Abstract
Robotic pancreaticoduodenectomy has generated significant interest in recent years. Our study aimed to evaluate the difference in surgical, oncological, and survival outcomes after pancreaticoduodenectomy (PD) by either a robotic (RPD) or open approach (OPD). Using the National Cancer Database, we identified patients from 2010 and 2017 diagnosed with pancreatic adenocarcinoma and underwent pancreaticoduodenectomy by either robotic PD or open approach. Patients who underwent robotic PD during 2010 were compared to patients receiving the same procedure in 2017. In addition, a secondary analysis was performed to assess outcomes of robotic PD to open PD for the 2017 patient cohorts. Our primary outcomes included 30-day and 90-day mortality, length of stay, as well as 30-day readmission. Secondary outcome measures were surgical margins, lymph node yield, and adjuvant chemotherapy initiation within 12 weeks of surgery. When we compared the 2017 data to 2010 data, we found that robotic pancreaticoduodenectomy had lower 30- and 90-day mortality rates in 2017 compared to 2010. Additionally, we found that the lymph node yield in robotic PD increased during the study period. When we compared robotic PD to open PD for 2017, we found no statistically significant differences in readmission rates (10.1% vs. 9.7%: p-0.4), lymph node yield, or negative margin between the groups. Outcomes of robotic PD have improved over the years. In 2017, outcomes of robotic PD were similar to open PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There has been a paradigm shift from open to minimally invasive surgery in all surgical specialties [1,2,3]. Studies have shown that complex operations can be performed through a minimally invasive approach with comparable efficacy and safety to open technique, which has led to minimally invasive surgery becoming the standard of care in surgical fields such as urology, and increasingly hepatobiliary surgery [4,5,6]. Society guidelines have framed minimally invasive surgery as the gold standard for specific procedures such as distal pancreatectomy [7, 8].
The role of robotic surgery in pancreaticoduodenectomy (PD) has been of significant debate [9]. The operation is complex and can involve long hours without additional benefits to the patient [10]. Several groups have successfully performed robotic-assisted major pancreatic resections in the past decade, but the literature shows that they have been slow to expand [10, 11]. In 2013, Zureikat et al. demonstrated a relatively higher rate of pancreatic fistulae in patients undergoing robotic PDs than open PDs. Furthermore, they did not find any significant difference in the length of hospital stay [11]. Hence, the benefits of minimally invasive surgery seen in other surgical fields were not reproducible in pancreaticoduodenectomies. However, robotic technology has been improving continuously, and motion control technologies have advanced and have become more precise [12].
The goals of our study are twofold. Our first aim was to assess if perioperative outcomes after robotic pancreaticoduodenectomy are improving. The second aim was to assess if perioperative outcomes are comparable to open pancreaticoduodenectomy.
Methods
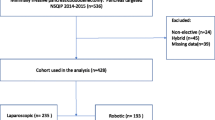
We performed a retrospective analysis of the National Cancer Database base for the years 2010 and 2017. The National Cancer Database is a joint project of the Commission on Cancer of the American College of Surgeons and the American Cancer Society containing Health Insurance Portability, and Accountability Act-compliant deidentified patient data. The database serves as a prospectively collected hospital-based registry that collects data on more than 70% of malignant diagnoses from more than 1,500 Committee on Cancer accredited institutions. We included all patients diagnosed with pancreatic cancer who underwent pancreaticoduodenectomy by either robotic or open approach.
Inclusion and exclusion criteria
We included patients of age 18–90 who underwent pancreaticoduodenectomy for adenocarcinoma of the head of the pancreas. The ICD-O-3 histology codes included in the study were: 8140/3, 8141/3, 8143/3, 8144/3, 8145/3, 8148/3, 8190/3, 8200/3, 8210/3, 8211/3, 8230/3, 8255/3, 8260/3, 8261/3, 8262/3, 8263/3, 8290/3, 8310/3, 8323/3, 8350/3, 8370/3, 8440/3, 441/3, 8450/3, 8470/3, 8471/3, 8480/3, 8481/3, 8482/3, 8490/3, 8500/3, 8503/3, 8504/3, 8510/3, 550/3, 8551/3, 8560/3, 8570/3, 8574/3, 8576/3, and 9015/3). Patients were categorized into two study groups based on the surgical approach—open vs. robotic. Extracted demographic data included: age, gender, hospital academic status, insurance status, comorbidities, and median income. Data from the years 2010 and 2017 were chosen for comparison as they represent the earliest years available in NCDB with coding for robotic pancreaticoduodenectomy, while 2017 was chosen as it is the latest year available in NCDB. Data extracted included data pertinent to the tumor: the stage of the disease, tumor grade, neoadjuvant chemotherapy, adjuvant chemotherapy, and radiotherapy.
We excluded patients ≤ 18-years-old, patients with an unknown surgical approach, or who had a laparoscopic pancreaticoduodenectomy. Additionally, patients with pathologic diagnoses other than pancreatic adenocarcinoma and those missing outcome data were excluded. Finally, patients with additional cancer diagnoses, tumors involving the celiac axis or superior mesenteric artery (T4), distant metastases, and individuals who underwent surgery with palliative intent were excluded.
Outcomes
Our Primary outcomes included 30-day and 90-day mortality, length of stay, as well as 30-day readmission. Secondary outcome measures were surgical margins, lymph node yield, and adjuvant chemotherapy initiation within 12 weeks of surgery. We also assessed for initiation of adjuvant chemotherapy within 12 weeks of surgery which is based on current National Comprehensive Cancer Network guidelines for relevant randomized controlled trials. First, we compared the perioperative outcomes of robotic pancreaticoduodenectomy in 2010 to its perioperative outcomes in 2017. Then, we compared the 2017 perioperative outcomes of robotic PD with the 2017 open PD group to see if the outcomes were similar. We hypothesized that perioperative outcomes of robotic pancreaticoduodenectomy have improved over the years and are now comparable to outcomes of open pancreaticoduodenectomy.
Propensity matching
We utilized propensity score matching in the 1:1 ratio to match the open group with the robotic group for 2017 before comparing their perioperative outcomes. We matched the two groups based on age, gender, comorbidities, race, insurance status, hospital characteristics such as facility type and volume, and tumor characteristics—tumor stage, grade, lymphovascular invasion, and use of neoadjuvant chemotherapy.
Statistical analysis
Statistical analyses were carried out using Statistical Product and Service Solutions (SPSS) version 21.0 software (SPSS Inc., IBM, Armonk, NY). All continuous data were presented as median and mean ± standard deviation (SD), and frequencies were presented when appropriate for the data type. Mean values of continuous variables were compared with a 2-tailed Student's t test. Nonparametric statistical tests were used if the variables did not follow the normal distribution. Categorical variables were presented as percentages. We compared categorical variables using Pearson's χ2 test or Fisher's exact test contingency tables. For all analyses, a p value of ≤ 0.05 was established to determined significance.
Results
We analyzed a total of 4193 patients diagnosed with pancreatic cancer in the years 2010 and 2017. Based on the inclusion and exclusion criteria, 137 patients underwent robotic PD in 2010 and 416 in 2017. There were no statistically significant differences in demographics, insurance status, or median income among patients undergoing robotic PD during the study period. Similarly, the tumor characteristics of patients undergoing robotic PD over the years have remained the same. Table 1 highlights the patient demographics across the two study periods.
Robotic surgery outcomes
When we compared the 2017 data to the 2010 data for robotic pancreaticoduodenectomy. We found that robotic PD had lower 30-day (4.4% vs. 1.2%, p = 0.02) and 90-day (7.3% vs 4.1%, p = 0.03) mortality rates in 2017 compared to 2010. We found that the lymph node yield increased during the study period (16 vs. 20, p < 0.001). We found no statistically significant difference in rates of positive margins between the two groups. The median length of stay for robotic PD improved from 9 days [IQR 7–14] in 2010 to 8 days [IQR 7–13] in 2017 (p-0.01). Table 2 highlights the perioperative outcome differences between the two study periods.
Open vs. robotic PD outcomes
We then sought to compare perioperative outcomes between open PD and robotic PD for the year 2017. In 2017, 1992 patients underwent open PD, while 416 patients underwent robotic PD. Patients who underwent open PD were more likely to have more comorbidities (42.6% vs. 31.2%; p-0.001), be uninsured (4.3% vs. 1.3%; p-0.001) and were more likely to have a higher tumor stage than the robotic counterpart. After propensity score matching, we had 310 patients in both robotic and open PD groups. We found no difference in preoperative characteristics among the two groups after matching. Table 3 highlights the matched and unmatched demographics.
In terms of perioperative outcomes, we found no statistically significant difference in 30-day (1.5% vs. 1.3%, p = 0.4) and 90-day (3.4% vs. 3.3%, p = 0.5) mortality between the open and the robotic group for 2017. There were no differences in readmission rates (10.1% vs. 9.7%: p-0.4). The median length of stay for robotic PD was similar to the open PD group (7 days [IQR 6–9] vs. 8 days [IQR 6–11; p-0.7). There was no difference in the initiation of chemotherapy within 12 weeks of surgery (50.1% vs. 49.8%: p-0.7).
In terms of oncological outcomes, there were no differences in lymph node yield (20 [10–21] vs. 20 [13–27]; p-0.5) and negative margin rates (79.1% vs. 78.1%; p-0.4) between the two groups. Table 4 highlights the perioperative outcome differences between the two study periods. Figure 1 highlights the difference in mortality trends across the study period for Open and Robotic PD.
Discussion
This study highlights improvements in robotic pancreatic surgery perioperative outcomes and shows comparable results to its open counterpart. First, we wanted to investigate if robotic PD outcomes have improved over the years because of the significant learning curve associated with the operation. We found significantly improved perioperative outcomes in 2017 compared to 2010 for robotic PD. Once we demonstrated that robotic PD's perioperative outcomes have improved, we wanted to compare it with the gold standard—open PD. We utilized propensity matching between the open and robotic groups due to the differences in demographics and tumor characteristics. Our study showed similar perioperative outcomes for open and robotic pancreaticoduodenectomy.
For the analyses, we used the years 2010 and 2017. 2010 was the earliest data year available to us from NCDB with granular details about the type of pancreaticoduodenectomy, while 2017 was the latest year available. Therefore, we chose these two points to assess if surgical and oncological efficacy has improved over the years. We chose not to include laparoscopic pancreaticoduodenectomy in the analysis for multiple reasons. First, laparoscopic technology has remained fairly constant, whereas robotic technology has undergone several changes since its inception. Secondly, more centers are now providing robotic technology as it is more adaptable than laparoscopy for pancreaticoduodenectomy and may provide for advantages that are not feasible in laparoscopic surgery. Furthermore, several case series have already reported oncologic outcomes comparable to OPD. [13,14,15]
The robotic approach's impact on more oncologic specific outcomes has also been a topic of much interest. In particular, there has been concern that a robotic approach may compromise oncologic outcomes, including margin status and the number of lymph nodes examined. Our study shows that the rates of R0 resection have remained the same, but lymph node yield has improved. We also see an improved 30 day and 90-day mortality during the study period.
As delays in adjuvant therapy initiation are associated with adverse outcomes, we sought to identify if robotic PD offers any advantage to earlier initiation of chemotherapy [16]. We found that while adjuvant therapy within 12 weeks of resection rates has improved for robotic PD during the study period, the rates are similar to the open group for 2017.
These findings are of utmost significance; it demonstrates improved robotic surgery perioperative outcomes over time and that its outcomes are currently comparable to the gold standard, open PD. This is a critical study because of previous data suggesting higher adverse events associated with robotic PD. In 2013, Zureikat et al. reported their experience with 250 robot-assisted pancreatic surgeries. In their study, 132 robotic PD cases were included, with a morbidity of nearly 62% [11]. In 2015, Chen et al. reported their first experience with robotic PD. They found the overall morbidity to be 35%, concluding that robotic PD did not have many advantages over open PD, and the main benefit of robotic PD was a less surgical burden [17].
Our study found no difference in median overall survival between RPD (21.9 months) and the open pancreatoduodenectomy group. Our findings are similar to a study by Nassour et al., which showed no difference in median overall survival between RPD and open pancreatoduodenectomy groups [18]. Their group has also shown similar results between the two approaches in patients receiving neoadjuvant therapy [19].
Robotic pancreatic surgery is expanding to a great variety of centers nationwide. These findings support the continuation of rigorous training to proliferate qualified robotic pancreatic surgeons. A recent study by Rosemurgy et al. showed that their outcomes of robotic PD were superior to predicted outcomes reported in ACS NSQIP for overall complications, serious complications, returned to the operating room, surgical site infections, deep vein thrombosis, and length of stay [20].
One of the main concerns regarding applying minimally invasive surgery to pancreatic cancer resections is the potential increase in morbidity. A European randomized trial of minimally invasive distal pancreatectomy demonstrated advantages to the minimally invasive approach with reduced time to functional recovery, operative blood loss, and frequency of delayed gastric emptying compared to open distal pancreatectomy [21]. Trials of laparoscopic pancreaticoduodenectomy vs. OPD, however, have shown mixed results with two trials suggesting advantages [22]. A 2010–2011 NCDB study showed an unadjusted 30-day mortality rate was 5.1% for minimally invasive PD versus 3.1% after open surgery. They concluded that minimally invasive PD has higher 30-day mortality then open surgery [23]. However, there has been improvement in outcomes with improvements in technology, increase in volume, and understanding of the learning curves associated with robotic PD. Our study highlights there have been improvements in perioperative mortality along with lymph node yield with robotic PD since 2010. A similar study by Nassour et al. utilized the NCDB and found that over time there have been improvements in mortality and lymphadenectomy with robotic PD with no changes in conversion to open surgery, negative margin resections, or readmissions [18].
This study's limitations include the bias associated with patient selection and the retrospective nature of the research [15]. Unmatched data showed patients with higher comorbidities and higher stages undergoing open PD; therefore, we performed propensity score matching to control biases. However, inherent biases in the data set cannot be controlled by propensity score matching [24, 25]. Lastly, the database available in NCDB in 2017 was more detailed than in 2010 [26]. Hence, we utilized only those accurately recorded variables in 2010 to have a fair comparison. Also, robotic technology has improved since 2017; the findings of this study should be interpreted in this context. As the technology continues to improve, more studies will be needed to assess its efficacy compared to the open approach. Also, details regarding systemic chemotherapy administration, especially on whether individuals were offered yet refused therapy, could not be ascertained. [27, 28] The database does not include specific post-pancreatectomy outcomes such as unplanned reoperations, pancreatic fistula, delayed gastric emptying, or post-pancreatectomy hemorrhage [29]. This does not allow to the identification of the exact etiologies for readmission. Another limitation of the database is that it does not allow for critical operative characteristics such as duration of surgery, estimated blood loss, or concomitant vascular resection and reconstruction involved in the operation [30].
Conclusion
Robotic pancreaticoduodenectomy was associated with similar positive margins and readmission rates as an open pancreaticoduodenectomy. Hence robotic pancreaticoduodenectomy may be considered as a non-inferior option. However, further randomized clinical trials should be designed to assess long-term outcomes and the cost-effectiveness of robotic pancreaticoduodenectomy.
Data availability
Yes, available.
References
Jung M, Morel P, Buehler L, Buchs NC, Hagen ME (2015) Robotic general surgery: current practice, evidence, and perspective. Langenbecks Arch Surg 400(3):283–292. https://doi.org/10.1007/s00423-015-1278-y (Epub 2015 Feb 18; PMID: 25854502)
Aziz H, Zeeshan M, Kaur N, Emamaullee J, Ahearn A, Kulkarni S, Genyk Y, Selby RR, Sheikh MR (2020) A potential role for robotic cholecystectomy in patients with advanced liver disease: analysis of the NSQIP Database. Am Surg 86(4):341–345
Hogen R, Aziz H, Lian T, Genyk Y, Sheikh M (2020) Robotic cystgastrostomy and transgastric pancreatic debridement. J Vis Surg. https://doi.org/10.21037/jovs.2019.12.05
Tan GY, Goel RK, Kaouk JH, Tewari AK (2009) Technological advances in robotic-assisted laparoscopic surgery. Urol Clin N Am 36(2):237–49.ix. https://doi.org/10.1016/j.ucl.2009.02.010 (PMID: 19406324)
Shah MF, Nasir IUI, Parvaiz A (2019) Robotic Surgery for Colorectal Cancer. Visc Med. 35(4):247–250. https://doi.org/10.1159/000500785 (Epub 2019 May 15. PMID: 31602387; PMCID: PMC6738279)
Diaz-Nieto R, Vyas S, Sharma D, Malik H, Fenwick S, Poston G (2020) Robotic surgery for malignant liver disease: a systematic review of oncological and surgical outcomes. Indian J Surg Oncol 11(4):565–572. https://doi.org/10.1007/s13193-019-00945-2 (Epub 2019 Jun 13. PMID: 33281400; PMCID: PMC7714835)
Chan KS, Wang ZK, Syn N, Goh BKP (2021) Learning curve of laparoscopic and robotic pancreas resections: a systematic review. Surgery. https://doi.org/10.1016/j.surg.2020.11.046 (Epub ahead of print. PMID: 33541746)
Asbun HJ, Moekotte AL, Vissers FL et al (2020) The Miami International evidence-based guidelines on minimally invasive pancreas resection. Ann Surg 271(1):1–14
Schwarz JL, Hogg ME (2021) Current state of minimally invasive pancreatic surgery. J Surg Oncol. https://doi.org/10.1002/jso.26412 (Epub ahead of print. PMID: 33559146)
Baker EH, Ross SW, Seshadri R et al (2015) Robotic pancreaticoduodenectomy for pancreatic adenocarcinoma: role in 2014 and beyond. J Gastrointest Oncol 6(4):396–405
Zureikat AH, Moser AJ, Boone BA et al (2013) 250 robotic pancreatic resections: safety and feasibility. Ann Surg 258:554–559 (discussion 559–62)
Aziz H, Shahjehan F, Jie T, Maegawa FB, Zeeshan M, Riall T (2018) Analysis of outcomes of open robotic and laparoscopic pancreaticoduodenectomy using NSQIP. J Pancreas 19(6):291
Nassour I, Choti MA, Porembka MR, Yopp AC, Wang SC, Polanco PM (2018) Robotic-assisted versus laparoscopic pancreaticoduodenectomy: oncological outcomes. Surg Endosc 32(6):2907–2913. https://doi.org/10.1007/s00464-017-6002-2
Cho A, Yamamoto H, Nagata M, Takiguchi N, Shimada H, Kainuma O, Souda H, Gunji H, Miyazaki A, Ikeda A, Tohma T (2009) A totally laparoscopic pylorus-preserving pancreaticoduodenectomy and reconstruction. Surg Today 39:359–362
Pugliese R, Scandroglio I, Sansonna F, Maggioni D, Costanzi A, Citterio D, Ferrari GC, Di Lernia S, Magistro C (2008) Laparoscopic pancreaticoduodenectomy: a retrospective review of 19 cases. Surg Laparosc Endosc Percutan Tech 18:13–18
Merkow RP, Bilimoria KY, Tomlinson JS, Paruch JL, Fleming JB, Talamonti MS et al (2014) Postoperative complications reduce adjuvant chemotherapy use in resectable pancreatic cancer. Ann Surg 260:372–377
Chen S, Chen JZ, Zhan Q et al (2015) Robot-assisted laparoscopic versus open pancreaticoduodenectomy: a prospective, matched, mid-term follow-up study. Surg Endosc 29(12):3698–3711
Nassour I, Winters SB, Hoehn R, Tohme S, Adam MA, Bartlett DL, Lee KK, Paniccia A, Zureikat AH (2020) Long-term oncologic outcomes of robotic and open pancreatectomy in a national cohort of pancreatic adenocarcinoma. J Surg Oncol 122(2):234–242. https://doi.org/10.1002/jso.25958 (Epub 2020 Apr 29 PMID: 32350882)
Nassour I, Tohme S, Hoehn R, Adam MA, Zureikat AH, Alessandro P (2021) Safety and oncologic efficacy of robotic compared to open pancreaticoduodenectomy after neoadjuvant chemotherapy for pancreatic cancer. Surg Endosc 35(5):2248–2254. https://doi.org/10.1007/s00464-020-07638-w
Rosemurgy A, Ross S, Bourdeau T, Craigg D, Spence J, Alvior J, Sucandy I (2019) Robotic pancreaticoduodenectomy is the future: here and now. J Am Coll Surg 228(4):613–624. https://doi.org/10.1016/j.jamcollsurg.2018.12.040 (Epub 2019 Jan 23 PMID: 30682410)
deRooij T, vanHilst J, vanSantvoort H et al (2019) Minimally invasive versus open distal pancreatectomy (LEOPARD): a multicenter patientblinded randomized controlled trial. Ann Surg 269:2–9. https://doi.org/10.1097/sla.0000000000002979
Nickel F, Haney C, Kowalewski K et al (2020) Laparoscopic versus open pancreaticoduodenectomy: a systematic review and meta-analysis of randomized controlled trials. Ann Surg 271:5466. https://doi.org/10.1097/sla.0000000000003309
Adam MA, Choudhury K, Dinan MA et al (2015) Minimally invasive versus open pancreaticoduodenectomy for cancer: practice patterns and short-term outcomes among 7061 patients. Ann Surg 262(2):372–377. https://doi.org/10.1097/sla.0000000000001055
Aziz H, Zeeshan M, Kaur N et al (2020) A potential role for robotic cholecystectomy in patients with advanced liver disease: analysis of the NSQIP Database. Am Surg 86(4):341–345
Aziz H, Hanna K, Lashkari N, Ahmad NU, Genyk Y, Sheikh MR (2021) Hospitalization costs and outcomes of open, laparoscopic, and robotic liver resections. Am Surg. https://doi.org/10.1177/00031348211011063 (published online ahead of print, 2021 Apr 16)
Nickel F, Haney CM, Kowalewski KF, Probst P, Limen EF, Kalkum E, Diener MK, Strobel O, Müller-Stich BP, Hackert T (2020) Laparoscopic versus open pancreaticoduodenectomy: a systematic review and meta-analysis of randomized controlled trials. Ann Surg 271(1):54–66
Hoehn RS, Nassour I, Adam MA, Winters S, Paniccia A, Zureikat AH (2020) National trends in robotic pancreas surgery. J Gastrointest Surg. https://doi.org/10.1007/s11605-020-04591-w (Epub ahead of print. PMID: 32314230)
Sweigert PJ, Wang X, Eguia E et al (2021) Does minimally invasive pancreaticoduodenectomy increase the chance of a textbook oncologic outcome? Surgery. https://doi.org/10.1016/j.surg.2021.02.021 (published online ahead of print, 2021 Mar 16)
Hoehn RS, Nassour I, Adam MA, Winters S, Paniccia A, Zureikat AH (2021) National trends in robotic pancreas surgery. J Gastrointest Surg 25(4):983–990. https://doi.org/10.1007/s11605-020-04591-w
Aziz H, Wang JC, Genyk Y, Sheikh MR (2021) Comprehensive analysis of laparoscopic, robotic, and open hepatectomy outcomes using the nationwide readmissions database. J Robot Surg. https://doi.org/10.1007/s11701-021-01257-w (published online ahead of print, 2021 May 25)
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study design, concept, data analysis, writing the manuscript, and final edits.
Corresponding author
Ethics declarations
Conflict of interest
Drs. Hassan Aziz, Muhammad Khan, Sara Khan, Guillermo P. Serra, Martin D Goodman, Yuri Genyk, Mohd. Raashid Sheikh, have no conflicts of interests to declare. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aziz, H., Khan, M., Khan, S. et al. Assessing the perioperative complications and outcomes of robotic pancreaticoduodenectomy using the National Cancer Database: is it ready for prime time?. J Robotic Surg 16, 687–694 (2022). https://doi.org/10.1007/s11701-021-01296-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-021-01296-3