Abstract
Purpose
Laparoscopic sleeve gastrectomy (LSG) is an effective bariatric procedure, yet can be followed by complications such as staple line leak and bleeding, vomiting, and gastroesophageal reflux disease (GERD). Various attempts have been described in the literature to improve the early outcome of LSG through various measures. This study aimed to assess the impact of adding T-shaped omentoplasty to LSG on the short-term outcome of the procedure.
Methods
This was a retrospective cohort study on patients with morbid obesity who underwent LSG in the period of November 2015 to November 2018. The outcome of patients with morbid obesity who underwent LSG combined with T-shaped omentoplasty (group I) was compared with that of a similar number of patients who underwent classical LSG without staple line fixation (group II). The main outcome measures were the rates of staple line bleeding and leak, postoperative nausea and vomiting (PONV), GERD, gastric axial rotation, other complications, and weight loss.
Results
The study included 106 patients of a mean BMI of 49.8 kg/m2. Group II had significantly higher PONV) scale at 1 week and 1 month than group I. Group I had significantly lower rates of staple line bleeding (0 vs 9.6%, p = 0.02) and GERD (3.7% vs 17.3%, p = 0.02) than group II. Both groups had similar rates of staple line leak and comparable operation time.
Conclusion
Staple line fixation using the T-shaped omentoplasty technique was associated with lower incidence of significant PONV, staple line bleeding, and GERD as compared with classical LSG.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laparoscopic sleeve gastrectomy (LSG) has become one of the most popular bariatric procedures [1]. In addition to the satisfactory weight loss induced by LSG, the procedure also tends to induce improvement in several obesity-related comorbidities. However, some potentially serious complications of LSG have been reported, including staple line bleeding and leak [2].
According to a recent literature review, the average rates of staple line bleeding and leak are about 2% and 2.2–2.4%, respectively [3]. Several attempts have been made to minimize the incidence of staple line complications. Sleeve fixation is a novel technique proposed by Godoy and Coleho [4] to reduce staple line complications after LSG. Abdallah and co-workers [5, 6] concluded that staple line inversion and distal fixation can prevent staple line bleeding and gastric axial rotation after LSG.
In the present study, we aimed to assess the short-term results of plication of the staple line of sleeve gastrectomy combined with fixation of the distal part of the staple line to the root of the transverse mesocolon and greater omentum after reconstructing it in a T-shape manner as compared with the classical LSG.
Patients and Methods
Study Design and Setting
This was a retrospective cohort study of prospectively collected data of patients with morbid obesity who underwent LSG in the period of November 2015 to November 2018. The study was conducted at the General Surgery Department of Ain Shams University Hospitals and private hospitals. Ethical approval for the study was obtained from the Research Ethics Committee.
Selection Criteria
We included adult patients aged less than 60 years presenting with primary morbid obesity. Patients with secondary obesity due to endocrine disorders, patients who underwent previous bariatric procedures, patients with major psychiatric disorders, and pregnant women were excluded.
Preoperative Assessment
A detailed history about the onset, duration, and previous management of obesity was taken from the patients. Clinical examination including general and abdominal examination was conducted. Body weight and height were recorded and BMI was calculated. Routine laboratory investigations were ordered and abdominal ultrasonography and ECG were performed routinely. All patients underwent esophagogastroduodenoscopy to assess the state of the esophagus and stomach before surgery. Only patients who complained of clinical symptoms of GERD were assessed with pH metry.
Decision Making
The decision to undergo classical SG or the modified procedure was based on shared decision-making that involved the patient, surgeons, dietitian, and a physician after explaining the nature, potential benefits, and complications of each procedure. The procedures in the two groups were performed in contemporary timelines by different surgeons with sufficient experience with LSG.
Operative Technique
Written informed consents to undergo the procedure were taken from the patients. All procedures were conducted under general anesthesia with patients placed in the supine position with splitting of the legs. The same anesthetic technique was used in both groups. Induction was made using propofol (1–2 mg/kg), rucronium (0.5–1 mg/kg), fentanyl (1 μg/kg), and Dormicum (0.05 mg/kg). Maintenance of anesthesia was done using isoflurane (1–1.2 mac) with oxygen to air ratio of 1:2. Recovery from anesthesia was done by reversal of the effect of muscle relaxant using neostigmine (0.02–0.04 mg/kg).
The procedures were performed in a standardized step-wise manner by bariatric surgeons who had sufficient experience with LSG. One gram of cefotaxime was administered intravenously on induction as prophylactic antibiotic.
Classic Laparoscopic Sleeve Gastrectomy
A standard five-trocar technique was used. Using LigaSure device, dissection started with opening of the greater omentum about 4 cm proximal to the pylorus, then continued towards the gastroesophageal junction. The left crus was completely freed of any adhesions to avoid leaving a posterior pouch.
After insertion of 38 French bougie, gastric transection started 4 cm proximal to the pylorus along the greater curvature using 60-mm manual endo-staplers (Echelon, Ethicon, USA). Firstly, two 4.1-mm cartridges were fired, then two 3.8-mm cartridges followed by one or two 3.5-mm cartridges in the direction of the gastroesophageal junction to complete gastric transection. Symmetrical stapling of the anterior and posterior gastric walls was confirmed to avoid gastric axial rotation.
Upon completion of gastric transection, the staple line was carefully inspected, making sure the blood pressure of the patient was within the normal range. If bleeding points were noted, hemostasis was then carried out using clips. Inversion of the staple line was not performed in the classical sleeve group, neither was buttress material used.
Laparoscopic Sleeve Gastrectomy with T-Shaped Omentoplasty Fixation
The gastroesophageal pad of fat was completely removed to allow good exposure of the gastroesophageal junction. After completion of sleeve resection, inversion, and fixation of the distal end of the staple line was performed using interrupted 2/0 Ticron™ suture over a 26-mm round-body needle.
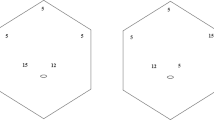
The anterior and posterior walls of the antrum were affixed to the mesocolic fat below the pancreas and to the edge of the free distal omentum close to the antrum. As the fixation proceeded upwards, the omentum was getting farther and heavier; therefore, we shortened the greater omentum with a stitch in a T-shaped manner (Fig. 1) resulting in an omental window between the two edges of the greater omentum. The bougie was partially withdrawn from the stomach just before performing the T-shaped omentoplasty.
Plication and combined fixation using interrupted sutures were continued upwards until the lower border of the pancreas. Finally, we plicated the gastric tube using continuous 2/0 Ticron™ suture starting from the proximal part near the angle of His until reaching the proximal end of interrupted suture line making sure the upper part of the gastric pouch was fitting over the bougie and the diameter of incisura was about 3 cm. Finally, the omental window was closed by sutures. None of the patients underwent concomitant surgery for hiatus hernia repair or other concomitant procedures in either group.
Postoperative Care
Pain control was achieved using non-steroidal anti-inflammatory medications applying analgesia on demand protocol. Postoperative nausea and vomiting (PONV) was assessed with PONV impact scale [7] at 24 h postoperatively. The PONV impact scale consists of two questions with total points of 0–6 and a score ≥ 5 defines clinically important PONV. PONV was treated with a single dose of intravenous (IV) 4 mg ondansetron (Zofran®). A single IV dose of 4 mg dexamethasone (Epidron®) was added as a second line treatment.
Prophylactic measures to prevent venous thromboembolism (VTE) were taken and included wearing an elastic compression stocking, early ambulation after surgery, adequate hydration, and subcutaneous injection of 2.5 mg fondaparinux sodium (Arixtra®, GlaxoSmithKline K.K., USA) within 12 h after surgery.
Clear oral fluids were allowed in the first 3 days, then purred diet was started for 1 week. Subsequently, semisolid diet was started for 1 or 2 weeks then normal diet was resumed with special instructions. Patients were asked to quit smoking for 4 weeks before surgery and to abstain from smoking in the postoperative period.
All patients were prescribed proton pump inhibitors (pantoprazole, 40 mg once per day) for 3 months after surgery. Additional medications were prescribed according to each patient’s condition and included antiemetic medications, analgesics, antidiabetic, and antihypertensive drugs in patients with type II DM and hypertension.
Follow-up
Patients were followed up in the outpatient clinic at 1 week then at 1, 3, 6, and 12 months postoperatively. PONV was assessed with PONV impact scale at 1 week and 1 month after surgery. The percentage of total weight loss (%TWL), decrease in BMI, and improvement in comorbidities were recorded at 12 months postoperatively. In addition, other complications were recorded.
Patients who reported clinical symptoms of GERD (n = 11) were assessed using GERD-Q questionnaire and was confirmed by endoscopy and 24-h pH study. Symptom questionnaires for GERD and PONV were collected by surgical residents who were unaware of the technique of surgery.
Study Outcomes
The primary outcome of the study was the PONV. Secondary outcomes included staple line complications, operation time, hospital stay, %TWL, improvement in comorbidities, GERD, and other complications. %TWL was calculated as [(preoperative weight − weight at 12 months)/preoperative weight] × 100. Improvement in comorbidities was defined according to the standardized outcomes reporting in metabolic and bariatric surgery [8].
Sample Size Calculation
The sample size of the study was based on the primary endpoint (incidence of PONV). In light of previous studies that reported the incidence of vomiting after LSG to range from 20 to 30% [5,6,7], and assuming that the T-shaped omentoplasty fixation technique will result in a reduction in postoperative vomiting by 20%, a minimum of 98 patients equally divided into two groups were needed to achieve study power of 80% with alpha set at 5%.
Statistical Analysis
Data were analyzed using SPSS version 25 program (IBM Corp., Chicago, USA). Quantitative data were analyzed using student’s t test, whereas qualitative data were processed by chi-square test or Fisher’s exact test. P value less than 0.05 was considered significant.
Results
Patients’ Demographics
The study included 106 patients of a mean age of 34.1 ± 7.8 years. Patients were 69 (65.1%) female and 37 (34.9%) male. The mean preoperative body weight was 144.3 ± 26.9 kg, the mean height was 170.2 ± 9.5 cm, and the mean baseline BMI was 49.8 ± 8.5 kg/m2. There were 12 patients with type 2 DM, 12 with hypertension, and five with hyperlipidemia.
Patients were divided according to the technique of surgery into two groups, group I entailed LSG with T-shaped omentoplasty fixation technique (n = 54) and group II entailed classical LSG (n = 52). There were no significant differences between the two groups in regards age, sex, preoperative weight, height, BMI, and comorbidities (Table 1).
Weight Loss and Improvement in Comorbidities
Both groups showed significant decrease in BMI at 3, 6, and 12 months postoperatively as compared with the baseline BMI. There were no significant differences between the two groups in terms of BMI at 3, 6, and 12 months or %TWL at 12 months (34.5% Vs 32.6%, p = 0.21). Improvement in comorbidities at 12 months postoperatively was comparable in the two groups (Table 2).
Complications
Both groups had comparable operation time with no significant difference (66.4 vs 58.7 min, p = 0.05). Group I had significantly lower rates of staple line bleeding (0 vs 9.6%, p = 0.02) and GERD (3.7% vs 17.3%, p = 0.02) as compared with group II. Both groups had similar rates of staple line leak (Table 3).
Staple line bleeding was recorded in five patients, all were in group II. Postoperative staple line bleeding was diagnosed based on clinical data (tachycardia and hypotension), decreased serum hemoglobin levels, drainage of excess amount of blood in the drain (if a drain was placed), and detection of free intraperitoneal fluid in abdominal ultrasound. Among the patients who developed staple line bleeding, two required blood transfusion and one required laparoscopic assessment and hemostasis by clipping of the bleeding points.
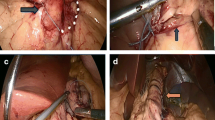
Nine patients in group II had significant persistent vomiting at 1 month after surgery and were investigated with upper GI series (gastrografin meal) (Fig. 2) and gastroscopy, three of whom were diagnosed with partial axial rotation and were managed with endoscopic balloon dilatation. As for the remaining six patients with persistent vomiting, they were treated conservatively with antiemetic and prokintic medications and five of whom showed complete resolution of symptoms after 3 months of treatment whereas the remaining patient had partial improvement in symptoms at 3 months yet on continuing medical treatment and adjusting life-style and diet she reported complete resolution of symptoms at 5 months after surgery.
PONV
The median PONV impact scale in group I was 3 (range, 1–6), 1 (range, 0–6), and 0 (range, 0–5) at 24 h, 1 week, and 1 month after surgery. The median PONV impact scale in group II was 4 (range, 1–6), 2 (range, 0–6), and 1 (range, 0–6) at 24 h, 1 week, and 1 month after surgery.
The perecntage of patients with significant PONV impact scale at 24 h was similar in the two groups (25.9% versus 30.7%; p = 0.73). However, at 1 week and 1 month postoperatively, the percentage of patients with significant PONV impact scale in group I was less than group II (5.5 vs 26.9%; p = 0.003) and (1.8% vs 17.3%; p = 0.007), respectively.
While there was no significant difference between the two groups regarding PONV impact scale at 24 h postoperatively, group II had significantly higher PONV scale at 1 week and 1 month as compared to group I (Table 4).
Discussion
The present study compared patients who underwent LSG and T-shaped omentoplasty with a matched cohort of patients who underwent classical LSG. Although this study was not a randomized clinical trial, the adequate matching of the two groups served to minimize the risk of bias.
The T-shaped omentoplasty technique entailed two essential components. Firstly, we reinforce and invert the staple line by oversewing it with sutures, this staple line reinforcement may help reduce staple line complications [9]. Secondly, we affix the distal part of the staple line to the root of the tranverse mesocolon and the free edges of the greater omentum in a T-shaped manner. The distal staple line fixation serves to hold the gastric pouch in place and avoid partial or complete axial twisting of the gastric pouch.
In line with another study [10], patients who had staple line fixation using T-shaped omentoplasty had significantly less vomiting at 1 week and 1 month postoperatively and lower rates of staple line bleeding, partial axial rotation, and GERD than classical LSG. Both groups had similar rates of staple line leak which may be attributed to the small numbers of patients in our study. The rate of bleeding in the present study is higher than the reported average after LSG and this might be attributed to either bleeding from the staple line or the greater omentum. Staple line bleeding might be due to stapler malfunction that did not allow full compression of the gastric tissues or patient-related factors such as postoperative rise in blood pressure in patients with hypertension. Another reason that may explain the rate of bleeding is that all five cases of bleeding were in the classical sleeve group in which routine staple line reinforcement with oversewing or buttressing was not performed.
Moreover, T-shaped omentoplasty managed to decrease the incidence of PONV significantly as compared to the classical LSG. This finding may be explained by improvement in gastric emptying which may get compromised after LSG as reported in some studies [11, 12]; however, other studies [13, 14] found SG accelerates gastric emptying. T-shaped omentoplasty may also help prevent partial or complete axial rotation of the gastric pouch. Axial rotation of the gastric pouch is mostly attributed to asymmetrical stapling of the stomach which leads to rotation of the gastric pouch. Axial rotation maybe also attributable to the nature of the procedure, leaving a long tubular gastric pouch with no supportive ligaments or omentum, thus distension of the gastric pouch by food may lead to axial rotation [15].
Partial axial rotation occurred in about 6% of patients in the classical LSG group whereas none of the patients in the T-shaped omentoplasty group developed axial rotation. Presumably, staple line fixation to the omentum helped restore the anatomic support of the stomach by the greater omentum, thus reduced the incidence of gastric twist and vomiting.
GERD is a frequent sequel of LSG. T-shaped omentoplasty was associated with lower rate of postoperative GERD than classical LSG. This corroborates the notion that loss of ligament fixation along the greater curvature of the stomach may lead to proximal migration of the gastric pouch, inducing significant GERD [16]. Therefore, restoring the anatomic orientation and fixation of the gastric pouch using T-shaped omentoplasty may have served to reduce the incidence of GERD by avoiding pouch migration.
Strengths of the present study include the introduction of a novel technique to reduce PONV, staple line complications, and axial rotation of the stomach. In order to highlight the beneficial impact of the T-shaped omentoplasty technique, a historical control group of classical LSG was compared. Limitations of the present study include its retrospective nature, relatively small number of patients included, and short-term follow-up. The study may be associated with the risk of selection bias because the selection and assignment of patients to each group was made after shared decision-making and was not random. Therefore, future well-designed randomized trials comparing LSG with T-shaped omentoplasty and conventional LSG are needed to ascertain the results of this study.
Conclusion
Patients who underwent LSG with staple line fixation using the T-shaped omentoplasty technique experienced lower rates of postoperative vomiting, staple line bleeding, and GERD when compared with traditional LSG.
References
Emile SH, Elfeki H, Elalfy K, et al. Laparoscopic sleeve gastrectomy then and now: an updated systematic review of the progress and short-term outcomes over the last 5 years. Surg Laparosc Endosc Percutan Tech. 2017;27(5):307–17. https://doi.org/10.1097/SLE.0000000000000418.
Alizadeh RF, Li S, Inaba CS, et al. Robotic versus laparoscopic sleeve gastrectomy: a MBSAQIP analysis. Surg Endosc. 2019;33(3):917–22. https://doi.org/10.1007/s00464-018-6387-6.
Iannelli A, Treacy P, Sebastianelli L, et al. Perioperative complications of sleeve gastrectomy: review of the literature. J Minim Access Surg. 2019;15(1):1–7. https://doi.org/10.4103/jmas.JMAS_271_17.
Godoy E, Coelho D. Gastric sleeve fixation strategy in laparoscopic vertical sleeve gastrectomy. ABCD Arq Bras Cir Dig. 2013;26(Suplemento 1):79–82.
Abdallah E, Emile SH, Elfeki H. Laparoscopic sleeve gastrectomy with or without staple line inversion and distal fixation to the transverse mesocolon: impact on early postoperative outcomes. Obes Surg. 2017;27(2):323–9.
Myles PS, Wengritzky R. Simplified postoperative nausea and vomiting impact scale for audit and post-discharge review. Br J Anaesth. 2012;108(3):423–9.
Brethauer SA, Kim J, El Chaar M, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Obes Surg. 2015;25(4):587–606.
Ruiz-Tovar J, Zubiaga L, Muñoz JL, et al. Incidence of postoperative nausea and vomiting after laparoscopic sleeve gastrectomy with staple line reinforcement with oversewing and staple line inversion vs buttressing material: a randomized clinical trial. Int J Surg. 2018;59:75–9. https://doi.org/10.1016/j.ijsu.2018.09.010.
Elbalshy MA, Fayed AM, Abdelshahid MA, et al. Role of staple line fixation during laparoscopic sleeve gastrectomy. Int Surg J. 2018;5:156–61.
Santoro S. Technical aspects in sleeve gastrectomy. Obes Surg. 2007;17(11):1534–5.
Fallatah B, Shehry A, Abdelsamad L, et al. Comparison study of gastric emptying after performing sleeve gastrectomy with two different techniques. Glob J Surg. 2013;1(4):53–6.
Braghetto I, Davanzo C, Korn O, et al. Scintigraphic evaluation of gastric emptying in obese patients submitted to sleeve gastrectomy compared to normal subjects. Obes Surg. 2009;19(11):1515–21.
Sista F, Abruzzese V, Clementi M, et al. The effect of sleeve gastrectomy on GLP-1 secretion and gastric emptying: a prospective study. Surg Obes Relat Dis. 2017;13(1):7–14.
Vives M, Molina A, Danús M, et al. Analysis of gastric physiology after laparoscopic sleeve gastrectomy (LSG) with or without antral preservation in relation to metabolic response: a randomised study. Obes Surg. 2017;27:2836–44.
Emile SH. Gastroesophageal reflux disease after sleeve gastrectomy: the need to predict its onset and prevent its consequences. Obes Surg. 2019 Aug;29(8):2625–6.
Baumann T, Kuesters S, Grueneberger J, et al. Time-resolved MRI after ingestion of liquids reveals motility changes after laparoscopic sleeve gastrectomy--preliminary results. Obes Surg. 2011;21(1):95–101.
Author information
Authors and Affiliations
Contributions
Emad Abdallah designed the study. Emad Abdallah, Mahmoud Zakaria, Mahmoud Abdelnaby, Sabry Mahmoud, Waleed Gado, and Samy Elbaz followed the patients, collected the data, and critically revised the manuscript. Sameh Emile and Mohamed Fikry participated in data collection and analysis and writing and revision of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Ethical approval for the study was obtained from the Research Ethics Committee.
Statement of Informed Consent
Informed consent does not apply as for this type of study; formal consent is not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abdallah, E., Zakaria, M., Fikry, M. et al. Laparoscopic Sleeve Gastrectomy with T-Shaped Omentoplasty: Impact on the Early Postoperative Outcomes. OBES SURG 30, 3735–3741 (2020). https://doi.org/10.1007/s11695-020-04743-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04743-6