Abstract
In the current opioid crisis, multimodal analgesic protocols should be considered to reduce or eliminate narcotic usage in the postoperative period. We assess the impact of bupivacaine liposome used along with a standard analgesia protocol following robotic inguinal hernia repair. A retrospective review of a prospectively maintained data including robotic inguinal hernia repairs (IHR) by two surgeons in the United States was performed. Within a multimodal analgesic protocol, local anesthetic was administered intraoperatively. One group received a mix of bupivacaine and bupivacaine liposome (BL), and one received standard bupivacaine (SB). Recovery room and home opiate doses were recorded. Primary outcomes included length of stay (LOS) and postoperative medication requirements. Statistical analysis was performed using Chi-square or Fisher’s exact test and Mann–Whitney U test as appropriate. 122 robotic IHRs were included; 55 received BL and 67 received SB. Hospital LOS (hours) was reduced in the BL group (2.8 ± 1.1 vs 3.5 ± 1.2; p = 0.0003). There was no significant difference in recovery room parenteral MME requirements between the groups; however, BL group had less oral MME requirements (5.0 ± 6.5 MME vs. 8.1 ± 6.9 MME, p = 0.02). The BL group had a higher rate of zero opiate doses at home (44% vs 5%, p = 0.0005). Of those that did require opiates at home, there was a significant reduction in number of narcotic pills used by the BL compared to the SB group (median 1 vs 5, respectively; p < 0.0001). Intraoperative administration of BL as part of a pain management protocol may decrease length of hospital stay, and reduce or eliminate the need for narcotic analgesic use at home.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
For decades now, there has been particular interest by both Anesthesiologists and Surgeons in exploring the effects of postoperative narcotic treatment in resulting dependence and long-term use of opiates among postoperative patients. In data reviewed from the 1970s, this was historically a rare consequence, with documented dependence reported in well under 1% of patients who had no history of addiction prior to medical treatment with narcotics [1]. Following this, in the 1990s, the use of opioids substantially increased with a change in expectations regarding pain management, as well as focused pharmaceutical marketing campaigns responding to the Joint Commission on Accreditation of Healthcare Organizations and the American Pain Society’s declaration of pain as the fifth vital sign [2, 3].
Much has changed since then, with the development of the ongoing opioid epidemic, in the recognition, reporting, and treatment of long-term narcotic use after medically necessary analgesia. Today, the reported incidence of persistent opioid use, defined as use beyond the 3-month postoperative mark, has a rate of up to 14% [3, 4]. Over-prescription of narcotic medications after commonly performed operations has been well described [5], and the current paradigm shift is toward minimization of narcotic use in the perioperative setting. Following inguinal hernia repair, for example, evidence comparing opioid utilization has reported that approximately one-third of patients do currently use opioids after hospital discharge [6, 7].
Minimally invasive surgical approaches have also significantly evolved over the last three decades, resulting in improved pain outcomes following common surgical procedures. Besides efforts in minimizing pain from surgical insult, the use of local anesthetics has surfaced as part of a multimodal strategy to mitigate the need for postoperative opiates. Furthermore, the development of liposome bupivacaine as a preparation for prolonged release of the drug by encapsulating it in biodegradable liposomes has been proven to be safe and effective. This formulation has rapid uptake and prolonged release for up to four days post-administration [8], and its benefits compared to standard bupivacaine have been documented in improvement of pain control, decreased risk of urinary retention and postoperative ileus, as well as shortening of hospital length of stay in various surgical settings [9,10,11,12,13].
The purpose of this review is to evaluate the impact of bupivacaine liposome used along with a standard pain-reduction protocol after robotic inguinal hernia repairs, assessing its potential to minimize or completely eliminate narcotic use by patients following these operations.
Materials and methods
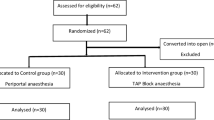
A retrospective review of prospectively maintained data was performed, including ambulatory inguinal hernia repairs (IHR) performed with the assistance of the Da Vinci® Xi robotic platform by two surgeons (OB, CA) between January, 2018 and May, 2019. IHRs were performed in a trans-abdominal, pre-peritoneal (TAPP) approach with a biosynthetic mesh. Patients under chronic pain treatment were excluded from the study. The study was approved by the appropriate Institutional Review Board (IRB); requirement for written informed consent was waived by the IRB, considering the retrospective nature of the study.
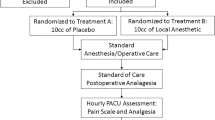
All patients received intravenously one dose of 30 mg ketorolac and one dose of 1 g acetaminophen intraoperatively in addition to general anesthesia. All patients also underwent administration of local anesthetic intraoperatively by the surgeon. One cohort received 10 cc of bupivacaine liposome (BL) mixed 1:1 with 0.25% bupivacaine (total 20 cc) (BL group), and one cohort received 20 cc of 0.25% standard bupivacaine (SB group). Although the two groups were defined secondary to temporal institutional availability of BL, analysis of demographics and preoperative parameters demonstrated no significant differences between the two groups (Table 1). The local anesthetic in both groups was administered as half the volume injected for an inguinal block, and the remainder split locally at the incision sites. Postoperatively, as-needed (PRN) doses of oxycodone, hydromorphone or fentanyl was administered in accordance to the degree of pain reported by the patient in the post-anesthesia care unit (PACU). All patients were educated on this perioperative multimodal pain-reduction protocol with the aim of limiting narcotic use, and were instructed to take acetaminophen and non-steroidal anti-inflammatory drugs (NSAIDs) around the clock for 2 days, and to take prescribed oxycodone as needed only for breakthrough pain at home. Patients were given a prescription for ten tabs of oxycodone 5 mg at time of discharge.
Primary outcomes included length of PACU stay (LOS) in hours from the time the skin is closed to the time the patient was checked out and cleared for discharge by the recovery unit nurse, narcotic usage in PACU, and oxycodone use at home as reported by patients. All PACU medications were converted to Morphine Milligram Equivalents (MME) for both parenteral and oral narcotic medications. Readiness of patient for discharge was determined by routine nursing protocols, not by surgeon input. Although the PACU nursing staff were aware of the local anesthetic provided in the operating room, they were not aware that data points were being collected regarding LOS or narcotic requirement. Secondary outcomes included number of postoperative visits (PV) at 60 days and number of telephone calls (TC) in the postoperative period, excluding the standard postoperative calls made by office staff.
Statistical analyses were performed using Graphpad Prism software version 8.3.0 [GraphPad Software, Inc. La Jolla, CA]. Categorical variables were analyzed using the Chi-square or Fisher’s exact test as appropriate. Continuous variables were analyzed using Mann–Whitney U test. A cutoff of p < 0.05 was used for statistical significance.
This manuscript adheres to the applicable PRISMA guidelines.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee. For this type of retrospective review study, formal consent was waived.
Results
A total of 122 robotic inguinal hernia repairs (IHR) were included. 55 IHR received BL and 67 received SB. Preoperative parameters are listed in Table 1. There was no significant difference between the groups with respect to gender, age, BMI, ASA score, and complexity of the hernia repair.
Postoperative outcomes are listed in Table 2. No significant differences between the groups were noted in operative time, rate of intraoperative or postoperative complications, or number of postoperative visits or patient calls. Hospital LOS (hr) was reduced in the BL group (2.8 ± 1.1 vs 3.5 ± 1.2 h p < 0.05).
Analgesic parameters are listed in Table 3. There was no difference in PACU parenteral MME requirement between the groups (p = 0.84); however, the PACU oral MME requirement was significantly less for the BL group (5.0 ± 6.5 MME vs. 8.1 ± 6.9 MME, p = 0.02) (Fig. 1). For patients that required opiate analgesics at home, there was a significant reduction in number of narcotic tabs used by the patients having received BL compared to SB (median 1 vs 5 tabs, respectively, p = < 0.0001) (Fig. 2). Additionally, a significant difference was noted in the number of patients that did not require any narcotics at home, with 44% of patients in the BL group versus only 15% of patients in the SB group reporting zero opiate doses (p = 0.0005). There was no difference on number of PV or TC.
Discussion
In the present climate combating the opioid epidemic, it is without doubt that the minimization or elimination of postoperative narcotics is an important objective for both Anesthesia and Surgical providers. Current expert guidelines recommend pain management with scheduled non-opiates as first line, and narcotic drug use only for breakthrough pain [5]. Enhanced recovery after surgery (ERAS) pathways and pain-reduction protocols have been implemented to follow common operations, with local anesthetic and non-opiate oral analgesics as the mainstay of pain control efforts. TAP blocks are now commonly performed by surgeons intraoperatively, with results in decreased opioid dose requirements even exceeding the efficacy of epidural analgesia in some reports [14].
Previous literature specifically evaluating inguinal hernia repairs has demonstrated that post-discharge opioid utilization is similar between patients undergoing open, laparoscopic, and robotic repair, as well as unilateral, compared to bilateral repairs [6, 7]. This underscores an important factor in that perhaps the effective use of multimodal pain management strategies is a more critical determinant than the choice of surgical approach, when aiming to minimizing use of opiates at home following inguinal hernia repairs.
To our knowledge, no published studies have evaluated the use of liposomal bupivacaine in robotic inguinal hernia repairs. The use of extended-release formulation anesthetics as part of multimodal pain therapy and ERAS pathways for abdominal wall repairs has been previously described [12], and echoes in our aim to provide local pain control that may eliminate the need for opiate analgesics. Pooled efficacy and safety data support the use of liposome bupivacaine as a means of reducing pain scores and consumption of opioids in inguinal hernia repair and other commonly performed operations [11]. In our analysis, the authors noted no significant difference in the percentage of patients that required administration of narcotic pain medications while in the hospital following the included ambulatory operations. This echoed the findings in a published randomized clinical trial evaluating liposomal bupivacaine as part of an enhanced recovery protocol following minimally invasive surgery demonstrated no significant difference in in-hospital opioid use in patients receiving the liposomal bupivacaine compared with standard bupivacaine [15]. These findings are likely related to nursing protocols with predetermined standards of postoperative narcotic administration regardless of the type of local or regional anesthetic the patients receive. This could present an area of interest in future research studies.
Beyond the immediate period in the recovery room, there is a clear benefit in reduction of opiate use after patients are discharged. In our data, a difference in the number of opiate pills taken at home by all patients was found, and the patients that did not require any narcotic medications after discharge were more likely to have received BL. Particularly for inguinal hernias, these data support the feasibility of opioid-free analgesia after postoperative discharge [4, 16]. In our analysis, nearly 28% of all patients did not require a narcotic prescription at all (Table 3). Similarly, a recent survey of mixed surgical providers reported that up to a third of patients attempted to return unused prescriptions to their surgeons [17], highlighting the providers’ tendency to overprescribe narcotics. This represents an enormous window for improvement in prescription trends for surgeons and surgical trainees. Individual as well as institution-wide initiatives must aim to more appropriately tailor opiate prescriptions. The benefits of such programs have been published. For example, Angelo et al. reported in 2019 a study following implementation of a quality improvement project in patients after common general surgery procedures, including inguinal hernia repair, demonstrating a significant decrease in the prescribed number of narcotic pills prescribed without a resultant increase in number of subsequent ED visits [16]. These findings will direct similar incentives at the authors’ institutions.
Limitations of this study are primarily related to its small size, and its retrospective nature with the inherent limitations of such a review, including reporting bias and missing data. Anatomic variation in hernias adds heterogeneity, which may lead to differences in analgesic needs. Additionally, the authors rely on the self-reported number of medication doses taken by patients post-hospital discharge, which cannot be completely validated.
In conclusion, the addition of bupivacaine liposome to a multimodal pain management protocol in ambulatory robotic inguinal hernia surgery appears to lead to an overall reduction in length of stay, PACU analgesic requirements, and narcotic usage at home in the immediate recovery period. Patients that receive BL are more likely to completely eliminate need for narcotic use at home. Prospective studies with larger sample sizes are needed to further support our findings.
Availability of data and materials
Available upon request.
Code availability
Not applicable.
References
Porter J, Jick H (1980) Addiction rare in patients treated with narcotics. N Engl J Med 302(2):123
DeSnyder SM (2020) Identifying factors predicting long-term opioid use after mastectomy. Ann Surg Oncol. https://doi.org/10.1245/s10434-020-08233-y (Epub ahead of print)
Lanzillotta-Rangeley J, Clark A, Christianson A, Kalarchian MA (2020) Association of prescription opioid exposure and patient factors with prolonged postoperative opioid use in opioid-naïve patients. AANA J 88(1):18–26
El-Kefraoui C, Olleik G, Chay MA et al (2020) Opioid versus opioid-free analgesia after surgical discharge: protocol for a systematic review and meta-analysis. BMJ Open 10(1):e035443. https://doi.org/10.1136/bmjopen-2019-035443
Overton HN, Hanna MN, Bruhn WE, Hutfless S, Bicket MC, Makary MA (2018) Opioid-prescribing guidelines for common surgical prodecures: an expert panel consensus. J Am Coll Surg 227(4):411–418
Knight AW, Habermann EB, Ubl DS, Zielinski MD, Thiels CA (2019) Opioid utilization in minimally invasive versus open inguinal hernia repair. Surgery 166(5):752–757. https://doi.org/10.1016/j.surg.2019.05.012 (Epub 2019 Jun 20)
Sheldon RR, Do WS, Weiss JB, Forte DM, Sohn VY (2019) Sage wisdom or anecdotal dictum? Equivalent opioid use after open, laparoscopic, and robotic inguinal hernia repair. Am J Surg 217(5):839–842. https://doi.org/10.1016/j.amjsurg.2019.02.022 (Epub 2019 Feb 22)
Hu D, Onel E, Singla N, Kramer WG, Hadzic A (2013) Pharmacokinetic profile of liposome bupivacaine injection following a single administration at the surgical site. Clin Drug Investig 33(2):109–115. https://doi.org/10.1007/s40261-012-0043-z
Burnett A, Faley B, Nyirenda T, Bamboat ZM (2018) Liposomal bupivacaine reduces narcotic use and time to flatus in a retrospective cohort of patients who underwent laparotomy. Int J Surg 59:55–60. https://doi.org/10.1016/j.ijsu.2018.09.018
Balocco AL, Van Zundert PGE, Gan SS, Gan TJ, Hadzic A (2018) Extended release bupivacaine formulations for postoperative analgesia: an update. Curr Opin Anaesthesiol 31(5):636–642
Dasta J, Ramamoorthy S, Patou G, Sinatra R (2012) Bupivacaine liposome injectable suspension compared with bupivacaine HCl for the reduction of opioid burden in the postsurgical setting. Curr Med Res Opin 28(10):1609–1615. https://doi.org/10.1185/03007995.2012.721760 (Epub 2012 Sep 3)
Fayezizadeh M, Petro CC, Rosen MJ, Novitsky YW (2014) Enhanced recovery after surgery pathway for abdominal wall reconstruction: pilot study and preliminary outcomes. Plast Reconstr Surg 134(4 Suppl 2):151S-S159. https://doi.org/10.1097/PRS.0000000000000674
Redan JA, Wells T, Reeder S, McCarus SD (2016) Reducing opioid adverse events: a safe way to improve outcomes. Surg Technol Int 28:101–109
Warren JA, Carbonell AM, Jones LK et al (2019) Length of stay and opioid dose requirement with transversus abdominis plane block vs epidural analgesia for ventral hernia repair. J Am Coll Surg 228(4):680–686. https://doi.org/10.1016/j.jamcollsurg.2018.12.017 (Epub 2019 Jan 8)
Ma P, Lloyd A, McGrath M, et al (2019) Efficacy of liposomal bupivacaine versus bupivacaine in port site injections on postoperative pain within enhanced recovery after bariatric surgery program: a randomized clinical trial. Surg Obes Relat Dis 15(9):1554–1562. https://doi.org/10.1016/j.soard.2019.06.004 (Epub 2019 Jun 17)
Angelo JL, Wu J, Sirody J, DeUgarte DA (2019) Reduction in prescribed opioids after general surgery procedures at a public hospital. Am Surg 85(10):1198–1203
Linnaus ME, Sheaffer WW, Ali-Mucheru MN, Velazco CS, Neville M, Gray RJ (2019) The opioid crisis and surgeons: National Survey of Prescribing Patterns and the Influence of Motivators, Experience, and Gender. Am J Surg 217(6):1116–1120. https://doi.org/10.1016/j.amjsurg.2018.11.032 (Epub 2018 Dec 3)
Funding
This project was internally funded.
Author information
Authors and Affiliations
Contributions
MVC, AL, CA, and OB were involved in the conceptualization and data collection. CA and OB performed data analysis. MVC, JS, GD, CA, and OB were responsible for manuscript writing and editing.
Corresponding author
Ethics declarations
Conflict of interest
Cheguevara Afaneh declares that he has received a speaker honorarium from Intuitive Surgical and W.L Gore. Omar Bellorin declares that he has received speaker honorarium from W.L Gore. Mariana Vigiola Cruz, James Senturk, and Gregory Dakin declare that they have no conflict of interest.
Ethical approval
Not applicable.
Informed consent
All procedures followed were in accordance with the Ethical Standards of the Responsible Committee on Human Experimentation (Institutional and National) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
Consent for publication
Patients signed informed consent regarding publishing their data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vigiola Cruz, M., Senturk, J., Dakin, G. et al. Bupivacaine liposome use reduces length of post-anesthesia care unit stay and postoperative narcotic use following robotic inguinal herniorrhaphy. J Robotic Surg 16, 967–971 (2022). https://doi.org/10.1007/s11701-021-01326-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-021-01326-0