Abstract
Single-incision laparoscopic cholecystectomy (SILC) has declined in popularity, posing a challenge for novice surgeons. However, robotic single-site cholecystectomy (RSSC) has gained popularity in hepatopancreatic surgery, suggesting a paradigm shift in minimally invasive procedures due to the advantages of robotic platforms. The purpose of this study was to compare the surgical outcomes and learning curves between experts and novices without SILC experience, and discuss the utility and potential of RSSC for novice surgeons. A total of 235 patients underwent RSSC between April 2019 and June 2023 at the OOO University Hospital. Among them, 31 cases from novice and expert surgeons were selected to compare their initial experience. Comprehensive demographic and perioperative factors were analyzed and statistical comparisons were made, including cumulative sum analysis (CUSUM) for learning curves. The demographic factors showed no statistically significant differences between the two groups. Although the docking time (P < 0.001) and hospital stay (P = 0.014) were statistically significant, the total operative time and other perioperative factors were comparable. Novice surgeons demonstrated a shorter absolute total operative time, primarily attributed to differences in docking time. The CUSUM analysis indicated a shorter learning curve for novice surgeons. This study shows that the inherent benefits of the robotic platform make it an accessible and reproducible technique for novices. The benefits of integrating observational learning into robotic surgery training programs and the intrinsic advantages of the robotic platform in minimizing the learning curve for RSSC were also highlighted.
Similar content being viewed by others

Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Robotic surgery has emerged as a pivotal approach in hepatopancreaticobiliary surgeries, including cholecystectomy, liver resection, pancreaticoduodenectomy, and liver transplantation. Robotic single-site cholecystectomy (RSSC) is one of the most frequently performed procedures using robotic platforms. The necessity of experience performing laparoscopic surgery before robotic surgery is a subject of debate, wherein evidence suggests that laparoscopic surgery may be beneficial prior to robotic surgery. Studies emphasize the indispensability of laparoscopic skills not only for port placement but also for addressing adhesions or anatomical variations that may impede the deployment of robotic instruments [1]. The literature suggests that a background in laparoscopic surgery may expedite the learning curve of robotic resection [2, 3]. Hence, laparoscopic skills may be transferred to robotic surgery; however, the extent to which they are transferred and the optimal training programs for robotic surgery are still unclear. Recent meta-analyses reflect a neutral stance on whether laparoscopic surgery contributes to the effectiveness of robotic surgery [4].
Despite the initial popularity of single-incision laparoscopic cholecystectomy (SILC) owing to its aesthetic benefits and reduced pain levels, a substantial decline in its use has been observed in recent years [5]. This decline is attributed to reported technical difficulties, including instrument collusion and restricted vision, as well as a higher incidence of complications compared to conventional laparoscopic cholecystectomy (CLC) [6, 7]. The inherent limitations of SILC present challenges for novices, leading to an extended learning curve. Therefore, the initiation of robotic surgery following mastery of SILC is particularly arduous and no longer an indispensable requirement, especially for novice surgeons.
In addition, the reported advantages of robotic surgery, such as enhanced angulation, stable 3D magnified operative field, and improved dexterity, serve to lower the entry barrier for novices. Recent reports have proposed that robotic surgery has a shorter learning curve than laparoscopy [8]. Furthermore, emerging research suggests that novices lacking prior laparoscopic experience can swiftly gain proficiency in robotic surgery [9].
In this study, we aimed to investigate and compare the surgical outcomes and learning curves of RSSC between expert and novice surgeons, both of whom had no experience in SILC. Additionally, we discuss the utility and potential of RSSC for novice surgeons, contributing valuable insights to the ongoing discourse in this field.
Materials and methods
Ethical approval
This study was approved by the ethics committee of OOO University Hospital (IRB No. OOO IRB-23-179). The requirement for informed consent was waived because of the retrospective nature of this study. The study was conducted in accordance with the principles of the Declaration of Helsinki.
Study population
Between April 2019 and June 2023, 235 patients underwent RSSC performed by two surgeons at the OOO University Hospital. The exclusion criteria for RSSC selection were the same as those in previous studies [10, 11]: (1) severe acute cholecystitis, (2) emergency room visits, (3) suspected cancer, and (4) refusal to undergo RSSC due to expense.
Among the 235 patients, 204 underwent surgery performed by an expert surgeon with advanced laparoscopic skills and experience in over 2000 CLC cases. The remaining 31 surgeries were performed by a novice surgeon with basic laparoscopic skills and experience in over 100 CLC cases. The novice surgeon assisted in RSSC procedures as a bedside surgeon in 2020 and began performing their own RSSC procedures in 2022.
Retrospective data collection was conducted on the initial 31 consecutive cases from the expert's 204 cases and 31 cases from the novice. Subsequently, a comparative analysis was performed to assess surgical outcomes.
Surgical procedures
The novice surgeon learned how to perform RSSC exclusively from our expert surgeon; therefore, the surgical techniques of the two operators were identical.
Patients were positioned in the supine and reverse Trendelenburg positions with their arms at their sides. A 2 cm trans umbilical incision was made, and a glove port (NELIS; Bucheon, Korea) was placed in it. The DaVinci Xi® system (Intuitive Surgical, Sunnyvale, CA, USA) was positioned in the right upper region after the pneumoperitoneum was established. The gallbladder was targeted using an 8 mm camera cannula placed in the blue channel. Subsequently, a 5 × 250 mm curved cannula was placed in the white channel on the right side for a permanent cautery hook. An identical cannula is placed under the hook on the left side of the crocodile grasper. The gallbladder was cranially retracted by the first assistant using a laparoscopic grasper through another white channel. Docking time was calculated starting from the skin incision. Once all the ports were in place, the cystic duct and artery were ligated using robotic Hem-o-lock® clips (Weck® Closure System; Research Triangle Park, NC, USA). Finally, the gallbladder was extracted from the fossa using a glove port. Interrupted sutures were used to close the fascia.
Statistical analyses
For categorical data, the findings were reported as percentages, and for continuous variables, as mean ± standard deviation. The t-test or Mann–Whitney U-test was used to examine continuous variables, whereas the chi-squared or Fisher's exact test was used to assess categorical variables. Statistical analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, N C, USA). The statistical significance level was set at P < 0.05. A cumulative sum analysis (CUSUM) was used. Cases were organized chronologically, with \({x}_{i}\) denoting total operative time and μ as the mean of time. As a result, CUSUM was calculated at each time point as follows [12]:
Results
Demographic and perioperative factors
Each surgeon selected 31 cases and compared their initial experience. Between the two groups, all preoperative factors including sex, age, preoperative diagnosis, body mass index, Age-adjusted Charlson Comorbidity Index [13], American Society of Anesthesiologists physical status classification, abdominal operation history, and laboratory findings were not significantly different (Table 1).
Postoperative outcomes
The operation time was defined as (1) total operative time, which is from the initial skin incision to the final skin closure, and (2) docking time, which is from the skin incision to the installation of the second robotic arm into the cannula, as in previous studies [10, 11].
Comparing the two groups, only docking time (9.68 ± 3.35 min performed by the expert surgeon versus 5.98 ± 1.48 min performed by the novice surgeon, P < 0.001) and hospital stay (2.74 ± 1.26 days in the procedure done by the expert surgeon versus 2.16 ± 0.37 days in the procedure done by the novice surgeon, P = 0.014) were statistically significant. Other factors including total operative time, total operative time minus docking time, perioperative findings, and postoperative day 1 pain score were not significantly different. Both groups did not have open conversion and postoperative complications (Table 2).
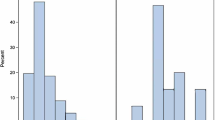
Total operative time, docking time, and total operative time minus docking time
Given the lack of statistical differences in other factors representing the comparison of surgical outcomes, a focused analysis of the operative times between the two groups is presented in Figs. 1 and 2. While the total operative time did not exhibit statistically significant differences between the two groups, it is noteworthy that the novice surgeon’s total operative time was approximately 3 min shorter than the expert surgeon’s total operative time. In contrast, the docking times showed statistically significant differences. However, when considering the time, minus the docking time, from the overall surgical time, there was no statistically significant difference between the two groups. Interestingly, the absolute value was lower in the procedure performed by the expert surgeon than that of the novice surgeon (Table 2). Evaluation of the difference in each operative time according to the operation sequence reveals a similar pattern in the graphs excluding the docking time (Fig. 2).
Cumulative sum analysis in total operative time
Comparing the CUSUM learning curves for the total operative time between the two groups, the learning curve was 15 cases in the expert surgeon and 10 cases in the novice surgeon. The maturation phases were over 18 and 16 cases for the expert and novice surgeons, respectively (Fig. 3).
Discussion
The increased adoption of RSSC in recent years has led to a proliferation of studies examining its surgical outcomes and comparing these with those of CLC and SILC. Collectively, these studies have provided substantial evidence supporting the efficacy of RSSC [5, 14,15,16]. Moreover, upon comparing the surgical outcomes of RSSC conducted at our institution with those reported in a recent publication, we observed that the results (average complication rate: 0–13.3%; conversion rate (open or laparoscopy): 0–6.7%) were not only comparable but had significantly shorter operative time even when performed by novice surgeons. (average operative time: 62.7 ± 16.6−101.57 ± 27.05 min) [16,17,18,19,20,21,22].
The study sheds light on the comparable postoperative outcomes of both experienced and novice surgeons in RSSC. Notably, the operative time and learning curve stand out as distinctive factors.
While our study indicated no statistical difference in the total operation time, the average time was shorter for novice surgeons. This discrepancy is believed to stem from differences in the docking time. Experienced surgeons required 20 min for the docking time in the initial two cases, whereas novice surgeons consistently maintained a flat docking time from the onset (Fig. 2b). This can be attributed to the fact that, unlike experienced surgeons who commenced robotic surgeries without observational learning, novices engaged in approximately two years of observational learning as bedside surgeons in robotic surgeries. For this reason, excluding the docking time from the total operation time showed no statistical difference; instead, the average times suggest that experienced surgeons performed better.
This finding aligns with the existing literature emphasizing the role of observational learning, which is the process of passively watching another individual perform a task, playing a crucial role in developing surgical expertise [23], especially when used as a supplement to physical practice [24]. In addition, the CUSUM analysis further supported a shorter learning curve for novices, likely associated with docking time and observational learning, indicating that even beginners can achieve surgical outcomes comparable to those of experienced surgeons with effective adaptation to the robotic platform.
In general, the surprising but promising fact that novices and experts had comparable operative times and postoperative outcomes reflects observational learning and the inherent advantages of the robotic platform in compensating for the lack of experience. The significant impact of observational learning on shorter docking times and learning curves of novice surgeons is crucial. This suggests that a structured training program incorporating observational learning can substantially benefit novices even before they perform their first procedure, potentially influencing the design of robotic surgery training programs that emphasize the need for both observational and hands-on surgical experience.
Despite these promising results, it is crucial to acknowledge that expert surgeons naturally possess high levels of experience and skill in performing RSSC. This expertise enables surgeons to navigate freely and manage challenging intraoperative situations more effectively, as reported by Korovin [25]. Expert surgeons are likely to exhibit superior operative performance and decision-making skills during the procedure compared with novice surgeons, as reported by Willuth [8]. Therefore, in challenging cases that may arise between the two groups, we believe that this pattern is consistent across all surgical procedures.
However, this study had some limitations. First, the data were collected retrospectively in a single-institution study with results from only one surgeon in each category, and generalizability may not be applicable. Second, the comparison, based on a limited number of cases performed by a novice surgeon over a one-year period, did not allow for matching preoperative findings between the two groups for comparison.
In conclusion, the results suggest that the intrinsic advantages of the robotic platform make it an accessible and reproducible technique for novice surgeons. These findings underscore the benefits of integrating observational learning into robotic surgery training programs, and the inherent advantages of robotic platforms in minimizing the learning curve for RSSC.
Data availability
No datasets were generated or analysed during the current study.
References
Abaza R (2009) The robotic surgery era and the role of laparoscopy training. Ther Adv Urol 1(3):161–165. https://doi.org/10.1177/1756287209344991
Gerbaud F, Valverde A, Danoussou D, Goasguen N, Oberlin O, Lupinacci RM (2019) Experience with transitioning from laparoscopic to robotic right colectomy. J Soc Laparoendosc Surg. https://doi.org/10.4293/JSLS.2019.00044
Odermatt M, Ahmed J, Panteleimonitis S, Khan J, Parvaiz A (2017) Prior experience in laparoscopic rectal surgery can minimise the learning curve for robotic rectal resections: a cumulative sum analysis. Surg Endosc 31(10):4067–4076. https://doi.org/10.1007/s00464-017-5453-9
Pietersen PI, Hertz P, Olsen RG, Møller LB, Konge L, Bjerrum F 2023. Transfer of skills between laparoscopic and robot-assisted surgery: a systematic review. Surg Endosc Germany: ©2023. The author(s), under exclusive licence to Springer Science+Business Media, LLC, part of Springer Nature.
Arezzo A, Passera R, Forcignanò E, Rapetti L, Cirocchi R, Morino M (2018) Single-incision laparoscopic cholecystectomy is responsible for increased adverse events: results of a meta-analysis of randomized controlled trials. Surg Endosc 32(9):3739–3753. https://doi.org/10.1007/s00464-018-6143-y
Evers L, Bouvy N, Branje D, Peeters A (2017) Single-incision laparoscopic cholecystectomy versus conventional four-port laparoscopic cholecystectomy: a systematic review and meta-analysis. Surg Endosc 31(9):3437–3448. https://doi.org/10.1007/s00464-016-5381-0
Lirici MM, Tierno SM, Ponzano C (2016) Single-incision laparoscopic cholecystectomy: does it work? A systematic review. Surg Endosc 30(10):4389–4399. https://doi.org/10.1007/s00464-016-4757-5
Willuth E, Hardon SF, Lang F, Haney CM, Felinska EA, Kowalewski KF et al (2022) Robotic-assisted cholecystectomy is superior to laparoscopic cholecystectomy in the initial training for surgical novices in an ex vivo porcine model: a randomized crossover study. Surg Endosc 36(2):1064–1079. https://doi.org/10.1007/s00464-021-08373-6
Zaman JA, Singh TP (2018) The emerging role for robotics in cholecystectomy: the dawn of a new era? Hepatobiliary Surg Nutr 7(1):21–28. https://doi.org/10.21037/hbsn.2017.03.01
Jeong Jang E, Kang SH, Kim KW (2021) Early outcomes of robotic single site cholecystectomy using the DaVinci Xi® system. JSLS. https://doi.org/10.4293/JSLS.2020.00082
Jang EJ, Kang SH, Kim KW (2023) Propensity score matched comparison of robotic single-site and laparoscopic cholecystectomy. JSLS. https://doi.org/10.4293/JSLS.2023.00043
Park JS, Ahn HK, Na J, Lee HH, Yoon YE, Yoon MG, Han WK (2019) Cumulative sum analysis of learning curve for video-assisted mini-laparotomy partial nephrectomy in renal cell carcinoma. Medicine (Baltim) 98(17):e15367. https://doi.org/10.1097/MD.0000000000015367
Charlson ME, Carrozzino D, Guidi J, Patierno C (2022) Charlson comorbidity index: a critical review of clinimetric properties. Psychother Psychosom. https://doi.org/10.1159/000521288
Rudiman R, Hanafi RV, Almawijaya A (2023) Single-site robotic cholecystectomy versus single-incision laparoscopic cholecystectomy: A systematic review and meta-analysis. Ann Gastroenterol Surg 7(5):709–718. https://doi.org/10.1002/ags3.12688
Lee SJ, Moon JI, Choi IS Robotic single-site cholecystectomy is better in reducing postoperative pain than single-incision and conventional multiport laparoscopic cholecystectomy. Surg Endosc. The author 37. Germany: © 2023(s), under exclusive licence to Springer Science+Business Media, LLC, part of Springer Nature.; 2023. p. 3548–56
Grochola LF, Soll C, Zehnder A, Wyss R, Herzog P, Breitenstein S (2019) Robot-assisted versus laparoscopic single-incision cholecystectomy: results of a randomized controlled trial. Surg Endosc 33(5):1482–1490. https://doi.org/10.1007/s00464-018-6430-7
Han DH, Choi SH, Kang CM, Lee WJ (2020) Propensity score-matching analysis for single-site robotic cholecystectomy versus single-incision laparoscopic cholecystectomy: a retrospective cohort study. Int J Surg 78:138–142. https://doi.org/10.1016/j.ijsu.2020.04.042
Lee SJ, Moon JI, Choi IS (2023) Robotic single-site cholecystectomy is better in reducing postoperative pain than single-incision and conventional multiport laparoscopic cholecystectomy. Surg Endosc 37(5):3548–3556. https://doi.org/10.1007/s00464-022-09846-y
Sun N, Fau ZJl, Zhang CS, Fau ZCs, Li XH, Li XhF, et al (2018) Single-incision robotic cholecystectomy versus single-incision laparoscopic cholecystectomy: A systematic review and meta-analysis. Medicine 97:36
Beltzer C, Gradinger K, Bachmann R, Axt S, Dippel H, Schmidt R (2020) Robotic multiport versus robotic single-site cholecystectomy: a retrospective single-centre experience of 142 cases. Eur Surg 52(1):16–21. https://doi.org/10.1007/s10353-019-00619-x
Ricciardiello M, Grottola T, Panaccio P, Esposito LM, Montemitro C, Mucilli F et al (2021) Outcome after single-site robotic cholecystectomy: an initial single center’s experience. Asian J Endosc Surg 14(3):496–503. https://doi.org/10.1111/ases.12903
Lee SM, Lim JH (2021) Comparison of outcomes of single incision robotic cholecystectomy and single incision laparoscopic cholecystectomy. Ann Hepatobiliary Pancreat Surg 25(1):78–83. https://doi.org/10.14701/ahbps.2021.25.1.78
Cordovani L, Cordovani D (2016) A literature review on observational learning for medical motor skills and anesthesia teaching. Adv Health Sci Educ Theor Pract. Netherlands 21(5):1113–1121. https://doi.org/10.1007/s10459-015-9646-5
Wulf G, Shea CH (2002) Principles derived from the study of simple skills do not generalize to complex skill learning. Psychon Bull Rev 9(2):185–211. https://doi.org/10.3758/bf03196276
Korovin LN, Farrell TM, Hsu CH, White M, Ghaderi I (2020) Surgeons’ expertise during critical event in laparoscopic cholecystectomy: an expert-novice comparison using protocol analysis. Am J Surg 219(2):340–345. https://doi.org/10.1016/j.amjsurg.2018.12.024
Funding
This study was funded by Dong-A University Research Fund
Author information
Authors and Affiliations
Contributions
Conceptualization: EJJ. Methodology: EJJ. Formal analysis and investigation: KWK. Writing—original draft preparation: EJJ. Writing—review and editing: KWK. Funding acquisition: EJJ. Approved final script: EJJ, KWK.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jang, E.J., Kim, K. Comparative analysis of robotic single-site cholecystectomy outcomes between novice and expert surgeons. J Robotic Surg 18, 118 (2024). https://doi.org/10.1007/s11701-024-01859-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11701-024-01859-0