Abstract
Background
Small intestinal bacterial overgrowth (SIBO) is defined by an increased number of bacteria measured via exhaled hydrogen and/or methane gas following the ingestion of glucose. This condition is prevalent following abdominal surgery, including Roux-en-Y gastric bypass (RYGB), and associated with a variety of non-specific abdominal symptoms, often requiring an extensive diagnostic work-up.
Aim
To assess the frequency that individuals with RYGB anatomy are diagnosed with SIBO and if they are more likely to report specific gastrointestinal (GI) symptoms compared to individuals with native anatomy.
Methods
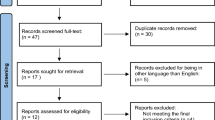
This large matched cohort study evaluated patients with GI symptoms who underwent a glucose breath test (GBT) for SIBO evaluation, utilizing 1:2 matching between RYGB and native anatomy. Patients with positive GBT were included in univariate and multivariate analyses to distinguish the presence of ten specific GI symptoms between RYGB and native anatomy.
Results
A total of 17,973 patients were included, where 271 patients with RYGB were matched to 573 patients with native anatomy that underwent GBT. Patients with RYGB anatomy and a positive GBT (199; 73.4%) as compared to those with native anatomy and a positive GBT (209; 36%) more often reported nausea, vomiting, bloating, and diarrhea. There were no differences between the two groups in the report of heartburn, regurgitation, chest pain, gas, or constipation.
Conclusions
SIBO is common in patients with RYGB and more commonly report nausea, vomiting, bloating, and diarrhea. The results of this study suggest that the report of these symptoms in RYGB should prompt early evaluation for SIBO.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Small intestinal bacterial overgrowth (SIBO) is defined by an increased number of bacteria in the small intestine prompting a variety of gastrointestinal symptoms [1]. SIBO is particularly prevalent following a variety of luminal abdominal surgeries, including Roux-en-Y gastric bypass (RYGB) [2, 3]. The modification of normal gut anatomy may induce bacterial stasis and subsequently precipitate SIBO and other nutritional deficiencies [4,5,6]. SIBO can either be diagnosed by the culturing of small bowel fluid obtained during upper endoscopy or non-invasively by the measurement of exhaled hydrogen and methane following the ingestion of a sugar substrate such as glucose or lactulose [4, 7]. The principle of breath testing is to utilize the fermentation of such simple sugars ordinarily absorbed in the small bowel to indirectly assess bacterial burden within the small bowel. Gases produced by this fermentation include hydrogen, carbon dioxide, and sometimes methane, which are then rapidly absorbed into the blood and ultimately excreted in the exhaled breath via the gas exchange that occurs in the lungs. The abnormal production of hydrogen and/or methane in the breath within a defined time frame following sugar ingestion is then interpreted as that of SIBO [7]. Symptoms of SIBO are known to be widely variable, and may include bloating, flatulence, abdominal discomfort, nausea, or change in bowel habits. Simultaneous measurement of both hydrogen and methane is recommended [7], as positive methane test results have been associated with increased predilection toward constipation [8, 9], which may lead to targeted therapy. The recognition of SIBO is prudent, as the condition has been associated with altered small bowel motility [10], fat malabsorption [11, 12], hypochlorhydria [13], and reversible protein-losing enteropathy [14]. This is particularly salient in the RYGB population, which additionally is at risk for nutritional deficiency [15, 16]. Therefore, prompt recognition and treatment are needed to prevent such metabolic complications.
Following RYGB, up to 30% of patients report perception of recurrent abdominal pain, subsequently interfering with post-surgical quality of life and patient satisfaction [17]. This often triggers an extensive diagnostic evaluation, commonly including breath testing for SIBO [18]. The present study sought to identify whether patients with RYGB anatomy are more likely to manifest certain symptoms of SIBO compared to patients with native anatomy in an effort to help prompt early evaluation of this condition in this patient population.
Materials and Methods
Data Source
This was a matched cohort study using a database collected between January 1989 and December 2017 in patients with gastrointestinal (GI) symptoms who underwent glucose breath test (GBT) for evaluation of SIBO at a single quaternary care institution. Patients presenting for GBT were asked at the time of testing to complete a questionnaire querying the presence or absence of symptoms of heartburn, regurgitation, chest pain, nausea, vomiting, abdominal pain, bloating, gas, diarrhea, and constipation. The University of Michigan Institutional Review Board approved this study under the IRB HUM00135842.
Study Sample
Patients were included if they had a positive GBT (using 50 g glucose dose) which required a rise > 12 parts per million (ppm) in breath hydrogen or methane concentration above baseline within 90 min [19]. Consecutive patients with RYGB anatomy and positive GBT tests were matched 1:2 with patients undergoing GBT with native anatomy found to have positive GBT. Matching factors were applied sequentially: age, body mass index, and diabetes status. Consecutive adult patients with positive GBT and RYGB anatomy were included in the RYGB group (n = 271). Of the patients with positive GBT and native anatomy, randomization was performed using the date of positive GBT category variable to include a total of 573 patients, which allowed for 2:1 matching.
Study Variables
Patient charts were reviewed under the approved institutional review board protocol. Patient demographics collected from the patient data registry included age (assessed as a continuous variable), sex, and body mass index (kg/m2). Information regarding known or suspected risk factors for the development of SIBO (including diabetes status, proton pump inhibitor (PPI) use, and alcohol use) were also collected.
Outcome
The primary outcome of the study included the presence or absence of ten specific gastrointestinal symptoms at the time of GBT were recorded including heartburn, regurgitation, chest pain, nausea, vomiting, abdominal pain, bloating, gas, diarrhea, and constipation.
Statistical Analysis
All statistical analyses were performed using the SAS 9.4 statistical package (SAS Institute, Inc., Cary, NC). The study was approved by the Institutional Review Board before inception. The Fisher exact test for binary variables and the Student t test or Wilcoxon signed-rank test for continuous variables based on normality of the data were applied to assess baseline differences across the RYGB and normal anatomy groups. Univariate and multivariate analyses were performed using chi-square or Fisher’s exact test and logistic regression, respectively. Statistical significance was established using p < 0.05.
Results
A total of 17,973 patients with positive GBT were included in the database. Of these, 271 patients had RYGB anatomy. The mean age of the RYGB cohort was 54.6 ± 0.8 years with a mean body mass index (BMI) of 30.6 ± 1.0 kg/m2. GBT was positive within 90 min in 199 (73.4%) of these patients. Five hundred seventy-three patients with native upper GI anatomy were also identified who were referred for GBT. Of these, 209 (36.5%) were positive for SIBO based on GBT. The mean age of the native positive GBT cohort was 53.5 ± 0.9 years with a mean BMI 27.8 ± 0.9 kg/m2. The percent of female patients was higher in the RYGB group as compared to those with normal anatomy (87.8 vs 68.8, p < 0.001) consistent with prior literature demonstrating a female predominance in patients undergoing bariatric surgery [20]. The groups were otherwise comparable in regard to demographic variables and distribution of potential risk factors leading to the development of SIBO (Table 1). There additionally were no significant differences in the frequency of proton pump inhibitor (PPI) use between the RYGB and native anatomy cohorts, those with positive GBT between cohorts and those with positive vs negative GBT in either the RYGB or native anatomy cohorts.
Among positive breath tests, RYGB patients were significantly more likely to have a positive GBT for SIBO based on hydrogen excretion (H2 only or H2 and CH4) as compared to those with native anatomy (94% vs 79.9%; p < 0.001), with OR of 3.92 (95% CI 2.00, 7.67). Conversely, patients with RYGB anatomy were significantly less likely to have methane only glucose breath tests compared to those with native anatomy (6.0% vs 20.1%; p < 0.001) (Table 2). Mean baseline and post-glucose ingestion hydrogen and methane levels are demonstrated in Table 3. RYGB patients had significantly greater elevations in both hydrogen and methane following glucose ingestion.
Patients with RYGB anatomy as compared to native anatomy more often reported nausea (57.7% vs 48%, p = 0.010), vomiting (33.2% vs 22.3%, p = 0.001), bloating (72.1% vs 62.5%, p = 0.006), and diarrhea (72% vs 59.7%, p < 0.001). There were no differences between groups in report of heartburn, regurgitation, chest pain, gas, or constipation (Table 4). When further stratifying by sex (Table 5), RYGB female patients were significantly more likely to self-report nausea compared to male patients (p = 0.01, OR = 4.00: 95% CI: 1.38, 11.95) and significantly less likely to self-report bloating compared to RYGB male patients (p = 0.02, OR = 0.20: 95% CI: 0.05, 0.75). There were no differences between RYGB female and male patients related to self-reporting vomiting or diarrhea as symptoms.
Discussion/Conclusion
SIBO is a syndrome that may cause diarrhea, abdominal bloating, malabsorption, and anemia. Predisposing factors for developing SIBO include a reduction in gastric acid (e.g., pump inhibitors [21] a post-gastrectomy state [22]), delayed intestinal transit [23] (e.g., diabetes or scleroderma [4, 12]), or surgery resulting in a blind loop [6, 24, 25]. Individuals who present with SIBO-related symptoms and are being considered for weight loss surgery may benefit from pre-operative testing, as SIBO has been shown to be associated with a lower magnitude of weight loss [3].
SIBO appears particularly prevalent following Roux-en-Y gastric bypass (RYGB), considerably more so than those with normal upper GI anatomy suspected of having SIBO based on GBT. Abdominal symptoms are common in patients who have undergone RYGB, often prompting extensive diagnostic work-up [18]. Patient history is therefore an essential component of making a diagnosis, with prioritization of diagnostic studies depending on initial presenting symptoms. Few studies to date have investigated symptoms of SIBO following RYGB, and whether the constellation of symptoms is unique in this patient population. Although jejunal aspiration is the historical gold standard in the diagnosis of SIBO, breath testing has been shown to have an increased sensitivity and specificity in patients who have undergone surgical reconstruction [26]. The frequency of SIBO in patients with RYGB and its role as the cause of symptoms is currently unknown. The present study sought to identify whether patients with RYGB anatomy are more likely to manifest certain symptoms of SIBO compared to patients with native anatomy in an effort to help prompt early evaluation of this condition.
This large study demonstrated RYGB patients with SIBO present significantly more frequently with symptoms of nausea, vomiting, bloating, and diarrhea compared to those with native anatomy. This was in part determined by sex, as females were significantly more likely to report nausea than men, however significantly less likely to report bloating (no difference in vomiting and diarrhea). Although opiate use was also significantly higher in the RYGB population, and may contribute to symptoms such as nausea and delay oral-cecal transit time (OCTT) through constipating mechanisms that would affect breath testing, this may be a small consideration as the significant increase in diarrhea observed in the RYGB population correlates with a significant increase in hydrogen breath testing; methane-predominant breath testing has been associated with constipation [8, 9].
Identifying this myriad of symptoms may lend credence to early SIBO breath testing, particularly in patients that have failed more conservative therapies, including open capsule PPI or sucralfate therapies [18]. It remains important to maintain SIBO within the differential diagnosis in these patients to avoid premature closure in making a diagnosis. Further study is needed to determine whether empiric treatment should be considered in the presence of these symptoms to obviate the need for confirmatory breath testing. This would be further tailored in the RYGB population as these patients were more likely to demonstrate hydrogen predominant positive GBT compared to those with native anatomy, which may be due to increased prevalence of diarrhea (and mildly reduced prevalence of constipation) in this population.
There are several limitations to this study. First, breath testing to diagnose SIBO may be problematic following RYGB, as rapid transit through the small bowel could result in the test substrate (glucose or lactulose) reaching the colon and initiating fermentation by colonic bacteria, leading to an early rise in breath hydrogen that might be falsely attributed to bacteria in the small bowel [27], although notably this carries a greater risk with lactulose as a result of being an osmotic laxative [26], whereas the present study solely evaluated GBT. Second, this is a retrospective study and prospective trials evaluating empiric SIBO management in RYGB patients with nausea, vomiting, bloating or diarrhea would further refine management. Third, the present study evaluated SIBO solely in RYGB surgical patients and further studies are warranted to evaluate the incidence and symptom manifestations of SIBO in alternative bariatric surgeries, including biliopancreatic diversion (DBP) and one anastomosis gastric bypass (OAGB). Fourth, patients may have undergone empiric treatment for SIBO prior to GBT and considering how that may affect symptoms in RYGB and native anatomy patients warrants further study. A final limitation is that the present study includes a comparison between RYGB and native anatomy in individuals with a positive GBT only. A future comparison including two additional groups (groups including RYGB anatomy and native anatomy with negative GBT) would provide further details about symptom constellation differences between groups.
SIBO is prevalent following intestinal surgeries, including Roux-en-Y gastric bypass (RYGB). Symptoms of nausea, vomiting, bloating, and diarrhea are significantly more commonly associated with RYGB anatomy compared to native anatomy and should prompt consideration of SIBO as a potential etiology and subsequent treatment target with antibiotics that have a comparatively safe adverse event profile such as rifaximin, and potentially obviate the need for further invasive testing such as upper endoscopy.
References
Pimentel M, Saad RJ, Long MD, et al. ACG clinical guideline: small intestinal bacterial overgrowth. Am J Gastroenterol. 2020;115(2):165–78. https://doi.org/10.14309/ajg.0000000000000501.
Machado JD, Campos CS, Lopes Dah Silva C, et al. Intestinal bacterial overgrowth after Roux-en-Y gastric bypass. Obes Surg. 2008;18(1):139–43. https://doi.org/10.1007/s11695-007-9365-y.
Sabate JM, Coupaye M, Ledoux S, et al. Consequences of small intestinal bacterial overgrowth in obese patients before and after bariatric surgery. Obes Surg. 2017;27(3):599–605. https://doi.org/10.1007/s11695-016-2343-5.
Bures J, Cyrany J, Kohoutova D, et al. Small intestinal bacterial overgrowth syndrome. World J Gastroenterol. 2010;16(24):2978–90. https://doi.org/10.3748/wjg.v16.i24.2978.
Coupaye M, Riviere P, Breuil MC, et al. Comparison of nutritional status during the first year after sleeve gastrectomy and Roux-en-Y gastric bypass. Obes Surg. 2014;24(2):276–83. https://doi.org/10.1007/s11695-013-1089-6.
Poitou Bernert C, Ciangura C, Coupaye M, et al. Nutritional deficiency after gastric bypass: diagnosis, prevention and treatment. Diabetes Metab. 2007;33(1):13–24. https://doi.org/10.1016/j.diabet.2006.11.004.
Rezaie A, Buresi M, Lembo A, et al. Hydrogen and methane-based breath testing in gastrointestinal disorders: the North American Consensus. Am J Gastroenterol. 2017;112(5):775–84. https://doi.org/10.1038/ajg.2017.46.
Kunkel D, Basseri RJ, Makhani MD, et al. Methane on breath testing is associated with constipation: a systematic review and meta-analysis. Dig Dis Sci. 2011;56(6):1612–8. https://doi.org/10.1007/s10620-011-1590-5.
Hwang L, Low K, Khoshini R, et al. Evaluating breath methane as a diagnostic test for constipation-predominant IBS. Dig Dis Sci. 2010;55(2):398–403. https://doi.org/10.1007/s10620-009-0778-4.
Justus PG, Fernandez A, Martin JL, et al. Altered myoelectric activity in the experimental blind loop syndrome. J Clin Invest. 1983;72(3):1064–71. https://doi.org/10.1172/jci111031.
Donaldson Jr RM. Role of enteric microorganisms in malabsorption. Fed Proc. 1967;26(5):1426–31.
Shindo K, Machida M, Koide K, et al. Deconjugation ability of bacteria isolated from the jejunal fluid of patients with progressive systemic sclerosis and its gastric pH. Hepatogastroenterology. 1998;45(23):1643–50.
Quigley EMM. The spectrum of small intestinal bacterial overgrowth (SIBO). Curr Gastroenterol Rep. 2019;21(1):3. https://doi.org/10.1007/s11894-019-0671-z.
Su J, Smith MB, Rerknimitr R, et al. Small intestine bacterial overgrowth presenting as protein-losing enteropathy. Dig Dis Sci. 1998;43(3):679–81. https://doi.org/10.1023/a:1018848132369.
Gobato RC, Seixas Chaves DF, Chaim EA. Micronutrient and physiologic parameters before and 6 months after RYGB. Surg Obes Relat Dis. 2014;10(5):944–51. https://doi.org/10.1016/j.soard.2014.05.011.
Gesquiere I, Foulon V, Augustijns P, et al. Micronutrient intake, from diet and supplements, and association with status markers in pre- and post-RYGB patients. Clin Nutr. 2017;36(4):1175–81. https://doi.org/10.1016/j.clnu.2016.08.009.
Mala T, Hogestol I. Abdominal pain after Roux-en-Y gastric bypass for morbid obesity. Scand J Surg. 2018;107(4):277–84. https://doi.org/10.1177/1457496918772360.
Schulman AR, Thompson CC. Abdominal pain in the Roux-en-Y gastric bypass patient. Am J Gastroenterol. 2018;113(2):161–6. https://doi.org/10.1038/ajg.2017.361.
Gasbarrini A, Corazza GR, Gasbarrini G, et al. Methodology and indications of H2-breath testing in gastrointestinal diseases: the Rome Consensus Conference. Aliment Pharmacol Ther. 2009;29(Suppl 1):1–49. https://doi.org/10.1111/j.1365-2036.2009.03951.x.
Kizy S, Jahansouz C, Downey MC, et al. National trends in bariatric surgery 2012-2015: demographics, procedure selection, readmissions, and cost. Obes Surg. 2017;27(11):2933–9. https://doi.org/10.1007/s11695-017-2719-1.
Su T, Lai S, Lee A, et al. Meta-analysis: proton pump inhibitors moderately increase the risk of small intestinal bacterial overgrowth. J Gastroenterol. 2018;53(1):27–36. https://doi.org/10.1007/s00535-017-1371-9.
Perez Aisa A, Garcia Gavilan MC, Alcaide Garcia J, et al. Small intestinal bacterial overgrowth is common after gastrectomy but with little impact on nutritional status. Gastroenterol Hepatol. 2019;42(1):1–10. https://doi.org/10.1016/j.gastrohep.2018.07.001.
Roland BC, Ciarleglio MM, Clarke JO, et al. Small intestinal transit time is delayed in small intestinal bacterial overgrowth. J Clin Gastroenterol. 2015;49(7):571–6. https://doi.org/10.1097/mcg.0000000000000257.
Decker GA, DiBaise JK, Leighton JA, et al. Nausea, bloating and abdominal pain in the Roux-en-Y gastric bypass patient: more questions than answers. Obes Surg. 2007;17(11):1529–33. https://doi.org/10.1007/s11695-008-9416-z.
Ledoux S, Calabrese D, Bogard C, et al. Long-term evolution of nutritional deficiencies after gastric bypass: an assessment according to compliance to medical care. Ann Surg. 2014;259(6):1104–10. https://doi.org/10.1097/sla.0000000000000249.
Losurdo G, Leandro G, Ierardi E, et al. Breath tests for the non-invasive diagnosis of small intestinal bacterial overgrowth: a systematic review with meta-analysis. J Neurogastroenterol Motil. 2020;26. Korea (South):16–28.
Jirapinyo P, Makuvire TT, Dong WY, et al. Impact of oral-cecal transit time on the interpretation of lactulose breath tests after RYGB: a personalized approach to the diagnosis of SIBO. Obes Surg. 2019;29(3):771–5. https://doi.org/10.1007/s11695-018-3575-3.
Funding
A.R. Schulman – Apollo Endosurgery (consultant); Boston Scientific (consultant); MicroTech (consultant); GI Dynamics (research, grant support). J.R. Baker – Medtronic (consultant); Diversatek Healthcare (consultant). K. Harer – Alnyam (consultant). R.D. Dolan, A. Lee, R. Saad, and W. Hasler have no personal or financial conflicts of interest to disclose.
Author information
Authors and Affiliations
Contributions
RD: analysis and interpretation of data; drafting of manuscript; critical revision of the manuscript for important intellectual content; approver of final draft submitted
JB: acquisition of data; analysis and interpretation of data; statistical analysis; critical revision of the manuscript for important intellectual content; approver of final draft submitted
KH: critical revision of the manuscript for important intellectual content; approver of final draft submitted
AL: critical revision of the manuscript for important intellectual content; approver of final draft submitted
WH: critical revision of the manuscript for important intellectual content; approver of final draft submitted
AS: study concept and design; acquisition of data; analysis and interpretation of data; critical revision of the manuscript for important intellectual content; approver of final draft submitted
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Conflict of Interest
Russell D. Dolan: No conflicts of interest to report.
Jason Baker: Consultant for Medtronic and Diversatek Healthcare.
Kimberly Harer: Consultant for Alnyam.
Allen Lee: No conflicts of interest to report.
William Hasler: No conflicts of interest to report.
Richard Saad: No conflicts of interest to report.
Allison R. Schulman: Consultant for Apollo Endosurgery, Boston Scientific and MicroTech. Receives research and grant support from GI Dynamics.
Informed Consent
Informed consent does not apply.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Guarantor of the article: Allison R. Schulman, MD, MPH
Rights and permissions
About this article
Cite this article
Dolan, R.D., Baker, J., Harer, K. et al. Small Intestinal Bacterial Overgrowth: Clinical Presentation in Patients with Roux-en-Y Gastric Bypass. OBES SURG 31, 564–569 (2021). https://doi.org/10.1007/s11695-020-05032-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-05032-y