Abstract
Purpose
Biliopancreatic diversion with duodenal switch (BPD-DS) is an effective weight loss surgical procedure. Yet, BPD-DS is technically difficult to perform and carries a higher risk of nutrient deficiencies as compared with other surgical interventions. Single-anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S) is a modified BPD-DS procedure conceived with the aim of decreasing the technical complexity, while retaining the weight loss efficiency. Whether the two surgical procedures diverge in nutrient absorption rates and malnutrition risk is still matter of debate. Our aim was to determine if postprandial nutrient absorption rates are different in patients subjected to BPD-DS or SADI-S for weight loss.
Materials and Methods
Plasma amino acid metabolomic profiling during mixed-meal tolerance test (MMTT) was performed in subjects (N = 18) submitted to BPD-DS (n = 9) or SADI-S (n = 9) 1.6 ± 0.1 years earlier.
Results
Patients submitted to SADI-S or BPD-DS presented distinct postprandial metabolomic profiles. Postprandial excursions of total and essential amino acids—leucine, isoleucine, and valine—were higher after SADI-S as compared with BPD-DS.
Conclusion
Our study demonstrates that a simplified malabsorptive bariatric surgery procedure SADI-S results in greater essential branched-chain amino acid absorption when compared with the classical BPD-DS intervention. These findings suggest that SADI-S can potentially lower lifetime risk of postoperative protein malnutrition, as well as have a positive impact on systemic metabolism and glucose homeostasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity prevalence increased exponentially over the last decades being currently a major public health concern [1]. Moreover, morbid obesity rates that carry a high risk of comorbid conditions and decrease life expectancy also reached unprecedented levels [2]. Severe obesity is recognized for being refractory to lifestyle and pharmacological interventions, while bariatric surgery is the only treatment with proven efficacy to achieve significant and sustained weight loss [3, 4]. Biliopancreatic diversion with duodenal switch (BPD-DS) is one of the most effective bariatric surgery interventions for the treatment of obesity and obesity-related comorbidities. [5,6,7]. Yet, BPD-DS is usually reserved for subjects with BMI greater than 50 kg/m2 or greater than 40 kg/m2 in the presence of one or more obesity-related conditions. It represents a minor percentage of bariatric surgery interventions performed worldwide, attributed to greater technical difficulty and associated risk of postoperative complications and malnutrition as compared with other bariatric procedures [6, 8]. Single-anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S) is a bariatric surgery procedure introduced in 2007 by Sánchez-Pernaute et al. with the primary purpose of reducing the risk of surgical complications associated with BPD-DS, while maintaining the weight loss efficacy [9]. Briefly, SADI-S consists in a modified BPD-DS with “one-anastomosis” only by eliminating the distal ileo-ileal anastomosis, thus reducing the technical complexity and operative time of the procedure, as well as the risk of surgical complications due to leaks, fistulae, and internal hernias through the mesenteric defect.
Patients submitted to BPD-DS and SADI-S achieve similar high rates of over 80% short and mid-term excess weight loss, and obesity comorbidity resolution, with the advantage of SADI-S requiring a shorter operative time [10,11,12,13]. Nevertheless, despite achieving similar short-term clinical outcomes, the endocrine mechanisms underlying the weight loss and metabolic effects of the two surgical procedures are potentially different, since postprandial GLP-1, glucagon, and insulin levels were demonstrated to be higher in patients previously submitted to SADI-S when compared with BPD-DS patients [14].
Malabsorptive surgeries, such as BPD-DS and SADI-S, rely on nutrient malabsorption as an important contributing mechanism to weight loss, which explains that malnutrition and protein deficiencies are reported as potential risks and therapeutic side effects of these interventions [15]. Protein malnutrition usually presents with fatigue, hair loss, and alopecia, as well as peripheral edemas, along with low serum albumin and protein levels [16]. Because SADI-S is characterized by a longer common limb compared with BPD-DS, it has been suggested that the longer absorptive area could potentially reduce the risk of nutrient malnutrition [8, 17], although this has not yet been demonstrated.
Therefore, the aim of this study was to compare the protein status, as well as the postabsorptive amino acid profile of subjects submitted to BPD-DS or SADI-S.
Methods
Participants
Subjects from a larger cohort of patients submitted to bariatric surgery for the primary treatment of obesity and obesity related comorbidities at a single institution, who met the enrolment criteria, were consecutively invited to participate in the study. Inclusion criteria were previous BPD-DS or SADI-S bariatric procedures and being weight stable for at least 6 months prior to study enrolment. Exclusion criteria were ongoing pregnancy and medical history of type 2 diabetes prior to or after surgery, according to the following criteria: Hb1Ac > 6.5%, fasting plasma glucose > 7.0 mmol/L, or being under glucose-lowering drugs. Subjects that met all eligibility criteria and accepted to participate were included in the study after informed consent.
Study subjects were allocated into 2 groups (n = 9/group) according to the type of bariatric surgery performed BPD-DS or SADI-S, as well as paired according to age at time of surgery, preoperative body mass index (BMI), and follow-up time after surgery.
Peripheral edema, fatigue, and low serum albumin (< 3.5 g/dL) or total protein levels (< 7 g/dL) were considered signs of protein malabsorption.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Surgical Procedures
All surgeries were performed laparoscopically by the same surgical team with similar experience in performing both surgical procedures at a single public bariatric center. The criteria for choosing between performing a SADI-S or BPD-DS procedure in a patient with a BMI greater than 50 kg/m2 was based on the patient preference, surgeon technical aptitudes, and surgical feasibility.
The BPD-DS was performed with a common limb of 100 cm and an alimentary limb of 200 cm, while the SADI-S was performed with a 300-cm common channel (Fig. 1), as previously described [14].
Study Design
After an overnight fast, subjects underwent a mixed-meal tolerance test (MMTT), in which a standardized commercially available liquid meal [Fresubin energy drink, 200 mL, 300 kcal (50E% carbohydrate, 15E% protein, and 35E% fat); Fresenius Kabi Deutschland, Bad Homburg, Germany] was ingested over a maximum period of 15 min. Peripheral venous blood samples were collected, from a catheter placed in an antebrachial vein, into ethylenediaminetetraacetic acid (EDTA) tubes (S-Monovette® 7.5 ml, K2 EDTA Gel, 1.6 mg/mL, Sarstedt), before the meal and at 15, 30, 45, and 120 min after the start of meal intake. The plasma was then separated and stored at − 20 °C until assayed.
Total Proteins, Albumin, Urea, and Plasma Amino Acid Measurement
Total proteins, albumin, and urea levels were quantified by spectrophotometry, using a hospital routine chemistry analyzer (Cobas 8000, Roche, USA). Total amino acid levels were quantified using a validated enzyme-linked immunosorbent assay (ELISA) (catalog no. ab65347; Abcam, Cambridge, UK), as previously described [18].
NMR Spectroscopy
Individual amino acid profiles were evaluated by nuclear magnetic resonance (NMR) spectrometry. This technique relies on the fact that molecules have variable chemical structures and hydrogen contents that result in different resonance frequencies and produces characteristic NMR signals, which allows to identify single metabolites present in cells or biologic fluids across a spectrum [19].
NMR metabolomics were used to quantify the plasma total metabolite content and to identify the metabolic signature of patients previously submitted to bariatric surgeries at a given time point during a mixed meal tolerance test.
Briefly, plasma samples (0, 15, 30, 45, and 120 min after the mixed meal ingestion) were homogenized and centrifuged at 9200 rpm for 5 min. Then, 45 μL of fumarate solution in D20 (2 mM, pH 7) was added to 180 μL of the plasma samples, and the mixture was homogenized and centrifugated (9200 rpm, 5 min). Each sample was transferred to an NMR tube and analyzed, as previously described [20].
Plasma metabolite 1H NMR presat spectra (Fig. 2a) are dominated by broad and high signals derived from lipoproteins that tend to overlap smaller metabolite signals. Therefore, 1H NMR cpmg spectra (Carr-Purcell-Meiboom-Gill spin-echo pulse sequence) were used to analyze amino acid after lipoprotein signal suppression (Fig. 2b).
Typical 1H NMR (presat) spectrum of plasma metabolites of a patient submitted to SADI-S at t = 0 (a). Spectrum used for amino acid analysis after lipoprotein signal suppression that enabled to visualize small metabolite signals (cpmg spectrum, b) indicated across the line: Ala alanine, BBCA branched chain amino acids (Val, Leu, Ile), EDTA ethylenediaminetetraacetic acid, Glc glucose, Gln glutamine, Lac lactate
Statistical Analysis
NMR data (17,504 points × 88 samples) was analyzed by multivariate analysis, as previously described [20]. Principal component analysis (PCA) was used to reduce the data information into two dimensions that allowed to identify the differences between surgical groups. Cluster formation and separation in (PC1, PC2) plots indicate differences in the surgical group metabolome. Pairwise partial least square discriminant analysis (PLS-DA) was used to identify metabolites that are differentially expressed in SADI-S or BPD-DS groups and that were responsible for group separations.
Amino acid areas were integrated in cpmg spectra and were analyzed by repeated measures two-way ANOVA (with Geisser-Greenhouse correction for the assumption of sphericity) followed by Sidak’s post hoc tests to compare amino acid levels at different time points.
Continuous variables are expressed as mean ± standard SD unless stated otherwise. Normality of continuous variables was evaluated using the D’Agostinho and Pearson test. For continuous variables, an unpaired two-tailed t test was used to compare the means of the two groups. For variables that did not pass the normality test, a Mann-Whitney test was used.
Total area under the curve (tAUC) was calculated for the total amino acids and for each individual amino acid analyzed using the trapezoidal rule. Incremental area under the curve (iAUC) was calculated subtracting the basal values to the tAUC.
Statistical analysis was performed using the GraphPad Prism version 6.01 for Windows (GraphPad Software, La Jolla, CA, USA). A p < 0.05 was considered statistically significant.
Results
Demographic and Clinical Data
There were no significant differences in the anthropometric features between the BPD-DS and SADI-S patient groups whether preoperatively and at the time of the MMTT (postoperatively) (Table 1). None of the study subjects presented symptoms nor signs of protein or lipid malabsorption, namely fatigue, peripheral edema, or steatorrhea.
There were also no significant differences between the two study groups with respect to total proteins (BPD-DS 6.7 ± 0.2 g/dL vs SADI-S 6.9 ± 0.3 g/dL, p = 0.22), albumin (BPD-DS 4.3 ± 0.1 g/dL vs SADI-S 4.2 ± 0.4 g/dL, p = 0.99), or urea (BPD-DS 25.6 ± 6.5 g/dL vs SADI-S 25.0 ± 5.7 g/dL, p = 0.65) levels, which were found to be within the normal limits in every study participant at 24 months after bariatric interventions.
Amino Acid Levels at Fasting State Are Similar in Both Surgical Groups
Fasting levels of total and individual amino acids were not significantly different between the study groups (p > 0.05, Table 2).
Postprandial Levels of Total and Branched Chain Amino Acids Are Higher in SADI-S Group
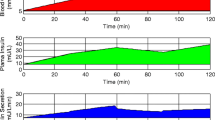
Thirty and forty-five minutes after the mixed meal intake, significantly higher levels of total amino acids were observed in the SADI-S group (Table 2; Fig. 3, 30 min, p < 0.01 and 45 min, p < 0.001).
PCA was used to identify clusters of individuals subjected to SADI-S and BPD-DS at individual time points (Fig. 4 left). The separation of postprandial plasma metabolic profiles between SADI-S and BPD-DS was predominantly observed at 30 and 45 min after the meal (Fig. 4a, b). This difference between the two surgical procedures was mostly attributed to branched-chain amino acids (BCAAs) that were higher in SADI-S group. At 120 min after meal, there was an overlap of metabolite species and concentrations in the two groups (Fig. 4c). After that, PLS-DA was applied to identify which metabolites were responsible for the separation between SADI-S and BPD-DS metabolome profiles (Fig. 4 right).
Principal component analysis (PCA) plots (left) and loading plots of the partial least square discriminant analysis (PLS-DA) models (right) of 1H NMR spectra, at different time points after meal: a 30 min, b 45 min, and c 120 min. PCA was used to observe possible clustering of individuals subjected to SADI-S and BPD-DS at individual time points. Separation of postprandial plasma metabolic profiles between SADI-S and BPD-DS was observed predominantly at 30 and 45 min after the meal. PLS-DA was applied to identify differentially expressed metabolites responsible for the separation of SADI-S and BPD-DS. The main difference observed between the two surgical methods, at 30 and 45 min after the meal, is in the BCAA levels being higher in the SADI-S group. Loadings are colored according to the variable importance in projection (VIP), and some assignments are indicated: branched chain amino acids (BCAAs), alanine (Ala), glutamine (Gln), threonine (Thr), and valine (Val). VIP > 1 indicate differentially expressed metabolites in respective groups
Postmeal levels of individual amino acid differed significantly between groups of subjects that underwent BPD-DS and SADI-S (Fig. 4 and Table 2). In particular, the iAUC of valine, leucine, and isoleucine were significantly higher in the SADI-S group as compared with the BPD-DS (p < 0.05, Table 2).
Thirty minutes after meal intake, significantly higher leucine levels were observed in the SADI-S group (p < 0.05, Fig. 5b). Similarly, at 45 min of MMTT, the valine, leucine, and isoleucine levels were significantly higher in the SADI-S group as compared with the BPD-DS group (p < 0.05, Fig. 5a–c). At 120 min, all the analyzed amino acid levels were similar between the two groups (p > 0.05).
Peripheral plasma levels of valine (a), leucine (b), isoleucine (c), glycine (d), alanine (e), glutamine (f), proline (g), and threonine (h) in subjects previously submitted to BPD-DS (n = 9) or SADI-S (n = 9) after ingestion of a standard mixed-meal served at t = 0 min. Data are presented as mean ± standard error of the mean. Two-way ANOVA: *p < 0.05 and **p < 0.01
No significant differences in other amino acids observed in 1H cpmg spectra, namely glycine, alanine, glutamine, proline, and threonine postprandial plasma levels, were observed between SADI-S and BPD-DS (p > 0.05, Fig. 5d–h).
Discussion
Malabsorptive bariatric surgeries, including BPD-DS and SADI-S, share as common anatomical feature exclusion of the proximal small gut from the intestinal transit and delaying the mixture of pancreatic enzymes with the nutrients, which consequently results in reduced and/or delayed protein digestion and absorption [21]. In normal physiological conditions, protein digestion is initiated within the stomach by the action of pepsin. The intermediate protein hydrolysis mixture comprising oligopeptides and free amino acids formed in the stomach are then delivered to the duodenum, where by the action of pancreatic enzymes, protein digestion is completed having as end result the release of free amino acids and dipeptides and tripeptides amenable for absorption by the enterocytes [22]. BPD-DS and SADI-S share the anatomic features that characterize malabsorptive bariatric surgeries, including a reduced stomach volume due to a vertical gastrectomy in addition to a shortened common intestinal limb, where the majority of the nutrients is absorbed. Yet, the small intestinal region where the first contact of nutrients with pancreatic juices occurs is considerably different in the two bariatric procedures, being located 100 cm from the ileum-cecum valve for BPD-DS and 300 cm from the vale for SADI-S. Consequently, SADI-S has a much longer common intestinal limb when compared with BPS-DS. Thus, it is conceivable that the different anatomical rearrangement of the gastro-intestinal tract produced by the two surgical procedures, can result in distinct protein digestion efficiencies and amino acid absorption, with a potential advantage for SADI-S when compared with BPD-DS. However, there are no clinical data available in support of SADI-S advantage over BPD-DS in what concern protein absorption [10, 11]. Therefore, we decided to investigate the impact of BPD-DS and SADI-S on amino acid excursions in the systemic circulation after a meal challenge.
The postprandial valine, leucine, and isoleucine levels of subjects submitted to SADI-S were higher when compared with those of patients submitted to BPD-DS. Valine, leucine, and isoleucine, which belong to the BCAA family, are considered essential amino acids since being indispensable substrates for human systemic metabolism, they cannot be synthesized de novo in the organism [23, 24]. Free essential amino acids are reported to be absorbed mainly in the proximal small intestine [25]. Since the intestinal rearrangement of BPD-DS as compared with SADI-S results in a shorter distal common intestinal limb available for proteins digestion and amino acids absorption (100 cm vs 300 cm), the decreased absorption of essential amino acid and the lower postprandial excursion in circulating plasma levels observed a predicted finding for a malabsorptive surgical procedure.
BCAAs comprise 15% up to 20% of protein intake and are important substrates for protein and glucose metabolism and participate in several physiological functions including glucose homeostasis by inducing insulin release by pancreatic β cells [26,27,28]. In a previous study, our group reported that on top of the anatomical differences, BPD-DS and SADI-S also elicit different postprandial hormone responses. In particular, patients submitted to SADI-S present higher postprandial insulin and glucagon levels, when compared with BPD-DS patients [14]. Our current study results further suggest that the higher postprandial BCAA levels observed in subjects previously submitted to SADI-S may contribute to the enhanced postprandial insulin levels observed in those patients. Besides that, other amino acids such as glycine, proline, alanine, and glutamine, are able to stimulate glucagon secretion and therefore known as glucagonotropic [18, 29]. However, since the glucagonotropic amino acid levels were similar in both study groups, our data do not support that amino acids would be responsible for higher postprandial glucagon levels found in patients submitted to SADI-S [14], which should be related to other still unidentified mechanisms.
Despite postprandial essential BCAA profile being significantly different in subjects submitted to SADI-S or BPD-DS, no other clinical or biochemical signs of protein malabsorption and consequent protein deficiency were observed in any of the study subjects up to 2 years after surgery. In pprevious cohort studies conducted in patients submitted to SADI-S with follow-up times ranging between 1 and 4 years, albumin and total protein deficiencies are reported to occur in 3 to 14% and 8 to 34% of the patients, respectively [10, 30,31,32,33,34,35,36]. Additionally, Zaveri et al found that the risk of albumin or total protein deficiencies increases significantly over the years as compared with the preoperative time [30]. Notwithstanding, no significant differences in protein and albumin deficiency rates were so far reported in studies comparing patients submitted to SADI-S and BPD-DS [10, 11].
Urea is a product of amino acid metabolism produced in the liver [37]. Since postsurgical levels of urea were within the normal reference range and similar in both study groups, the rate of amino acid turnover was most likely similar and uncompromised in these subjects.
Our study has generated novel and clinically relevant data on the amino acid absorption profiles after two different malabsorptive obesity surgeries, but there are some limitations that need to be acknowledged. Thus, identification and measurement of every single circulating amino acid were not performed due to the limitations of the NMR technique, such as low resolution and sensitivity. Besides that, since SADI-S is a bariatric surgery procedure relatively recently described as compared with other interventions, no long-term data on the rate of protein deficiencies are available to extend our study results. Moreover, the small number of subjects participating in the study is also a limitation, although mitigated by the low variability of results observed within each group.
Conclusion
In conclusion, our study demonstrates that the postprandial amino acid metabolic signature after two different malabsorptive obesity surgery procedures differs. SADI-S, a simplified version of the BPD-DS procedure, results in higher postprandial levels of essential branched-chain amino acids likely attributed to enhanced absorption suggesting that SADI-S could result in a lower lifetime risk of protein malnutrition.
However, these findings need further validation in a larger cohort of patients submitted to BPD-DS and SADI-S with longer postoperative follow-up times.
References
Collaborators GBDO, Afshin A, Forouzanfar MH, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377(1):13–27.
Apovian CM. Obesity: definition, comorbidities, causes, and burden. Am J Manag Care. 2016;22(7 Suppl):s176–85.
Glandt M, Raz I. Present and future: pharmacologic treatment of obesity. J Obes. 2011;2011:636181.
Adams TD, Davidson LE, Litwin SE, et al. Weight and metabolic outcomes 12 years after gastric bypass. N Engl J Med. 2017;377(12):1143–55.
Skogar ML, Sundbom M. Duodenal switch is superior to gastric bypass in patients with super obesity when evaluated with the bariatric analysis and reporting outcome system (BAROS). Obes Surg. 2017;27(9):2308–16.
Strain GW, Torghabeh MH, Gagner M, et al. The impact of biliopancreatic diversion with duodenal switch (BPD/DS) over 9 years. Obes Surg. 2017;27(3):787–94.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–37.
Sethi M, Chau E, Youn A, et al. Long-term outcomes after biliopancreatic diversion with and without duodenal switch: 2-, 5-, and 10-year data. Surg Obes Relat Dis. 2016 Nov;12(9):1697–705.
Sanchez-Pernaute A, Rubio Herrera MA, Perez-Aguirre E, et al. Proximal duodenal-ileal end-to-side bypass with sleeve gastrectomy: proposed technique. Obes Surg. 2007;17(12):1614–8.
Surve A, Zaveri H, Cottam D, et al. A retrospective comparison of biliopancreatic diversion with duodenal switch with single anastomosis duodenal switch (SIPS-stomach intestinal pylorus sparing surgery) at a single institution with two year follow-up. Surg Obes Relat Dis. 2017;13(3):415–22.
Cottam A, Cottam D, Portenier D, et al. A matched cohort analysis of stomach intestinal pylorus saving (SIPS) surgery versus biliopancreatic diversion with duodenal switch with two-year follow-up. Obes Surg. 2017;27(2):454–61.
Surve A, Cottam D, Sanchez-Pernaute A, et al. The incidence of complications associated with loop duodeno-ileostomy after single-anastomosis duodenal switch procedures among 1328 patients: a multicenter experience. Surg Obes Relat Dis. 2018;14(5):594–601.
Torres A, Rubio MA, Ramos-Levi AM, et al. Cardiovascular risk factors after single anastomosis duodeno-Ileal bypass with sleeve gastrectomy (SADI-S): a new effective therapeutic approach? Curr Atheroscler Rep. 2017;19(12):58.
Pereira SS, Guimaraes M, Almeida R, et al. Biliopancreatic diversion with duodenal switch (BPD-DS) and single-anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S) result in distinct post-prandial hormone profiles. Int J Obes (Lond). 2019;43(12):2518–2527.
Billeter AT, Fischer L, Wekerle A-L, et al. Malabsorption as a therapeutic approach in bariatric surgery. Viszeralmedizin. 2014;30(3):198–204.
Atiyeh B Body contouring following bariatric surgery and massive weight loss: post-bariatric body contouring: Bentham science publishers; 2012.
Moon RC, Kirkpatrick V, Gaskins L, et al. Safety and effectiveness of single- versus double-anastomosis duodenal switch at a single institution. Surg Obes Relat Dis. 2019;15(2):245–52.
Wewer Albrechtsen NJ, Junker AE, Christensen M, et al. Hyperglucagonemia correlates with plasma levels of non-branched-chain amino acids in patients with liver disease independent of type 2 diabetes. Am J Physiol Gastrointest Liver Physiol. 2018;314(1):G91–g6.
Emwas A-H, Roy R, McKay RT, et al. NMR spectroscopy for metabolomics research. Metabolites. 2019;9(7):123.
Jarak I, Pereira SS, Carvalho RA, et al. Gastric Bypass with different biliopancreatic limb lengths results in similar post-absorptive metabolomics profiles. Obes Surg. 2020;30(3):1068–1078.
Handzlik-Orlik G, Holecki M, Orlik B, et al. Nutrition management of the post-bariatric surgery patient. Nutr Clin Pract. 2015;30(3):383–92.
Kiela PR, Ghishan FK. Physiology of intestinal absorption and secretion. Best Pract Res Clin Gastroenterol. 2016;30(2):145–59.
Brosnan JT, Brosnan ME. Branched-chain amino acids: enzyme and substrate regulation. J Nutr. 2006;136(1):207S–11S.
Wu G. Amino acids: metabolism, functions, and nutrition. Amino Acids. 2009;37(1):1–17.
Adibi SA, Gray SJ. Intestinal absorption of essential amino acids in man. Gastroenterology. 1967;52(5):837–45.
Sener A, Malaisse WJ. The stimulus-secretion coupling of amino acid-induced insulin release: insulinotropic action of branched-chain amino acids at physiological concentrations of glucose and glutamine. Eur J Clin Investig. 1981;11(6):455–60.
Yoon M-S. The emerging role of branched-chain amino acids in insulin resistance and metabolism. Nutrients. 2016;8(7):405.
Yang J, Chi Y, Burkhardt BR, et al. Leucine metabolism in regulation of insulin secretion from pancreatic beta cells. Nutr Rev. 2010;68(5):270–9.
Müller WA, Faloona GR, Unger RH. The effect of alanine on glucagon secretion. J Clin Invest. 1971;50(10):2215–8.
Zaveri H, Surve A, Cottam D, et al. Mid-term 4-year outcomes with single anastomosis duodenal-Ileal bypass with sleeve gastrectomy surgery at a single US Center. Obes Surg. 2018;28(10):3062–72.
Cottam A, Cottam D, Zaveri H, et al. An analysis of mid-term complications, weight loss, and type 2 diabetes resolution of stomach intestinal pylorus-sparing surgery (SIPS) versus roux-en-Y gastric bypass (RYGB) with three-year follow-up. Obes Surg. 2018;28(9):2894–2902.
Cottam A, Cottam D, Roslin M, et al. A matched cohort analysis of sleeve Gastrectomy with and without 300 cm loop duodenal switch with 18-month follow-up. Obes Surg. 2016;26(10):2363–9.
Topart P, Becouarn G. The single anastomosis duodenal switch modifications: a review of the current literature on outcomes. Surg Obes Relat Dis. 2017;13(8):1306–12.
Sanchez-Pernaute A, Rubio MA, Cabrerizo L, et al. Single-anastomosis duodenoileal bypass with sleeve gastrectomy (SADI-S) for obese diabetic patients. Surg Obes Relat Dis. 2015;11(5):1092–8.
Enochs P, Bull J, Surve A, et al. Comparative analysis of the single-anastomosis duodenal-ileal bypass with sleeve gastrectomy (SADI-S) to established bariatric procedures: an assessment of 2-year postoperative data illustrating weight loss, type 2 diabetes, and nutritional status in a single US center. Surg Obes Relat Dis. 2020;16(1):24–33.
Shoar S, Poliakin L, Rubenstein R, et al. Single anastomosis duodeno-Ileal switch (SADIS): a systematic review of efficacy and safety. Obes Surg. 2018;28(1):104–13.
King N. Amino acids and the mitochondria. In: Schaffer SW, Suleiman MS, editors. Mitochondria: the dynamic organelle. New York: Springer New York; 2007. p. 151–66.
Acknowledgments
Authors would like to thank the Senior Nurse Sandra Tavares (Centro Hospitalar de Entre o Douro e Vouga, Santa Maria da Feira, Portugal) for her technical assistance during the MMTT.
Funding
Unit for Multidisciplinary Research in Biomedicine (UMIB) is funded by Foundation for Science and Technology (FCT) Portugal (UID/Multi/00215/2019). JJH holds an unrestricted grant from the NNF Center for Basic Metabolic Research, Copenhagen, Denmark. The NNF foundation Center for Basic Metabolic Research is an independent research institution at the University of Copenhagen, Denmark.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pereira, S.S., Jarak, I., Carvalho, R.A. et al. Different Malabsorptive Obesity Surgery Interventions Result in Distinct Postprandial Amino Acid Metabolomic Signatures. OBES SURG 30, 4019–4028 (2020). https://doi.org/10.1007/s11695-020-04774-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04774-z