Abstract
Robotic surgery has revolutionized surgical procedures and has provided many advantages over traditional laparoscopic and open surgeries. Despite the benefits, there are concerns about the physical discomfort and injuries that may be experienced by surgeons during robotic surgeries. This study aimed to identify the most common muscle groups implicated in robotic surgeons’ physical pain and discomfort. A questionnaire was created and sent to 1000 robotic surgeons worldwide, with a response rate of 30.9%. The questionnaire consisted of thirty-seven multiple-choice questions, three short answer questions, and one multiple-option question pertaining to the surgeon’s workload as well as their level of discomfort while and after performing surgery. The primary endpoint was to identify the most common muscle groups implicated in robotic surgeons’ physical pain and discomfort. Secondary endpoints were to highlight any correlation between age group, BMI, hours of operation, workout regimen, and significant pain levels. The results showed that the most common muscle groups implicated in physical pain and discomfort were the neck, shoulders, and back, with many of the surgeons attributing their muscular fatigue and discomfort to the ergonomic design of the surgeon console. Despite the level of surgeon comfort the robotic console provides when compared to other conventional forms of surgery, the findings suggest the need for better ergonomic practices during robotic surgeries to minimize physical discomfort and injuries for surgeons.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The first robotic surgery was performed in 1985 when the evolution of surgical technique heralded a new era in surgery far greater than ever before. The implementation of robotics in surgery has allowed surgeons to drive a dramatic transition in surgical methods/methodology and augment the number of favorable outcomes [1]. The precision and flexibility that robotic technologies provide result in optimal outcomes for the patient while maximizing surgeon comfort. When compared to laparoscopic and open surgery, robotic surgery provides more accurate visualization using a three-dimensional and magnified stereoscopic display. It also provides more precision due to its protruding instruments and motion scaling abilities, not to mention the clear recovery benefits to the patients while minimizing complication rates [2]. It was also believed that the implementation of robotics in surgery would improve the ergonomics in minimally invasive surgery [2]. The seated position of the surgeon has dramatically impacted surgeon comfort during surgery and has been reported to not only increase surgeon longevity but also reduce surgery-associated injuries to the surgeon [2].
Surgeon injury from repetitive surgical maneuvers is commonly reported in laparoscopic surgery [3], along with injuries to the cervical spine, shoulder, and knee due to the standing position in open and laparoscopic surgery. However robotic surgery, though less physically demanding compared to laparoscopic surgery [4], can still pose different kinds of surgical ailments in the long run [4, 5]. Though over time, robotic surgery has proven to be a more efficient and precise procedure [5], it may also create detrimental damage to the surgeon’s physical health.
In the current literature, there is little published data correlating robotic surgery to specific muscle group injuries. Testimonials from numerous robotic surgeons have bolstered such opinions, but questions regarding the negative impacts of robotic surgery on physicians are yet to be answered. Thus, it is crucial to investigate the potential physical discomfort inflicted on the surgeon. Accordingly, we described a questionnaire-based survey on surgeon reports documenting their fatigue levels, physical discomfort, and areas of injuries performed across a vast array of surgical specialties while using the DaVinci robot.
Methodology
Literature search
A literature search on PubMed was conducted to obtain previous studies of physical discomfort reported by robotic surgeons as well as a correlation or comparison between injuries experienced by open or minimally invasive surgeons. Though most of the topic-related articles did not focus solely on robotic surgery, we were able to focus our search on previously identified areas of pain pertaining to robotic surgeons and identify patterns throughout the literature. First, we searched key terms such as “Robotic-assisted surgery” and “Ergonomic analysis”. Then after generating several comparative articles, we focused our search using “surgeon injury” and “muscular fatigue”.
Questionnaire details
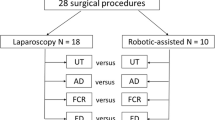
We created a questionnaire through Google forms that consisted of thirty-seven multiple-choice questions, three short answer questions, and one multiple-option question (Tables 1, 2, 3, 4, 5, 6). This questionnaire was reviewed by expert robotic surgeons (VP, MCM) before being sent out to 1000 robotic surgeons working in different medical centers worldwide, in several specialties, with different levels of expertise ranging from novice to expert. We received 309 responses (30.9% response rate). Figure 1 illustrates our survey process.
After gathering the data, each questionnaire was reviewed by robotic surgeons to identify pertinent correlations. Each response given was considered along with the responder’s demographics, experience level, and existence of previous medical conditions. Consequently, we were able to generate charts representing the frequency of muscle discomfort experienced by each surgeon (Figs. 2, 3, 4, 5, 6).
Endpoints
The primary endpoint was to identify the most common muscle groups implicated in robotic surgeons’ physical pain and discomfort. Secondary endpoints were to highlight any correlation between age group, BMI, hours of operation, workout regimen, and significant pain levels.
Results
Demographics
Table 1 and Fig. 2 illustrate the questions for this topic. Overall, we received 309 forms from surgeons practicing in 39 different countries, with multiple medical centers represented in some countries. We received the largest number of responses from the United States and Brazil to our questionnaire. Most surgeons were older than 41 years old, with the largest group being in the 41–45 age group. In terms of BMI, we found that an overwhelming proportion of surgeons are between 21 and 30. Most of the surgeons surveyed were urologists and male.
Surgeon experience
Table 2 and Fig. 3 illustrate the questions for this topic. Many of their surgeries are performed robotically. Most of the surveyed surgeons have been practicing robotic surgery for a minimum of 3 years but almost a third of the respondents have been practicing for > 10 years (31.5%). Most of the Surgeons complete between 1–6 robotic surgeries each week, with very few completing more than 20. On operative days, most surgeons spend between 1–6 h on the console operating. Only 8.2% spend more than 8 h operating. The number of surgeries performed by each surgeon over their career is very diverse, with an almost even spread between 50 and 2500 cases.
Ergonomics
Table 3 and Fig. 4 illustrate the questions for this topic. Most of the surgeons use a chair with arms to operate (> 60%) with the alternative method being a stool. Even though the chair does provide back and arm support, a large proportion of surgeons responded they do not use either of them (42.7%), with only 26.9% using back support. Half of the surgeons reported wearing glasses but most of them do not report headaches after surgery. Most surgeons also report sitting straight with relaxed shoulders while operating, with a large proportion reporting that they do not have to readjust their position during surgery. Many also report re-adjusting the robot arms quite frequently during the surgery using the clutch. Most surgeons report having their console view straight forward or sometimes tilted downwards while operating, however, the majority report that they must tilt their head downwards while operating.
Discomfort
Table 4 and Fig. 5 illustrate the questions for this topic, which was our primary endpoint. Most responses identified muscles of the neck and upper back as the most common sources of pain after robotic surgery. The next two most common muscle groups affected are the lumbar muscles as well as muscles of the finger. Most of the discomfort reported ranged from 1–5/10 on a subjective pain severity scale with only 15% of the surgeons reporting pain ≥ 6/10.
Pain relieving and preventing mechanisms
Table 5 and Fig. 6 illustrate the questions for this topic. Most surgeons (> 75%) report occasional or no stretching whatsoever after performing a case, but if they were to stretch, they mostly focused on the neck, shoulders, and lumbar muscles, where they reported the most pain. Interestingly, approximately 70% of surgeons report minimal to no exercise at the end of their surgical day, despite admitting that either stretching or exercise does help relieve their discomfort from surgery. To gauge objectively the extent of the discomfort, we asked if the surgeons required medical or physical therapy for their pain to which most of them replied no but if they were to require some form of pain-relieving mechanisms, the most common methods would be massages and analgesic medications.
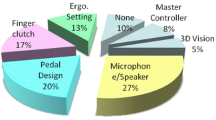
Surgeon suggestions
Table 6 and Fig. 6 illustrate the questions for this topic. Most surgeons conveyed that they believe the main cause of their discomfort, during and immediately after surgery, is the ergonomics of the robot, and more specifically the viewer and the seat used. Many of these surgeons could be receptive to changing the way they practice if there was a method to prevent discomfort while operating.
As part of our secondary outcome, we noticed that a slightly higher number of surgeons who are overweight (BMI: 26–30) reported a higher rating on the subjective pain scale when compared to surgeons with a normal BMI (21–25). Surgeons who never or sometimes stretch after a case and exercise have a noticeably higher rating on their subjective pain scale than surgeons who do so more frequently. Remarkably, surgeons who spend 2–4 h on the console on an operative day have a noticeably higher rating on their subjective pain scale when compared to surgeons who spend 1–2 or 6–8 h a day. Surgeons who believe that the ergonomics of the robot is the main cause of their pain have a noticeably higher rating on their subjective pain scale.
Discussion
The delicate nature of surgery and its inherent risks compels constant optimization of technique and environment. Achieving an optimal working environment for the surgeon is essential for optimizing outcomes. The ergonomics of the robotic console seem to cause the most discomfort in the shoulders and neck muscles as we would have expected. We found that the shoulders and upper cervical spine area are the most commonly reported surgical pain sites (38.4% and 57.8% respectively). This result is similar to what Al-Sabah et al. demonstrated in a web-based survey [6]. Most laparoscopic and robotic bariatric surgeons reported that the most common site of discomfort is the shoulders followed by the back and neck. Furthermore, the neck was seen more pronouncedly in the robotic surgeon group, however, the number of robotic surgeons surveyed was modest (26/113). Incorporating the robot as part of surgical procedures seems to be geared towards optimizing surgeon comfort [7, 8]. When compared to open and laparoscopic surgery, surgeons report less pain when operating on a robotic console [8]. McDonald et al. however, reported in a survey-based study to evaluate physician pain in minimally invasive gynecologic oncology surgery, that using the robot, as well as being a part of the female sex, appeared to be risk factors for experiencing physical pain [9]. Despite that, we do not have a truly objective assessment of its efficacy in alleviating physical pain and maintaining surgeon career longevity.
Although more surgeons performed the surgery while using a chair, our results showed no real difference on the subjective pain scale when comparing surgeons who use a chair to those who use a stool when operating. Dalager et al. studied the muscular load while performing robotic surgery using an ergonomically designed chair versus regular office chair [10]. It was an observational study where they integrated surgeon-answered questionnaires, EMG studies, and postural observation using a validated assessment worksheet to assess the difference in workload on different chairs. They were not able to find any significant difference between the chair ergonomics which they attributed to the inherent complexity of robotic surgery, where it overshadows any focus on the effect of the seat. This further emphasizes the fact that the design of the console should be the focus of ergonomics rather than the seat. Despite robotic surgery being deemed less physically demanding than laparoscopic surgery [7], the long hours required to complete the surgery inevitably take a toll on the surgeon.
Another hypothesis is that the lack of tactile feedback can cause the surgeon to unconsciously apply excessive force to the manipulators, especially during suture handling, since there is no locking mechanism on the robot [2]. This could explain some wrist and forearm pain experienced by some of the surgeons in our questionnaire group. Among the surgeons who complained of wrist and finger pain, twice as many reported frequent clutching to recenter their position. This was further emphasized in a survey-based study by Plerhoples et al. where they reported less physical discomfort, but more thumb and eye pain when surgeons operate using a robot [11]. A proposed remedy to this predicament is formal ergonomics training.
Many surgeons do not receive proper instruction during their training about correct ergonomics and posture while using the robot. Most of them suffice with informal discussions with colleagues and mentors on their preferred form [12]. Franasiak et al. conducted a survey to assess the degree of reception by surgeons about formal ergonomic training. 19 surgeons out of 42 surveyed reported strain specifically related to robotic surgery. After those 19 received formal ergonomic training, 14 reported decreased strain and all of them felt that the training was essential [12]. A literature review on the ergonomics of robotic surgery performed by Wee et al further highlighted this point [13]. Many of the surgeons in our study answered that they frequently had to either readjust their posture or use the clutch to readjust the arms. This is an indicator of prominent discomfort with the working environment provided by the console to the surgeon, which could be reduced with formal ergonomic training.
Finally, our study is not devoid of limitations. Being a questionnaire-based study, it is subjective to the assessment method and has increased chances of recall bias. Furthermore, due to the restricted access to new platforms by most centers, our study intentionally focused on one type of robot (Da Vinci Surgical System) and did not consider these other robots with a different ergonomic design. However, to the best of our knowledge, this is the first study accessing the surgeon’s demographic and ergonomic perception, including several different specialties in robotic surgery.
Conclusion
Despite the robotic surgery ergonomics improvement and intraoperative surgeon comfort when compared to laparoscopic and open surgery, it is still a significant factor contributing to physical pain in surgeons. We described some factors that may be related to these issues, and the robot ergonomics as well as the surgeon seat seem to be the most prominent causative factor. In this scenario, we believe that our data was crucial to understanding that every surgical approach has a different impact on the surgeon’s health, longevity and ultimately patient outcomes.
References
Thai MT, Phan PT, Hoang TT, Wong S, Lovell NH, Do TN (2020) Advanced intelligent systems for surgical robotics. Adv Intell Syst 2(8):1900138. https://doi.org/10.1002/aisy.201900138
Lee GI, Lee MR, Green I, Allaf M, Marohn MR (2017) Surgeons’ physical discomfort and symptoms during robotic surgery: a comprehensive ergonomic survey study. Surg Endosc 31(4):1697–1706. https://doi.org/10.1007/s00464-016-5160-y
Nguyen NT, Ho HS, Smith WD et al (2001) An ergonomic evaluation of surgeons’ axial skeletal and upper extremity movements during laparoscopic and open surgery. Am J Surg 182(6):720–724. https://doi.org/10.1016/S0002-9610(01)00801-7
Dalager T, Søgaard K, Bech KT, Mogensen O, Jensen PT (2017) Musculoskeletal pain among surgeons performing minimally invasive surgery: a systematic review. Surg Endosc 31(2):516–526. https://doi.org/10.1007/s00464-016-5020-9
Cheng SC, Chao YK (2022) Editorial perspective: robot-assisted evaluation of robotic surgical skills. Ann Surg Oncol 29(11):6524–6525. https://doi.org/10.1245/s10434-022-12062-6
AlSabah S, Al Haddad E, Khwaja H (2019) The prevalence of musculoskeletal injuries in bariatric surgeons. Surg Endosc 33(6):1818–1827. https://doi.org/10.1007/s00464-018-6460-1
Lee GI, Lee MR, Clanton T, Sutton E, Park AE, Marohn MR (2014) Comparative assessment of physical and cognitive ergonomics associated with robotic and traditional laparoscopic surgeries. Surg Endosc 28(2):456–465. https://doi.org/10.1007/s00464-013-3213-z
Craven R, Franasiak J, Mosaly P, Gehrig PA (2013) Ergonomic deficits in robotic gynecologic oncology surgery: a need for intervention. J Minim Invasive Gynecol 20(5):648–655. https://doi.org/10.1016/j.jmig.2013.04.008
McDonald ME, Ramirez PT, Munsell MF et al (2014) Physician pain and discomfort during minimally invasive gynecologic cancer surgery. Gynecol Oncol 134(2):243–247. https://doi.org/10.1016/j.ygyno.2014.05.019
Dalager T, Jensen PT, Winther TS et al (2019) Surgeons’ muscle load during robotic-assisted laparoscopy performed with a regular office chair and the preferred of two ergonomic chairs: a pilot study. Appl Ergon 78:286–292. https://doi.org/10.1016/j.apergo.2018.03.016
Plerhoples TA, Hernandez-Boussard T, Wren SM (2012) The aching surgeon: a survey of physical discomfort and symptoms following open, laparoscopic, and robotic surgery. J Robot Surg 6(1):65–72. https://doi.org/10.1007/s11701-011-0330-3
Franasiak J, Craven R, Mosaly P, Gehrig PA (2014) Feasibility and acceptance of a robotic surgery ergonomic training program. JSLS 18(4):e2014.00166. https://doi.org/10.4293/JSLS.2014.00166
Wee IJY, Kuo L, Ngu JC (2020) A systematic review of the true benefit of robotic surgery: ergonomics. Int J Med Robot. https://doi.org/10.1002/rcs.2113
Funding
The authors have not disclosed any funding.
Author information
Authors and Affiliations
Contributions
Ela Patel and Anya Mascarenhas questionnaire design and manuscript writing Shady saikali manuscript writing and supervision of questionnaire Marcio Moschovas and Vipul Patel review of paper, questionnaire and professional opinion.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Patel, E., Saikali, S., Mascarenhas, A. et al. Muscle fatigue and physical discomfort reported by surgeons performing robotic-assisted surgery: a multinational survey. J Robotic Surg 17, 2009–2018 (2023). https://doi.org/10.1007/s11701-023-01608-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-023-01608-9