matching for age, the newer trauma population might have more comorbidities and physiologic derangements at baseline that predisposes them to increased mortality. Lastly, Richardson et al. also show that experienced emergency physicians are able to efficiently triage sicker trauma patients and have them admitted faster [13]; so it could be that once the OWS protocol was implemented, physicians more effectively triaged sicker patients towards the streamlined ICU pathway, thus creating a selection bias. Regardless, OWS patients were sicker, and after controlling for APACHE 2 score, mortality was not found to be different between the two groups.
Multiple previous studies report that boarding of patients in the ED results in worse patient outcomes. In a recent study by Singer et al. examining over 40,000 patients admitted to the ED, ED boarding is associated with an increased mortality, need for ICU admission and hospital LOS [14]. Similarly Hung et al. show an increase in mortality and an increase in resource expenditure for patients who spend greater than 4 h in the ED while on mechanical ventilation [8]. Contrary to their findings, our study does not find a different in mortality ICU LOS, and hospital LOS; however, our study was not powered to examine these specific outcomes. Even without significant findings in mortality and LOS, we believe that reducing ED LOS has the potential for improving patient outcomes for not just the specific patient in question, but also for all the other patients in the ED. There are many unmeasured downstream benefits to reducing ED overcrowding. As ICU patients are extremely resource intensive, decompressing the ED of ICU patients would make resources that were previously tied up now available.
Limitations
There are potential limitations to this study. First, this was a retrospective study, and therefore we were not able to prospectively control for confounding variables, and relied on the accuracy of the medical records to obtain information retrospectively. In addition, as with any before–after study, while the outcomes measured may have demonstrated a change, they do not prove causality. The observed changes may have in part been due to some other contributing factor that occurred over the study period that cannot be fully excluded; however, given the effect size and intervention type this is less likely. Furthermore, given the retrospective nature of the manuscript we were not able to document the negative impact an early transfer to the ICU could potentially have. For instance should a patient require further diagnostic tests that are more easily accessible in the ED than the ICU, we would be unable to account for this negative impact of early transfer to the ICU. This is certainly a very interesting topic that should be investigated in the future; however, at our institution this would be less likely as trauma patients typically have already received their pan-CT scan immediately before ICU admission.
In addition, our intervention arm was by definition aimed at the most critically ill trauma patients, requiring both a trauma activation and immediate transfer to the ICU, and therefore a selection bias is possible, reflected in the higher APACHE II score in the intervention arm. Unfortunately, our sample size was also not adequately powered to detect differences in our secondary outcomes and avoid a Type II error. Finally, given this study was performed at a single, academic, quaternary care, level-one trauma center, our results might not be fully generalizable to hospitals in other settings.
Conclusion
In our hospital, streamlined OWS admission of critically ill trauma patients to the ICU reduces ED LOS without measurable negative patient care consequences.
References
Dickinson G (1989) Emergency department overcrowding. CMAJ 140:270–271
Richardson DB (2006) Increase in patient mortality at 10 days associated with emergency department overcrowding. Med J Aust 184:213–216
Pines JM, Hollander JE, Localio AR, Metlay JP (2006) The association between emergency department crowding and hospital performance on antibiotic timing for pneumonia and percutaneous intervention for myocardial infarction. Acad Emerg Med 13:873–878
Pines JM, Localio AR, Hollander JE et al (2007) The impact of emergency department crowding measures on time to antibiotics for patients with community-acquired pneumonia. Ann Emerg Med 50:510–516
Fee C, Weber EJ, Maak CA, Bacchetti P (2007) Effect of emergency department crowding on time to antibiotics in patients admitted with community-acquired pneumonia. Ann Emerg Med 50:501–509 (509.e1)
Nguyen HB, Rivers EP, Havstad S et al (2000) Critical care in the emergency department: a physiologic assessment and outcome evaluation. Acad Emerg Med 7:1354–1361
Chalfin DB, Trzeciak S, Likourezos A, Baumann BM, Dellinger RP, group D-Es (2007) Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med 35:1477–1483
Hung SC, Kung CT, Hung CW et al (2014) Determining delayed admission to intensive care unit for mechanically ventilated patients in the emergency department. Crit Care 18:485
Sampalis JS, Denis R, Frechette P, Brown R, Fleiszer D, Mulder D (1997) Direct transport to tertiary trauma centers versus transfer from lower level facilities: impact on mortality and morbidity among patients with major trauma. J Trauma 43:288–295 (discussion 95-6)
Baker SP, O’Neill B, Haddon W Jr, Long WB (1974) The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma 14:187–196
Copes WS, Champion HR, Sacco WJ et al (1990) Progress in characterizing anatomic injury. J Trauma 30:1200–1207
Ladha KS, Zhao K, Quraishi SA et al (2015) The Deyo-Charlson and Elixhauser-van Walraven comorbidity indices as predictors of mortality in critically ill patients. BMJ Open 5:e008990
Richardson JD, Franklin G, Santos A et al (2009) Effective triage can ameliorate the deleterious effects of delayed transfer of trauma patients from the emergency department to the ICU. J Am Coll Surg 208:671–678 (discussion 8-81)
Singer AJ, Thode HC Jr, Viccellio P, Pines JM (2011) The association between length of emergency department boarding and mortality. Acad Emerg Med 18:1324–1329
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Fuentes, E., Shields, JF., Chirumamilla, N. et al. “One-way-street” streamlined admission of critically ill trauma patients reduces emergency department length of stay. Intern Emerg Med 12, 1019–1024 (2017). https://doi.org/10.1007/s11739-016-1511-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-016-1511-x