Abstract
Introduction
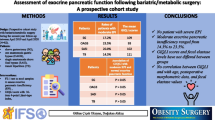
After bariatric surgery (BS), patients might suffer from nutrient maldigestion, malabsorption, and vitamin deficiencies. In this study, our aim was to assess pancreatic functions after BS using fecal elastase-1 assay (FE-1).
Material and Methods
Sixty patients (21M) undergoing BS and 20 (6M) healthy controls were included into the study. Stool samples were collected 1 year after surgery. Ten patients from one anastomosis gastric bypass (OAGB) and single anastomosis duodenal switch (SADS) groups with the lowest value of FE-1 and GIQLI scores were given pancreatic enzyme replacement therapy (PERT). After PERT, FE-1, excess weight loss (EWL), BMI, GIQLI scores, and vitamin D levels were measured.
Results
Vitamin D levels were detected as 19.04 (9–46.5) pg/ml, 15.1 (8.4–23.6) pg/ml, 17.8 (5–30) pg/ml, and 21.79 (11–40.3) pg/ml after sleeve gastrectomy (SG), OAGB, SADS, and control groups, respectively (p = 0.04). GIQLI scores in the first year were found to have increased in all patients (p = 0.02). FE-1 levels were found as 642.35 (566.3–711.4) μg/g, 378.52 (183.5–561.1) μg/g, 458.88 (252.5–593, 5) μg/g, and 518.2 (351.6–691) μg/g for the SG, OAGB, SADS, and control groups, respectively. There was a strong inverse correlation between EWL and FE-1 levels at the end of the first year (Spearman’s rho = − 0.688, p = 0.003). After having performed PERT for patients with the lowest FE-1 levels, the levels increased to 683.39 (615.5–720) μg/g in the OAGB and 691.5 (643.1–720) μg/g in the SADS groups (p = 0.011).
Conclusion
FE-1 measurements demonstrated that many patients suffer from malabsorption after OAGB or SADS, whereas functions remain normal after SG. PERT corrects pancreatic functions without affecting weight loss and also contributes to the normal serum level of vitamin D.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The pancreas is the second largest organ of the digestive system after the liver with exocrine/endocrine functions. While sodium bicarbonate (ductal function) and digestive enzymes are secreted by the exocrine pancreas into the duodenum, the endocrine pancreas secretes many hormones into circulation, especially those that regulate glucose metabolism [1]. The majority of the pancreas consists of exocrine cells while 10% show endocrine cell function. The different cell types it contains have different exocrine and endocrine secretion properties. While exocrine pancreatic enzymes are secreted as a result of cephalic, gastric, and intestinal phases, these phases are regulated by humoral and neuronal control mechanisms [2].
For the digestive functions to start, postprandial pancreatic secretions are allowed following the gastric discharge of acid chymes and are controlled by fundic relaxation, inhibition of antrum motility, and the pyloric motor activity called as duodenogastric reflexes [3]. Cholecystokinin release (CCK), as a response to food in the duodenum, is the main hormone-mediated postprandial stimulation of exocrine pancreatic secretion [4]. CCK hormone stimulates the release of trypsin, amylase, and lipase enzymes from the pancreas. Secretin, a digestive hormone, is secreted by the small intestinal mucosa following the entry of foods into the intestine and stimulates the bicarbonate-rich pancreatic fluid discharge. Deterioration encountered in any process of these mechanisms results in exocrine pancreatic insufficiency (EPI).
Loss of pancreatic functions after surgery depends heavily on the degree of anatomical changes to the stomach, duodenum, and pancreas and reduces the release of some hormones, particularly CCK, playing a major role in digestion [5]. Therefore, any gastric, duodenal, and pancreatic surgery might result in varying degrees of EPI.
EPI is categorized as mild, moderate, and severe. Mild EPI is characterized as decreased secretion of digestive enzymes with an appropriate bicarbonate concentration in the duodenum and regular fecal fat excretion. Moderate EPI is described as having decreased activity of enzymes and concentration of bicarbonate with regular excretion of fecal fat, whereas severe EPI indicates decreased enzyme activity and concentrations of bicarbonate which results in steatorrhea and its clinical signs and symptoms [6]. Patients with EPI may experience symptoms such as steatorrhea, abdominal distension, diarrhea, abdominal pain, and weight loss, and these findings are usually due to maldigestion [7]. However, enzyme levels are expected to fall almost 10% below normal levels, especially for steatorrhea development [8]. Although the clinical diagnosis of EPI can be made on the basis of symptoms in patients with underlying diseases (pancreatitis, cystic fibrosis, pancreatic cancer) or a history of surgical operation, EPI can be diagnosed by specific tests in patients with maldigestion and protein malnutrition but without any obvious symptoms [9].
There are many direct diagnostic methods used to evaluate exocrine functions of the pancreas, and CCK test, secretin test, combined secretin-CCK test, endoscopic pancreatic function test, and Lundh’s test are among of the few. However, in order to perform all these tests, a naso-duodenal tube should be placed, and a partially long-time interval is required to collect the duodenal content with these methods.
In the current clinical practice, the fecal elastase-1 (FE-1) test is the most widely used simple, easy to perform, and patient-friendly test. Unlike other pancreatic enzymes, FE-1 is a pancreas-specific enzyme that passes through the intestines without degradation. A stool sample, single or multiple, is evaluated with human pancreas elastase-specific antibodies with enzyme-linked immunosorbent assay. Studies have demonstrated a good association between the pancreatic discharge of elastase-1 and FE-1 test with relatively reliable cut-off values [10]. When direct pancreatic function tests are taken as a reference, it is seen that the approximate sensitivity of FE-1 for severe, moderate, and mild EPI cases is 100%, 77–100%, and 0–63%, respectively, with around 93% specificities [11]. Previous studies have also shown that FE-1 is more sensitive and specific than fecal chymotrypsin [12].
Bariatric surgery (BS) is the most effective method used in the treatment of morbid obesity today and is classified as restrictive, malabsorptive, or combined procedures. All procedures in BS, based on either anatomical alterations and/or hormonal changes, result in altered pancreatic functions [13]. Gastric resections or altered gastric anatomy and any kind of anastomosis, gastrojejunal or duodenojejunal, in commonly used effective bariatric procedures to achieve weight loss might also result in varying degrees of EPI. Patients with successful weight loss might also suffer from abdominal discomfort and vitamin deficiencies as a result of EPI [14, 15].
Pancreatic enzyme replacement therapy (PERT) is a commonly used method for treating EPI that occurs secondary to systemic diseases, or after gastrointestinal and pancreatic surgery. The main goal of PERT is to reduce the malabsorption of fats and fat-soluble vitamins and the resulting malnutrition [16].
The present study aims to assess exocrine pancreatic functions following different bariatric procedures, including sleeve gastrectomy (SG), one anastomosis gastric bypass (OAGB), and single anastomosis duodenal switch (SADS) using FE-1 assay and to evaluate the effectiveness of PERT in EPI after BS.
Patients and Methods
Subjects
Three hundred (142 males) patients with BMI > 40 kg/m2 and a median (range) age of 39 (19–76) years had undergone successful BS between 2017 and 2019 in our department. One hundred and thirty-seven of them had SG, 114 of them had OAGB, and the remaining had SADS.
As part of our routine, after BS, all patients were given a standard postbariatric diet and multivitamin pills containing iron, folic acid, vitamin D, vitamin B12 (hydroxocobalamin), and calcium citrate once a day. All patients were followed up in the first month, and then every 3 months at the outpatient clinic. Weight, body mass index (BMI), excess weight loss (EWL), Gastrointestinal System Quality of Life Index (GIQLI) scores, and vitamin D levels of the patients were measured and registered during the follow-up.
Patients with diabetes or history of any known causes of EPI (such as pancreatitis, pancreatic resections, and previous upper gastrointestinal surgery) or those already using PERT were excluded from the study.
After having received ethical approval (approved by the Committee on Institutional Ethics of Liv Hospital Ankara, 2017/1-006), twenty patients from each group of operations (a total of 60 (21 Male)) with symptoms such as maldigestion, steatorrhea, diarrhea, abdominal pain, and low GIQLI scores were randomly selected from the patients completing 1-year follow-up and invited to be included into the study for the evaluation of exocrine pancreatic function. Twenty healthy persons (6 males), whose body mass indexes were similar to the study group and had no previous abdominal surgery and no known EPI or EPI symptoms, were taken as the control group (Fig. 1). Participants received verbal and written information about the study, and informed consent was obtained from all.
Details of the Surgical Procedures
Sleeve gastrectomy was created over a 39F calibration tube using linear stapler starting distally 2 cm from the pylorus towards to the 1 cm lateral from the angle of His (Fig. 2a) as explained by Ozmen and Gagner [17, 18].
During OAGB, a loose gastric pouch, approximately 18–22 cm in length, was created, and gastro-jejunal anastomosis 200 cm distally from the Treitz ligament was performed in ante-gastric fashion (Fig. 2b) with 60-mm linear cutter and was followed by anti-reflux stitches in all patients [19].
In single anastomosis duodenal switch procedure, after performing a loose sleeve (using 50F bougie), the duodenum was transected from the gastroduodenal artery level, and duodenojejunal anastomosis was performed 300 cm distally from the Treitz ligament (Fig. 2c) [20, 21].
FE-1 Measurement
Stool samples were collected from the patients to measure FE-1 levels at the end of the first year. Patients were invited to the clinic where they sampled their stool into a labeled stool tube that was transported to – 20 °C fridge. FE-1 measurements were done using the Pancreatic Elastase ELISA kit from Immundiagnostik (IDK Elastase Kit, Immundiagnostik AG, Bensheim, Germany) according to manufacturer’s instructions (IDK® Pancreatic Elastase ELISA for the in vitro determination of human pancreatic elastase in stool) [22].
The assay is a solid-phase enzyme immunoassay based on double sandwich technique that uses two polyclonal antibodies recognizing different epitopes on human pancreatic elastase sequences. A single spot sample of the stool was used for the test, and the results were given as μg/g stool.
Definition of EPI and PERT
After having measured FE-1 in patients and controls, it was decided for enzyme replacement therapy that PERT would not be given to patients with FE-1 levels higher than 500 μg/g. The logic behind this is the classification of EPI by Borbely at al. [23]. They have classified patients with symptoms as moderate to severe if FE-1 is < 200 μg/g and borderline if FE-1 is 200–500 μg/g [24]. Therefore, none of the patients from the SG group and healthy controls received any replacement treatment (as FE-1 > 500 μg/g).
Ten patients from the OAGB and SADS groups with the lowest value of FE-1 (< 500 μg/g) were given PERT for 3 months using Kreon (Abbott Products GmbH, Hannover, Germany) consisting of 10.000 IU pancreatin (Lipase 10000Ph.Eur.Unit, Amylase 8000Ph.Eur.Unit, Protease 600Ph.Eur.Unit) three times daily.
At the end of these 3 months, FE-1 levels, weight, BMI, EWL, GIQLI scores, and vitamin D levels were measured and noted during this visit. PERT was defined as effective in patients with FE-1 levels higher than 500 μg/g and improvement on EPI symptoms.
Statistical Analysis
The sample size was calculated with a power analysis. A minimum sample size of 15 patients in each group was required for primary outcome measures (FE-1, vitamin D, EWL). The distribution normality of continuous variables was evaluated with the Shapiro-Wilk test, and Mann-Whitney U test was used to evaluate independent groups of non-normal data. The percentage distribution of FE-1 was analyzed using a linear correlation between the groups and EWL using the Pearson correlation test. Analyses were performed with SPSS MAC version 26.0 (SPSS Inc. Chicago, USA), and p < 0.05 was accepted as statistically significant.
Results
When the patients were evaluated according to their demographic characteristics, the groups were similar. In the control group, mean age was 33 (22–56) years, and it was 43 (21–62) years in operated patients. EWL was 58%, 65%, and 70% after SG, OAGB, and SADS, respectively (Table 1).
Vitamin D levels were found to be 21.79 (11–40.3) pg/ml in the control group (severe deficiency < 10 pg/ml, deficiency < 20 pg/ml). Vitamin D levels in the first postoperative year were found to have decreased in almost 60% of the patients. Vitamin D levels were measured as 19.04 (9–46.5) pg/ml after SG, 15.1 (8.4–23.6) pg/ml after OAGB, and 17.8 (5–30) pg/ml after SADS, respectively (p = 0.04). For patients with OAGB, lower levels of vitamin D were found.
Preoperative GIQLI scores of the patients included into the study were 81 (31–125), 82.8 (44–124), and 80.2(40–121) in SG, OAGB, and SADS groups, respectively. Postoperative GIQLI scores in the first year were found to be increased in all patients (SG = 113.9 (82–138), OAGB = 105.9 (58–136), SADS = 101.8 (56–131)) (p = 0.02). After 3 months of PERT therapy, GIQLI scores increased to 118.8 (71–137–720) in the OAGB and 114.1(68–134) in the SADS groups (p = 0.01) (Fig. 3).
FE-1 levels were found as 642.35 (566.3–711.4) μg/g, 378.52 (183.5–561.1) μg/g, and 458.88 (252.5–593.5) μg/g for SG, OAGB, and SADS, respectively, while it was found to be 518.2 (351.6–691) μg/g in the control group (Table 2).
Although levels of FE-1 remained unchanged after SG, a significant decrease was observed following malabsorptive surgeries (p = 0.001).
The correlation between EWL and FE-1 levels was also statistically evaluated. It was found that there was a strong inverse correlation between EWL and FE-1 levels at the end of the first year. (Spearman’s rho = − 0.688, p = 0.003). For the SG group, EWL was lower than the OAGB and SADS groups, but FE-1 levels were higher in the SG group.
After 3 months of PERT therapy in patients with the lowest FE-1 levels, it was increased to 683.39 (615.5–720) μg/g in the OAGB and 691.57 (643.1–720) μg/g in the SADS groups (p = 0.011) (Fig. 4).
Although there was a significant inverse correlation between EWL and FE-1 levels, PERT did not affect weight loss during the 3 months of treatment. In this group of patients after 3 months of PERT therapy, GIQLI scores were also improved in the OAGB and the SADS groups as shown in Fig. 3 (p = 0.01).
Vitamin D levels were also found to have significantly increased after PERT (23.8 (12.2–35) pg/ml in the OAGB and 23.2 (13–30) pg/ml in the SADS groups) (Table 2).
Discussion
Obesity surgery is a successful form of treatment for morbid obesity with innovative methods and increased competence. The main purpose of obesity surgery is weight loss, but these operations have significant limitations that might cause morbidity and mortality. EPI might be one of them as previous studies indicate the increased occurrence of nutritional deficiencies after gastric bypass procedures [25]. However, there is no study evaluating and comparing EPI after three different techniques including restrictive (SG), malabsorptive (OAGB), and combined (SADS) procedures.
In our study, FE-1 levels were inversely proportional to EWL, and in the SG group, EWL was lower than the OAGB and SADS groups, but FE-1 levels were higher in the SG group. The fact that FE-1 levels are inversely proportional to EWL shows that EPI is another factor contributing to weight loss in malabsorptive operations. Additionally, PERT was shown to improve the FE-1 levels of the patients while not having negative effects on weight loss in our study.
It is already known that EPI occurs following upper gastrointestinal surgery for malignancies. After gastric surgery, multiple pathways can affect pancreatic secretions. For exocrine pancreatic functions to be effective, the pH in the intestinal lumen should be at an optimum level. Due to decreased gastric acidity, increased intestinal bacterial overgrowth changes normal pH value, and pancreatic secretions become ineffective [26]. In patients with gastrectomy, decreased CCK secretions result in decreased exocrine pancreatic secretions. After gastric bypass procedures, this pathway is possibly responsible for this [27]. Armbrecht et al. have compared PERT and placebo treatments after surgery in patients operated for gastric cancer and concluded that the stool scores were significantly better in the PERT group, and stool fat excretions were significantly reduced [28]. In another study published by Brägelmann et al., it was observed that the patients using PERT showed a significant improvement in abdominal findings compared with the group using placebo [29]. Similarly, in our study, we found that there was a significant improvement in FE-1 levels and GIQLI scores of the patients in parallel with PERT treatment given in gastric bypass or duodenal switch groups, which are supported by previous studies.
In SG, as the anatomy of the antrum and pyloric parts of the stomach are partially preserved, stomach acidity and intestinal pH might remain in optimum levels. The preserved FE-1 levels in SG patients might partly be explained by this, and due to normal CCK stimulation after SG, the pancreas may effectively continue its digestive function [30].
On the other hand, preservation of the pylorus and the duodenum is vital for the secretion of CCK and normal pancreatic functions which results in normal FE-1 levels. In OAGB and SADS, as the foods do not interact with gastric and pancreatic secretions, exocrine pancreatic secretions do not occur with intestinal stimulation. EPI correlates with decreased pancreatic secretions.
EPI is common in both type 1 and type 2 diabetes [31]. The relationship between obesity syndrome and diabetes mellitus is well defined. The risk of diabetes is increased for overweight or obese people without metabolic syndrome [32]. Hahn et al. have demonstrated an increased risk of EPI as BMI increases in patients with diabetes mellitus [33]. However, excess weight does not seem to affect the function of the exocrine pancreas unless it is related with diabetes mellitus. In BS today, we have various well-defined surgical techniques such as Roux-n Y gastric bypass (RYGB), OAGB, adjustable gastric banding, biliopancreatic diversion (BPD), and SADS. After SADS and OAGB, type 2 diabetes mellitus and insulin resistance are significantly decreased [25]. However, the benefits of bariatric surgery procedures on diabetes recovery are not accepted to be sufficient alone in the efforts to correct EPI.
One of the well-known complications of BS is decreased vitamin and nutrient absorption and related deficiencies. Malabsorptive surgeries are known to cause vitamin B12, iron, and folate deficiencies, and most surgeons recommend daily multivitamin supplements for these patients [34]. Procedures that induce weight loss by fat malabsorption can also affect the absorption of fat-soluble nutrients such as vitamins A, D, E, and K, zinc, and essential fatty acids. Similarly, Slater et al. [35] have put forward that low vitamin D levels after BS may continue for a long time after surgery, and that vitamin supplements should continue. Although we used multivitamin supplements in all BS patients, we observed a statistically significant impairment in vitamin D levels if EPI also developed in patients after malabsorptive surgeries in which fat absorption was impaired. Arias et al. have also shown that the absorption of vitamin D is affected after gastric bypass [36]. We observed significant improvements in these impaired values after PERT. These findings show that besides absorption-dependent vitamin D deficiency, fat malabsorption also contributes to the deepening of fat-soluble vitamin deficiencies like vitamin D.
FE-1 is a basic and non-invasive technique to diagnose EPI [37]. Many studies in the literature have used FE-1 for the evaluation of EPI. Despite its worldwide usage, its accuracy rate is low, especially in mild EPI patients. Recent studies have shown that FE-1 and 13C-mixed breath tests have similar diagnostic power for the diagnosis of EPI in patients with chronic pancreatitis [38]. Depending on these recommendations and information, we can easily say that FE-1 is a reliable test for the diagnosis of EPI.
Our study is the first prospective case-control study evaluating the effectiveness of PERT in EPI and exocrine pancreatic function after different bariatric procedures (SG, OAGB, SADS) by using FE-1 assay. Miroslav et al. have also reported severe EPI at a rate of 9.1% in their pilot study on gastric bypass patients (RYGB and OAGB), and the use of FE-1 in diagnosis alone may not be sufficient due to the low sensitivity of FE-1. They have remarked that the use of secretin magnetic retrograde cholangiopancreatography may be useful in revealing the diagnosis of EPI in this group of patients. Despite the low GIQLI scores of the patients included in our study, we found that FE-1 levels did not correlate with these scores at an expected level. We are also of the opinion that magnetic resonance images with FE-1 measurements may increase sensitivity in diagnosis [39].
EPI treatment was focused on dietary advice and PERT in our study. Inhibition of gastric acid secretion is often required to increase the effectiveness of PERT. We can conclude that PERT should be started in all patients with EPI with the presence of symptoms and/or nutritional deficiencies, which may occur in patients who have undergone a malabsorptive type of surgery. The main goal of the treatment should be relieving EPI symptoms and correcting nutritional deficiencies. Therefore, enzyme replacement therapy is performed after both the patient’s diet and deficiencies are corrected.
We showed early findings after SG, OAGB, and SADS; however, we still do not know the long-term impact on exocrine pancreatic functions. We found a significant improvement in FE-1 levels after 3 months of PERT treatment in the OAGB and SADS groups.
Conclusion
After BS, patients may suffer from different levels of impaired bowel habits and vitamin deficiencies depending on the type of procedure performed, and many of these findings might be related with EPI. FE-1 measurements showed that almost every patient suffers from malabsorption after OAGB or SADS, whereas functions remain normal after SG. PERT corrects pancreatic functions without affecting weight loss and also contributes to the normal serum level of vitamin D. Therefore, we conclude that PERT should be a part of the treatment algorithm, especially after malabsorptive procedures.
References
Mezza T, Cinti F, Giaccari A. Diabetes secondary to pancreatic diseases. In: Diabetes Complications, Comorbidities and Related Disorders; 2020. p. 523–39.
Wang D, Wang J, Bai L, et al. Long-term expansion of pancreatic islet organoids from resident Procr+ progenitors. Cell. 2020;180(6):1198–211.
Vélez CD, Kuo B. Gastroduodenal anatomy and physiology. In: Clinical and Basic Neurogastroenterology and Motility. Cambridge, MA: Academic Press; 2020. p. 89–100.
Rehfeld JF. Measurement of cholecystokinin in plasma with reference to nutrition related obesity studies. Nutr Res. 2020;76:1–8.
Lahsen R, Berry M. Surgical interventions to correct metabolic disorders. Br J Diabetes Vasc Dis. 2010;10(3):143–7.
Ghodeif AO, Azer SA. Pancreatic Insufficiency. In StatPearls [Internet]. StatPearls Publishing. 2020.
Lankisch PG, Schmidt I, Konig H, et al. Faecal elastase 1: not helpful in diagnosing chronic pancreatitis associated with mild to moderate exocrine pancreatic insufficiency. Gut. 1998;42:551–4.
Pezzilli R, Caccialanza R, Capurso G, et al. Pancreatic enzyme replacement therapy in pancreatic cancer. Cancers. 2020;12(2):275.
Imrie CW, Connett G, Hall RI, et al. Enzyme supplementation in cystic fibrosis, chronic pancreatitis, pancreatic and periampullary cancer. Aliment Pharmacol Ther. 2010;32:1–25.
Dominguez Munoz JE. Diagnosis of chronic pancreatitis: functional testing. Best Pract Res Clin Gastroenterol. 2010;24:233–41.
Domínguez-Munoz JE, Hieronymus C, Sauerbruch T, et al. Fecal elastase test: evaluation of a new noninvasive pancreatic function test. Am J Gastroenterol. 1995;90:1834–7.
Behhary S, Ellis L, Corey M, et al. How useful is fecal pancreatic elastase 1 as a marker of exocrine pancreatic disease? J Pediatr. 2002;141:84–90.
Vujasinovic M, Valente R, Thorell A, et al. Pancreatic exocrine insufficiency after bariatric surgery. Nutrients. 2017;9(11):1241.
Sabater L, Ausania F, Bakker OJ, et al. Evidence-based guidelines for the management of exocrine pancreatic insufficiency after pancreatic surgery. Ann Surg. 2016;264:949–58.
Dominguez-Muñoz JE. Diagnosis and treatment of pancreatic exocrine insufficiency. Curr Opin Gastroenterol. 2018;34(5):349–54.
Ledoux S, Flamant M, Calabrese D, et al. What are the micronutrient deficiencies responsible for the most common nutritional symptoms after bariatric surgery? Obes Surg. 2020; 30(5):1891–1897. https://doi.org/10.1007/s11695-020-04412-8.
Ozmen MM, Gagner M. Laparoscopic sleeve gastrectomy: pitfalls and techniques to prevent complications. Eur J Endosc Laparosc Surg. 2014;1:55–8.
Guldogan CE, Ozozan OV, Ozmen MM. Sleeve gastrectomy and its modifications. Ann Laparosc Endosc Surg. 2020; https://doi.org/10.21037/ales-20-30.
Ozmen MM, Sahin TT, Güldogan CE. Single anastomosis gastric bypass: a novel bariatric procedure. Eur J Endos Laparosc Surg. 2014;1:187–95.
OZMEN MM, Guldogan CE, Gundogdu E. Changes in HOMA-IR Index levels after bariatric surgery: comparison of single anastomosis duodenal switch-proximal approach (SADS-p) and one anastomosis gastric bypass-mini gastric bypass (OAGB-MGB). Int J Surg. 2020; online first; https://doi.org/10.1016/j.ijsu.2020.04.008.
Ozmen MM. Single anastomosis duodenal switch: a novel procedure for obesity and metabolic surgery. Ann Laparosc Endosc Surg. 2020; online first; https://doi.org/10.21037/ales-2019-bms-07.
IDK PMN-Elastase ELISA. For the in vitro determination of PMN elastase in stool. (27/03/2019) Available at http://www.immundiagnostik.com/fileadmin/pdf/PMN-Elastase_1P_K6830.pdf
Borbély Y, Plebani A, Kröll D, et al. Exocrine pancreatic insufficiency after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2016;12(4):790–4.
Sollier C, Barsamian C, Bretault M, et al. Diagnostic and therapeutic management of post-gastric bypass chronic diarrhea: a systematic review. Obes Surg. 2020:1–10.
Domínguez-Muñoz JE. Pancreatic enzyme replacement therapy: exocrine pancreatic insufficiency after gastrointestinal surgery. HPB. 2009;11:3–6.
Chaudhary A, Domínguez-Muñoz JE, Layer P, et al. Pancreatic exocrine insufficiency as a complication of gastrointestinal surgery and the impact of pancreatic enzyme replacement therapy. Dig Dis. 2020;38(1):53–68.
Svane MS, Bojsen-Møller KN, Martinussen C, et al. Postprandial nutrient handling and gastrointestinal hormone secretion after Roux-en-Y gastric bypass vs sleeve gastrectomy. Gastroenterology. 2019;156(6):1627–41.
Armbrecht U, Lundell L, Stockbrügger RW. The benefit of pancre- atic enzyme substitution after total gastrectomy. Aliment Pharmacol Ther. 1988;2:493–500.
Brägelmann R, Armbrecht U, Rosemeyer D, et al. The effect of pancreatic enzyme supplementation in patients with steatorrhoea after total gastrectomy. Eur J Gastroenterol Hepatol. 1999;11:231–7.
Lüth S, Teyssen S, Forssmann K, et al. Fecal elastase-1 determination: gold standard of indirect pancreatic function tests. Scand J Gastroenterol. 2001;36(10):1092–9.
Hardt PD, Krauss A, Bretzetal L. Pancreatic exocrine function in patients with type 1 and type 2 diabetes mellitus. Acta Diabetol. 2000;37(3):105–10.
Arnlov J, Sundstrom J, Ingelsson E, et al. The impact of body mass index and the metabolic syndrome on the risk of diabetes in middle-aged men. Diabetes Care. 2011;34(1):61–5.
Hahn JU, Kerner W, Maisonneuve P, et al. Low fecal elastase 1 levels do not indicate exo- crine pancreatic insufficiency in type-1 diabetes mellitus. Pancreas. 2008;36(3):274–8.
Bal BS, Finelli FC, Shope TR, et al. Nutritional deficiencies after bariatric surgery. Nat Rev Endocrinol. 2012;8(9):544–56.
Slater GH, Ren CJ, Siegel N, et al. Serum fat-soluble vitamin deficiency and abnormal calcium metabolism after malabsorptive bariatric surgery. J Gastrointest Surg. 2004;8(1):48–55.
Arias PM, Domeniconi EA, García M, et al. Micronutrient deficiencies after Roux-en-Y gastric bypass: long-term results. Obes Surg. 2020;30(1):169–73.
Chowdhury RS, Forsmark CE. Pancreatic function testing. Aliment Pharmacol Ther. 2003;17(6):733–50. https://doi.org/10.1046/j.1365-2036.2003.01495.x.
Bernhard R, Gabriele R, Kaser S. Exocrine Pancreatic Insufficiency in Type 1 and Type 2 Diabetes. Currt Diabet Rep. 2020;20(6):18. https://doi.org/10.1007/s11892-020-01304-0.
Miroslav V, Gregor K, Brane B, et al. Is pancreatic exocrine insufficiency a cause of Malabsorption in patients after bariatric surgery? J Pancreas (Online). 2016;17(4):402–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
The authors state that this study has been approved by the appropriate institutional and research ethics committee and has been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed Consent Statement
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ozmen, M.M., Gundogdu, E., Guldogan, C.E. et al. The Effect of Bariatric Surgery on Exocrine Pancreatic Function. OBES SURG 31, 580–587 (2021). https://doi.org/10.1007/s11695-020-04950-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04950-1