Abstract
We aimed to compare surgical, oncological, and functional outcomes of robot-assisted radical prostatectomy (RARP) in prostate cancer patients with and without prior history of transurethral resection of the prostate (TURP), using a matched cohort analysis. In an IRB-approved protocol, all patients who underwent RARP at our institution between April 2005 and July 2018 with at least 1-year follow-up were included. Among these, patients who had undergone a previous TURP (Group A) were compared with those without TURP (Group B) using the Survival, Continence, and Potency outcomes reporting system. Using propensity score matching for age, PSA and Gleason score, the two cohorts were further subdivided in a 1:2 ratio into Group C (prior TURP from Group A) and Group D (without prior TURP from Group B). Similar comparisons were made between Group C and D. Patients in Group A (n = 40) had lower PSA (p = 0.031) and were more likely to have Gleason grade 1 disease (p = 0.035) than patients in Group B (n = 143). In the propensity-matched group analysis, patients of Group C (n = 38) had higher operative time and blood loss than Group D (n = 76) patients. Group C patients also had lower continence at 3, 6, and 12 months after surgery. However, oncological and potency outcomes were similar in both the groups. We concluded that previous TURP is a predictor for surgical and continence outcomes following RARP. Even though these patients have a potentially lower stage or grade of disease, they are less likely to achieve social continence than men who have not had a previous TURP. This information would be important in counseling them for treatment options.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Robot-assisted radical prostatectomy (RARP) is the standard of care for the management of localized prostate cancer [1]. Considering the same population also suffers from benign prostatic hyperplasia (BPH), it is not uncommon for patients with prostate cancer to have a history of previous transurethral resection of the prostate (TURP) or of being diagnosed with prostate cancer incidentally on TURP chips [2]. With increasing experience and proven efficacy of RARP, more complex cases like prostate cancer with prior history of TURP have been managed with robotic surgery [3]. Outcomes of RARP in men with prior TURP are variable [4,5,6]. Standardizing the reporting of outcomes is an important aspect of assessing results and the Survival, Continence, and Potency (SCP) system assesses three domains of oncological outcome and biochemical disease-free survival, continence, and potency. [7].
In regions where PSA screening is not routine, it is not uncommon to see post-TURP patients for RARP. Many of these patients have a low-risk disease but seek definitive intervention. Considering the duality of low-risk disease but a potentially higher risk of complications post-TURP, clear knowledge of SCP outcomes after TURP would be useful in providing accurate advice and prognosis to these patients. Few studies have tried to compare the outcomes of RARP with and without prior history of TURP [2,3,4,5]. However, systematic assessment of the oncological and functional outcomes is limited. Difference in baseline characteristics, heterogeneity in surgical approach, variable definitions and non-standardized reporting of outcomes including definitions of disease persistence or recurrence, continence and potency limit the current evidence [2,3,4,5,6]. In this study, we report the operative, oncological, and functional outcomes in patients of localized prostate cancer undergoing RARP, with or without a history of previous TURP, using propensity score-matched cohort analysis. The use of SCP terminology [7] to capture all the domains of trifecta outcomes systematically and the propensity score-matching helped in elimination of selection and reporting bias.
Materials and methods
In an IRB-approved study (IRB number: IECPG-402/30.08.2018), all patients who underwent RARP at our institution between April 2005 and July 2018 and completed at least 2-year follow-up were retrospectively identified from hospital records. All patients were contacted and invited to visit the hospital for follow-up. If a patient had died, the time and cause of death were ascertained through records or a verbal autopsy, and these patients were excluded from the study. Patients were considered lost to follow-up if they could not be contacted or if no follow-up information was available.
RARP was performed a minimum of 6 weeks after biopsy and 12 weeks after TURP. The modified Vattikuti Institute prostatectomy technique was used in most cases with some operated using the extraperitoneal and posterior-first approaches [8].
During the study-specific follow-up visit, information regarding biochemical recurrence and functional outcomes was obtained [7]. Patients with PSA > 0.1 ng/ml at first follow-up, i.e., 6 weeks after surgery was defined as disease persistence [10]. Biochemical recurrence was defined as PSA > 0.2 ng/ml. Survival outcomes (S) were recorded as patients treated with adjuvant therapies (Sx), patients without PSA recurrence (S0), and patients with PSA failure (S1) [7]. Continence outcomes (C) were recorded as patients not using a pad (C0- Total Continence), patients using one pad for security (C1), and patients using ≥ 1 pad (C2). Patients who were incontinent before surgery were marked Cx. Social continence was defined as the use of no pads or up to one safety pad (C0/C1) per day [7].
For assessment of potency (P), English or validated Hindi version of the abridged five-item of the International Index of Erectile Function (IIEF-5) questionnaire was used [9]. As per the SCP criteria [7], potency (P) was assessed as patients not sexually active preoperatively (Px), potent (IIEF-5 score > 17) without any aids (P0), potent (IIEF-5 score > 17) with erectile aids (P1), or impotent (IIEF-5 score < 17) (P2).
All patients were categorized into those with previous TURP (Group A) and those without TURP (Group B). Using 1:2 propensity score match analysis, patients of Group A were matched with patients of Group B in age, preoperative PSA, and preoperative histopathological grade of the disease. The two groups were compared for operative parameters, oncological and functional outcomes.
Statistical analysis
Continuous variables were expressed as mean ± standard deviation (SD) or median (Interquartile range [IQR]) as appropriate. Categorical variables were compared using the Chi-square test and continuous variables were compared using Student’s t-test, multiple ANOVA, Mann–Whitney test, or Kruskal–Wallis test as appropriate. Owing to inherent differences between patients with and without prior TURP in terms of baseline patient and disease characteristics, 1:2 propensity score matching was done to reduce this customary bias. Propensity score was calculated for each patient using multivariable logistic regression model based on age, PSA and preoperative Gleason Grade. A 1:2 matching was used for optimal estimation of treatment effect with improved precision. Subgroup analysis was then performed.
All statistical tests were two-sided. Statistical significance was taken as p < 0.05. Data were analyzed using IBM SPSS Statistics software (version 20.0, Chicago. IL, USA). The authors confirm the availability of and access to all data reported in this study.
Results
Four hundred and forty-seven patients underwent RARP during the study period and 401 of them completed a minimum of 24 months of follow-up. Among these 401 patients, 32 patients died and were excluded from the study. Among remaining 369 patients, 183 patients (49.6%) patients could be followed up and provided the information required for this study and were included. The remaining patients could not be followed up or contacted. Of these 183 patients, 40 patients had undergone a previous TURP (Group A) while Group B included the remaining 143 patients. The mean age of patients was 64.3 ± 5.9 years. Among the 40 patients with prior TURP, the median (IQR) duration between TURP and RARP was 4 (3–94) months. Twenty-two (55%) of them were diagnosed with carcinoma prostate on TURP chips (clinical stage T1b). When compared with patients in Group B, patients in Group A had lower baseline PSA (median 8.2 vs 12.2 ng/dl, p = 0.010), had fewer patients with PSA > 20 ng/ml (17.5% vs 22.5% p = 0.028), and had fewer patients with Gleason Grade Group 3 or higher disease (4.6% vs 18.2%, p = 0.068) (Table 1). However, the mean operative time, blood loss, and need for bladder neck reconstruction were all significantly higher in Group A (Table 1). Similarly, the duration of urinary catheter drainage and major complications (Clavien–Dindo grade III or more) were significantly higher in Group A. The rate of positive surgical margins (PSM) was similar in both groups (20% in Group A vs 21% in Group B, p = 0.457).
Using the propensity score match analysis, 38 patients in Group A (Group C) were compared to 76 patients (Group D), who were matched from among patients in Group B. The mean age, median PSA, and the preoperative Gleason Grade Group were similar in the two groups (Table 2). Group C had significantly longer operative time (mean = 203.7 ± 44.7 vs. 179.9 ± 54.3 min, p = 0.022), greater blood loss (median 325 vs 225 ml, p = 0.032) and need of bladder neck reconstruction (21.1% vs 6.6%, p = 0.027) (Table 2). Among the complications, 7.9% had major complications (Grade III or more) in Group C as compared to 2.6% in Group D (p = 0.098). Though the mean hospital stay was similar, the mean duration for urinary catheter was higher in Group C (p = 0.007) (Table 2).
Oncological outcomes were similar in both groups. The PSM rates were similar (Table 2). Disease persistence (PSA > 0.1 ng/ml) occurred in 3 patients in Group C and they received adjuvant therapy (Sx) compared with 6 patients in Group D, of whom 4 received adjuvant therapy (Sx) (p = 0.712). Biochemical recurrence (BCR) [S1] occurred in 5.2% of patients in Group C compared to 15.8% in Group D (p = 0.104). The median time to BCR was 18 months. Nine patients received salvage androgen-deprivation therapy alone while 5 patients received salvage radiation therapy with or without androgen-deprivation therapy.
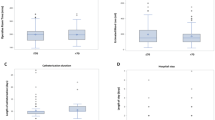
Recovery of continence was significantly lower in Group C as compared to Group D. Table 3 depicts detailed continence outcomes at various time frames in post-operative period as per SCP criteria. In terms of complete continence (C0), early complete continence at 6 weeks was achieved in 26.3% patients in Group D as compared to zero patient Group C (p = 0.001). On a similar trend, 77.6% in Group D attained C0 status at 12 months as compared to 44.7% patients in Group C. Early social continence at 6 weeks was achieved by 18.4% in Group C vs 43.4% in Group D (p = 0.008) and at 3 months in 39.5% vs 85.5% (p = 0.001). The difference remained significant at 1-year follow-up (84.2% vs 97.4%, p = 0.016). However, at 2-year follow-up, social continence rates remained similar in the two groups but complete continence increased to 52.6% in Group C and 85.5% in Group D (p = 0.001) (Table 3). Figure 1a–c depicts the distribution of patients in both the groups with complete continence (C0), using one safety pad (C1) and complete incontinence (C2) at various time frames, respectively.
26.3% of patients were not sexually active at the time of surgery. 18 patients (47.4%) in Group C and 46 patients (60.6%) in Group D were potent with IIEF score > 17. At 1-year follow-up period, 3 patients (16.7%) in Group C versus 3 patients (6.5%) in Group D had normal potency (P0) while 1 patient (5.6%) in Group C and 2 patients (4.3%) had P1 status. At 2-year follow-up, P0 status remained the same, however, 2 patients (11.1%) in Group C and 4 patients (8.7%) in Group D achieved P1 status.
Discussion
BPH and prostate cancer occur in the same population of men. The lack of a uniform PSA screening policy coupled with the wide-spread availability of TURP means that some men diagnosed with prostate cancer have previously undergone a TURP for symptom relief. Further, it is not uncommon to find men who are diagnosed with PCa on histopathological examination of TURP specimen [2, 3]. These men pose two specific problems. The first is that the majority are likely to have low-risk or low-grade incidental disease where the benefits of RARP are not absolute. In such men, it is imperative that if it is decided to perform RARP, the harms be minimized. On the other hand, the previous TURP increases the risk of poor functional outcomes, primarily in the form of incontinence. Unfortunately, both these fears are reinforced by the findings of our study.
We found that patients undergoing RARP following a previous TURP had lower PSA and grade of disease as compared with a matched cohort of patients who had not undergone a previous TURP. Although they had similar oncological outcomes, despite having lower grade disease, these men had poorer operative and functional continence outcomes.
TURP has an impact on intra-operative and perioperative outcomes [11]. Surgical planes may be obscured due to periprostatic inflammation and fibrosis may lead to difficult dissection. The probable cause of this inflammation might be a prostatic infection or capsular perforation and extravasation of the irrigation fluid during TURP. However, RARP is usually performed at least 3 months after TURP and it is expected that the periprostatic inflammation would resolve during this period. The vesicourethral anastomosis might be technically difficult due to rigidity of the bladder neck and loss of elasticity of the urethra. The bladder neck becomes floppy and distorted after prior TURP, thereby, making the identification of prostate-vesical junction as well as ureteric orifice difficult. Moreover, bladder neck reconstruction is often required owing to the wide bladder neck and associated distortion [2, 3].
Martin et al. compared 24 patients undergoing RARP with a prior history of bladder outlet surgery to 486 surgery-naïve patients and reported similar operative time and mean estimated blood loss [12]. Tugcu et al. did a match-pair analysis of 25 patients with previous bladder outlet surgery (20-TURP, 5-open prostatectomy) with 36 patients without prior TURP and reported longer console time, anastomotic time, blood loss, and a higher rate of urinary leakage [13]. On the other hand, Su et al. compared 44 patients undergoing RARP after a prior TURP with 2644 TURP-naïve group and reported similar blood loss and operative time [5]. Similar results were reported by Hung et al. [14]. In a systematic review of patients undergoing radical prostatectomy, patients with prior history of TURP had significantly longer operative time [Weighted Mean Difference (WMD) = 13.2 min], higher blood loss (WMD = 55.3 ml), and higher complication rate [4]. However, there were significant baseline differences in the two groups including smaller prostate volume and low PSA. Moreover, the patients underwent open, laparoscopic, or robot-assisted radical prostatectomy which makes the inference difficult.
The oncological outcome is possibly the most important trifecta outcome measure. Post-inflammatory fibrotic reaction post-TURP, distorted bladder neck anatomy and difficult bladder neck dissection may lead to PSM. Hampton et al. compared 51 patients with prior TURP to 2041 TURP-naïve patients and reported significantly higher PSM rate [12]. The margin positivity was maximum at the bladder apex. Jaffe et al. [15] compared PSM in patients with prior TURP undergoing laparoscopic radical prostatectomy and reported significantly higher PSM rate (21.8% vs 12.6%) in the TURP group. However, other series found a similar PSM rate in patients with prior TURP [5, 6, 14]. In a systematic review [4], there was a significantly higher PSM rate in the TURP group [OR (95% CI) = 1.5(1.09–1.55)]. However, in our matched analysis, we found a similar PSM rate between the previous TURP and TURP-naïve groups. A part of this could be explained by the relatively high number of low-risk patients in our series. The incidence of PSM is directly proportional to the grade and stage of disease [16]. This could also affect the BCR in these patients [16]. Tugcu et al. reported a similar rate of BCR in patients undergoing RARP with or without prior TURP [13]. Hung et al. reported similar BCR at 1-year follow-up, i.e., 18.8% in the TURP group while 11.4% in the TURP-naïve group (p = 0.416) [14]. We also found similar results.
Continence outcome after RARP in patients with the previous TURP is a concerning factor. Su et al. compared the urinary symptoms via American Urological Association (AUA) Symptom Score in patients following RARP and reported worse symptoms by a score difference of 0.71 in the TURP group [5]. In another study, prior TURP was associated with poor early continence rates, i.e., 43.7% vs 68.6% at 3 months (p = 0.06) but similar continence rates at 1 year [6]. Others have reported similar continence rates at 12-month follow-up in the two groups [13, 14]. However, the systematic review [4] reported lower continence rates in patients with prior TURP at 3-month, 6-month, and 12-month follow-up periods. In the subgroup analysis of RARP, the continence rates were similar in the two groups at 3 months and 12-months follow-up period. Inadequate preservation of residual urethral length due to surrounding fibrosis, poor healing of urethrovesical anastomosis due to possible cicatrization and deficient internal sphincter mechanism along with the possible risk of injury to external sphincter during prior TURP are among the possible explanations. Our data reconfirm that continence may be affected adversely in these patients and this remains a significant issue that patients should be informed about.
Potency rates have been variable in studies reporting outcomes of RARP, particularly in patients with prior TURP. Hung et al. reported similar potency rates at 1-year follow-up period in 16 patients with prior TURP and 184 TURP-naïve patients. However, they observed significant difficulty in performing the nerve-sparing technique in patients with prior TURP (23.3%) compared to those without prior TURP (92%) (p = 0.001) [14]. Tugcu et al. and Zugor et al. reported a similar potency rate in the two groups at 1-year follow-up [6, 13].
Unlike previous studies on this subject, our outcomes gain strength from the propensity matching between groups. The complete TURP-naïve cohort (Group B) differed significantly in baseline characteristics from the TURP group and these differences in disease pathology can affect outcomes. Propensity matching made baseline characteristics similar between the two groups. The functional outcomes were recorded by a single observer using standardized tools, thereby, minimizing the observation bias. We assessed disease persistence, need of adjuvant therapy and biochemical failure in oncological outcomes and reported both social continence and complete continence as separate domains of continence. This is the first study to use systematic SCP classification to assess trifecta outcomes in RARP after TURP. Assessment of continence with well-defined terminology of complete continence (C0: no safety pad), one safety pad/day (C1) and more than one safety pad/day (C2) (as defined in SCP classification [7]) along with social continence (upto 1 safety pad/day) at various timepoints after surgery is important as TURP is known to impact continence and a single umbrella definition of continence or incontinence, often used in previous published series [2,3,4,5,6,7, 12,13,14,15], is insufficient to provide accurate prognosis to these patients.
However, the study has certain limitations. The number of patients is relatively small in the TURP group but is somewhat mitigated by comparing it with a similar cohort. The various newer modifications of TURP including laser ablation or laser enucleation could have a variable impact on the outcomes of RARP. This has not been studied as all our patients underwent conventional TURP. Moreover, other factors such as prostate gland size, inherent variations in surgical technique of different surgeons, and an individual’s immune response for inflammation might affect the outcomes of RARP. The histopathology reporting was not done by a single genitourinary pathologist, however, all the reporting was done by experienced pathologists.
Conclusions
Previous TURP is an important predictor for surgical and continence outcomes following RARP. Even though these patients have a potentially lower stage or grade of disease, they are less likely to achieve social or absolute continence than men who have not had a previous TURP. This information would be important in counseling them for treatment options.
Availability of data and material
The authors confirm the availability of and access to all data reported in this study.
Code availability
Appropriate codes were used to maintain patient confidentiality in data management software.
References
Chopra S, Srivastava A, Tewari A (2012) Robotic radical prostatectomy: the new gold standard. Arab J Urol 10(1):23–31
Gupta NP, Singh P, Nayyar R (2011) Outcomes of robot-assisted radical prostatectomy in men with previous transurethral resection of prostate. BJU Int 108(9):1501–1505
Acar Ö, Esen T (2014) Robotic radical prostatectomy in patients with previous prostate surgery and radiotherapy. Prostate Cancer 2014:1–9
Li H, Zhao C, Liu P, Hu J, Yi Z, Chen J et al (2019) Radical prostatectomy after previous transurethral resection of the prostate: a systematic review and meta-analysis. Transl Androl Urol 8(6):712–727
Su Y-K, Katz BF, Sehgal SS, Yu S-JS, Su Y-C, Lightfoot A et al (2015) Does previous transurethral prostate surgery affect oncologic and continence outcomes after RARP? J Robot Surg 9(4):291–297
Zugor V, Labanaris AP, Porres D, Witt JH (2012) Surgical, oncologic, and short-term functional outcomes in patients undergoing robot-assisted prostatectomy after previous transurethral resection of the prostate. J Endourol 26(5):515–519
Ficarra V, Sooriakumaran P, Novara G, Schatloff O, Briganti A, Van der Poel H et al (2012) Systematic review of methods for reporting combined outcomes after radical prostatectomy and proposal of a novel system: the survival, continence, and potency (SCP) classification. Eur Urol 61(3):541–548
Menon M, Tewari A, Peabody JO, Shrivastava A, Kaul S, Bhandari A et al (2004) Vattikuti Institute prostatectomy, a technique of robotic radical prostatectomy for management of localized carcinoma of the prostate: experience of over 1100 cases. Urol Clin N Am 31(4):701–717
Rosen RC, Cappelleri JC, Smith MD, Lipsky J, Peña BM (1999) Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res 11(6):319–326
Bianchi L, Nini A, Bianchi M, Gandaglia G, Fossati N, Suardi N et al (2016) The role of prostate-specific antigen persistence after radical prostatectomy for the prediction of clinical progression and cancer-specific mortality in node-positive prostate cancer patients. Eur Urol 69(6):1142–1148
Colombo R, Naspro R, Salonia A, Montorsi F, Raber M, Suardi N et al (2006) Radical prostatectomy after previous prostate surgery: clinical and functional outcomes. J Urol 176(6):2459–2463
Hampton L, Nelson RA, Satterthwaite R, Wilson T, Crocitto L (2008) Patients with prior TURP undergoing robot-assisted laparoscopic radical prostatectomy have higher positive surgical margin rates. J Robot Surg 2(4):213–216
Tugcu V, Atar A, Sahin S, Kargi T, Gokhan Seker K, IlkerComez Y et al (2015) Robot-assisted radical prostatectomy after previous prostate surgery. JSLS 19(4):e2015.00080
Hung C-F, Yang C-K, Ou Y-C (2014) Robotic assisted laparoscopic radical prostatectomy following transurethral resection of the prostate: perioperative, oncologic and functional outcomes. Prostate Int 2(2):82–89
Jaffe J, Stakhovsky O, Cathelineau X, Barret E, Vallancien G, Rozet F (2007) Surgical outcomes for men undergoing laparoscopic radical prostatectomy after transurethral resection of the prostate. J Urol 178(2):483–487 (discussion 487)
Ficarra V, Novara G, Secco S, D’Elia C, Boscolo-Berto R, Gardiman M et al (2009) Predictors of positive surgical margins after laparoscopic robot assisted radical prostatectomy. J Urol 182(6):2682–2688
Acknowledgements
We acknowledge Ms Anupama Raman, Nursing Officer in-charge of operative records, for helping with the database retrieval.
Funding
No funding or research support has been obtained for this study.
Author information
Authors and Affiliations
Contributions
All the authors have contributed in the research work and preparation of the manuscript as per International Committee of Medical Journal Editors (ICMJE) guidelines. HG: definition of intellectual content, literature search, clinical studies, data acquisition, data analysis, statistical analysis, manuscript preparation, manuscript editing, and manuscript review. AS: concepts, design, definition of intellectual content, literature search, manuscript editing, and manuscript review. RK: concepts, design, definition of intellectual content, literature search, clinical studies, manuscript preparation, manuscript editing, manuscript review, and guarantor (only one).
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interests.
Ethics approval
The study was reviewed and approved by Institute Ethics Review Board (IRB number: IRB number: IECPG-402/30.08.2018).
Consent to participate
An informed written consent was taken from all the patients included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Garg, H., Seth, A. & Kumar, R. Impact of previous transurethral resection of prostate on robot-assisted radical prostatectomy: a matched cohort analysis. J Robotic Surg 16, 1123–1131 (2022). https://doi.org/10.1007/s11701-021-01348-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-021-01348-8