Abstract
Background
Some weight regain is expected after bariatric surgery; however, this concept is not well defined. A favorable weight loss response has commonly been defined as 50% excess weight loss (EWL). The medical literature uses %total weight loss (%TWL), which has recently been adopted in some surgical literature.
Objective
To demonstrate variability in bariatric surgery outcomes based on the definition applied and propose a standardized definition.
Methods
A retrospective review of patients who underwent bariatric surgery from 2001 to 2016 with ≥ 1 year follow-up was completed. Several previously proposed definitions of weight regain were analyzed.
Results
One thousand five hundred seventy-four patients met inclusion criteria. Preoperative mean body mass index (BMI) was 47.6 ± 6.4 kg/m2. Increased preoperative BMI was associated with increased mean %TWL at 2 years postoperative (29.3 ± 9.1% for BMI < 40, vs. 37.5 ± 9.5% for BMI > 60; P < 0.001). Based on %EWL, 93% of patients experienced ≥ 50% EWL by 1–2 years, and 61.8% maintained ≥ 50% EWL through the 10-year follow-up period. Similarly, 97% experienced ≥ 20% TWL by 1–2 years and 70.3% maintained ≥ 20% TWL through the 10-year follow-up period. Over 50% of patients maintained their weight based on several proposed definitions through 5 years follow-up.
Conclusions
A high percentage (> 90%) of patients achieve ≥ 20% TWL and ≥ 50% EWL. Increased preoperative BMI was associated with increased %TWL and decreased %EWL at 2 years postoperative. The incidence of weight regain varies depending on the definition. We propose a standardized definition for identifying good responders following bariatric surgery to be ≥ 20% TWL, as this measure is least influenced by preoperative BMI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past several decades, various bariatric operations have been used and can be extremely effective tools in helping patients achieve the goals of significant and sustained weight loss, comorbidity risk reduction, quality of life improvement, and treatment of metabolic illness [1, 2].
As more research is occurring in this field of obesity, we are beginning to understand that obesity is a chronic disease. There are variable outcomes with both medical and surgical treatments. The concept of success and/or failure may be outdated. Defining outcomes may better be described as good responders and poor responders. Because obesity is a chronic disease, there are patients who initially have a good response with treatment, but over time the disease returns. There are many factors that contribute to this, many of which are likely out of the patients’ control or influence. The measures and definition of weight loss and weight regain are not well understood. Favorable outcomes following bariatric surgery can be determined in a variety of ways including improvements in obesity-related comorbidities, quality of life, and weight loss. Various definitions have been used in the bariatric literature to report weight loss and define outcomes with regard to weight loss and weight regain. Some of the proposed definitions include total weight loss (TWL), percent total weight loss (%TWL), percent excess weight loss (%EWL), and change in body mass index (BMI) (Table 1). There are advantages and disadvantages to each definition, and it has been shown that preexisting patient factors such as T2D, mental health issues, and preoperative BMI will affect the outcome measures for many patients [3, 4]. Previous reports have proposed standard definitions for outcome reporting in bariatric surgery in an effort to address difficulties in interpreting and comparing outcomes [5].
Markers for identifying a favorable response to surgery have been extensively evaluated over the past decade. There is no clear consensus on what metric should be used to define a good or poor response in relation to weight loss and weight regain. Some proposed definitions for weight regain in the literature include BMI increase to ≥ 35 kg/m2 after experiencing a BMI ≤ 35 kg/m2, weight regain of > 25% EWL over nadir, EWL < 50% after experiencing ≥ 50% EWL, and maintaining > 20% TWL. Several authors claim %TWL may be the most accurate metric for assessing weight loss across the bariatric population. They have reported that %TWL is the least influenced by confounding anthropometric factors, and it can be compared with behavioral and pharmacological series reported in the medical literature, which commonly use %TWL. It has also been noted to be easier to calculate, comprehend, and explain to patients [2, 4, 6].
Given the variability in reported measures of weight loss and weight regain, the primary objective of this study was to apply the common definitions used in the literature to our patient population to evaluate the variability in outcomes based on different definitions of weight loss following bariatric surgery. We also sought to propose a standard definition.
Methods
A retrospective review of our institution’s prospective bariatric surgery registry was completed to identify all patients who underwent laparoscopic Roux-en-Y gastric bypass (LRYGB) or laparoscopic sleeve gastrectomy (LSG) from September 2001 through December 2016. Patients with less than 1 year of follow-up data were excluded from analysis. Postoperative weights were obtained through our integrated multispecialty health system’s electronic medical record. Several definitions of weight loss and weight maintenance were evaluated over the long-term (10-year) follow-up period, including several definitions identified by Nedelcu and colleagues [7] and Corcelles and colleagues [6]: (1) BMI increase to ≥ 35 kg/m2 after experiencing a BMI ≤ 35 kg/m2, (2) weight regain of > 25% EWL over nadir, (3) EWL < 50% after experiencing ≥ 50% EWL, as well as (4) maintenance of TWL ≥ 20%. Ideal body weight used to calculate %EWL was defined as the weight that corresponds to a BMI of 25 kg/m2 [5]. The proportion of patients who met these definitions of weight maintenance was analyzed, along with patients’ mean weight loss. Univariate tests of association between patient demographics and weight loss outcomes included χ2, Wilcoxon rank sum, and Kruskal-Wallis tests. To control for potential confounding effects of demographic and clinical factors, multivariate linear regression models of %EWL and %TWL at 2 and 5 years postoperative were also construed. All statistical analysis was performed using SAS 9.4 (Cary, NC).
Results
Overall, 1766 patients underwent bariatric surgery; 1574 met inclusion criteria. Of those, 1355 underwent LRYGB and 219 underwent LSG. Preoperative mean age and BMI were 44.9 ± 10.3 years and 47.6 ± 6.4 kg/m2, respectively; 80.9% were female. Preoperatively, 557 (35.4%) patients had T2D, 1079 (68.6%) had dyslipidemia, and 939 (59.7%) had hypertension. The median operative time was 146 (interquartile range 127–164) minutes, and mean length of stay was 2.2 ± 1.1 days. The lowest mean BMI, maximum mean %EWL, and mean %TWL were reached between 1 and 2 years follow-up at 30.2 ± 5.4 kg/m2, 79.6 ± 20.9%, and 36.4 ± 8.6%, respectively. Overall, 1395 of 1496 patients (93.2%) with complete data experienced ≥ 50% EWL and 1450 of 1496 (96.7%) experienced ≥ 20% TWL by 1–2 years postoperative. The mean %TWL was 34.2 ± 9.7% at 2 years postoperative and decreased to 25.1 ± 11.8% at 10 years postoperative (Fig. 1). Over 50% of patients with complete data maintained their weight based on several of the proposed definitions of weight regain through 5 years postoperative (Table 2).
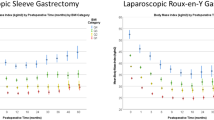
When stratified by preoperative BMI, 162 (9.2%) had a preoperative BMI < 40.0 kg/m2, 545 (30.9%) had a preoperative BMI between 40.0 and 44.9 kg/m2, 508 (28.8%) had a preoperative BMI 45.0–49.9 kg/m2, 319 (18.1%) had a preoperative BMI 50.0–54.9 kg/m2, 144 (8.2%) between 55.0 and 59.9 kg/m2, and 85 (4.8%) had a preoperative BMI ≥ 60 kg/m2. Patients with a preoperative BMI ≥ 40 kg/m2 experienced a significantly greater %TWL at 2 years postoperative compared to those with a preoperative BMI < 40 kg/m2 (Fig. 2a). Mean %EWL and BMI changes were significantly different when stratified by preoperative BMI at each annual postoperative interval through 10 years postoperative (Fig. 2b, c). The %TWL measure demonstrated less variability based on preoperative BMI as compared to %EWL and change in BMI.
In a multivariate linear regression model, at 2 years postoperative, factors that were independently associated with increased %TWL included absence of preoperative T2D, female sex, age < 40 years, preoperative BMI ≥ 40 kg/m2, and LRYGB procedure (Table 3). At 5 years postoperative, only LRYGB, female sex, and preoperative BMI 40–49 kg/m2 remained significant factors for increased %TWL (Table 3). Using the same variables in a model for %EWL, factors that were associated with increased %EWL at 2 years postoperative included absence of preoperative T2D, absence of preoperative HTN, female sex, age < 40 years, preoperative BMI < 40 kg/m2, and LRYGB (Table 4). At 5 years postoperative, predictors of increased %EWL were LRYGB procedure, preoperative BMI < 40 kg/m2, and female sex (Table 4).
Discussion
Goals of bariatric surgery include quality of life improvement, comorbidity risk reduction, remission and improvement in metabolic disease, and weight loss. Many of these factors have been extensively studied and are well defined in the literature. There are established metrics for defining improvement and remission of obesity-related comorbidities [5], and multiple quality of life questionnaires that aid in defining a good response to bariatric surgery. The concept of weight regain has not been well defined and there is no standard found in the literature. There are many ways to evaluate how a patient responds to bariatric surgery; however, the focus of this study was to apply several of the commonly used definitions of weight loss that are already found in the literature and determine which metric could be established as a standard.
Weight loss has been reported in many ways; however, the best method should allow for the most accurate comparisons between the broadest ranges of patients’ weight and population characteristics [1]. In 1982, Dr. Reinhold published one of the flagship studies using the definition of > 50% EWL as a “good” bariatric weight loss result [8]. He cited data published by Dr. Seltzer which indicated that patients from a non-bariatric surgery population with “30% excess weight” above the average had a sharp increase in mortality [8, 9]. This benchmark permeated the bariatric literature and, despite its inherent flaws, remained the standard for decades. Subsequent research has found that perhaps %TWL was a more appropriate marker for weight loss. This conclusion was based on the results of multiple studies which showed that other parameters, such as %EWL and %EBMIL, had greater variability related to preoperative BMI [1, 2, 4, 6, 10]. Corcelles et al. used this information to create a definition of > 20% TWL as a “successful result” in the first year after surgery [6]. This definition was founded on the evidence that there is improvement of obesity-related comorbidities and cardiovascular risk factors with a weight loss of 5–10% [11,12,13]. Recent research has focused on long-term reporting and weight maintenance after bariatric surgery. In 2016, Nedelcu et al. published results from a public forum used to survey bariatric surgeons on what they believed was the most appropriate definition for weight regain [7]. These definitions included, but are not limited to regaining weight to achieve a BMI > 35 kg/m2, weight regain greater than 25% EWL over nadir, and EWL < 50% after experiencing ≥ 50% EWL with respect to minimal weight achieved after LSG. They concluded that there is a need for standardized definitions of weight regain.
The best description of a positive weight loss result after bariatric surgery would be an all-inclusive, easy to calculate, comprehend, and convey definition based on robust data from a large sample size. To date, there is no single best definition of weight regain or weight loss. Each of the above-mentioned definitions carry inherent shortcomings and biases. Many of these are biased towards patients with lower preoperative BMIs, but are reasonable metrics to consider.
It is impressive that 97% of patients achieved at least 20% TWL at some point in the postoperative period with a mean of 34% TWL at nadir. The spectrum of weight loss outcomes varies widely based off of the definition used to define good or poor response and regain. At 10 years postoperative, in the same cohort of patients, this ranges from 48.4 to 70.3% solely determined by the definition applied (Table 2). Our medical colleagues routinely use %TWL to define a good response with their treatment modalities. A benchmark of 5% TWL is typically used with pharmacotherapy [14, 15]. It has been shown that patients who achieve 5–10% TWL have significant reduction of obesity-related comorbidities [11,12,13]. By applying %TWL to define a good response to weight loss after surgery, we are able to communicate in the same language as our medical colleagues and show that surgery provides excellent long-term outcomes. By this proposed definition, bariatric surgery provides four times the weight loss at 10 years that current pharmaceutical intervention does in the short term. A common concern among prospective patients, providers, and payers is the lack of long-term durable weight loss. To the contrary, these data show that a majority of patients are able to keep a substantial portion of their weight off throughout the long-term follow-up period.
The effect of preoperative BMI on weight regain depends on the terms used to define it. Three such examples are depicted in Fig. 2, demonstrating the weight regain curves of patients as represented by the definitions of %TWL, %EWL, and BMI loss. Based on these definitions, our data confirmed that the definition that conferred the least variability when stratified by preoperative BMI was %TWL. Body mass index and %EWL are noted to have significantly more variability with regard to preoperative BMI, suggesting that %TWL may be a better measure. Initial BMI loss was significantly greater in the groups with higher preoperative BMIs in our series. This trend continued throughout our long-term follow-up period. Conversely, a good response under the parameter of %EWL favors those patients with lower initial preoperative BMIs. Due to these findings, we recommend the routine use of %TWL as the standard metric to track long-term weight regain after bariatric surgery.
The authors suggest that %TWL be used to quantify weight loss and propose that ≥ 20%TWL become the accepted benchmark to identify those who are good responders to weight loss surgery along with reporting of remission or improvement of obesity-related comorbidities such as T2D and hyperlipidemia. It is one of the simplest ways to comprehend, calculate, and explain to both colleagues and patients. As discussed, this metric minimizes one of the largest confounding factors that have affected most of the other definitions, preoperative BMI. This metric is used in the medical literature; therefore, using it in the surgical literature as well allows for consistent comparison and improved understanding of surgical outcomes for our medical colleagues.
Strengths of this paper include the long-term study period, with results through 10 years postoperative from a single-center integrated multispecialty electronic health record system. No self-reported data were used. Additional strengths include the large sample size, low attrition rate, and long-standing bariatric program with consistent surgical technique among all surgeons. Limitations of this study include its design as a single-center, retrospective review of a fairly homogenous population. Stratification by procedure type (LRYGB and LSG) were completed only for the multivariate regression model due to decreased follow-up duration in the LSG group. There was a lack of control for patient compliance, dieting, physical activity, and use of other weight loss adjuncts. In addition, application of this proposed benchmark to other bariatric procedures and interventions has yet to be performed, and further data from large, multicenter databases is needed.
Conclusions
The %TWL resulted in the least variability when stratified by various preoperative patient characteristics and should be considered as a standard metric to assess response to weight loss and weight regain. Over a long-term follow-up period, 70% of patients maintained ≥ 20% TWL. A lower preoperative BMI, preoperative T2D or hypertension, age greater than 40 years, and male sex were associated with reduced %TWL in the early postoperative period. Thus, we would expect improved short- and long-term results with earlier intervention. This information can be used in counseling patients on postoperative expectations for both short- and long-term weight loss. We propose that ≥ 20% TWL be considered as a measure to identify patients that are good responders to bariatric surgery. Further validation of this measure with a larger sample is needed.
References
Sczepaniak JP, Owens ML, Shukla H, et al. Comparability of weight loss reporting after gastric bypass and sleeve gastrectomy using BOLD data 2008-2011. Obes Surg. 2015;25(5):788–95.
van de Laar A, de Caluwe L, Dillemans B. Relative outcome measures for bariatric surgery. Evidence against excess weight loss and excess body mass index loss from a series of laparoscopic Roux-en-Y gastric bypass patients. Obes Surg. 2011;21(6):763–7.
de Hollanda A, Ruiz T, Jiménez A, et al. Patterns of weight loss response following gastric bypass and sleeve gastrectomy. Obes Surg. 2015;25(7):1177–83.
Hatoum IJ, Kaplan LM. Advantages of percent weight loss as a method of reporting weight loss after Roux-en-Y gastric bypass. Obesity (Silver Spring). 2013;21(8):1519–25.
Brethauer SA, Kim J, el Chaar M, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Surg Obes Relat Dis. 2015;11(3):489–506.
Corcelles R, Boules M, Froylich D, et al. Total weight loss as the outcome measure of choice after Roux-en-Y gastric bypass. Obes Surg. 2016;26(8):1794–8.
Nedelcu M, Khwaja HA, Rogula TG. Weight regain after bariatric surgery—how should it be defined? Surg Obes Relat Dis. 2016;12(5):1129–30.
Reinhold RB. Critical analysis of long term weight loss following gastric bypass. Surg Gynecol Obstet. 1982;155(3):385–94.
Seltzer CC. Some re-evaluations of the build and blood pressure study, 1959 as related to ponderal index, somatotype and mortality. N Engl J Med. 1966;274(5):254–9.
Lager CJ, Esfandiari NH, Subauste AR, et al. Milestone weight loss goals (weight normalization and remission of obesity) after gastric bypass surgery: long-term results from the University of Michigan. Obes Surg. 2017;27(7):1659–66.
Zhou YH, Ma XQ, Wu C, et al. Effect of anti-obesity drug on cardiovascular risk factors: a systematic review and meta-analysis of randomized controlled trials. PLoS One. 2012;7(6):e39062.
Aminian A, Jamal M, Augustin T, et al. Failed surgical weight loss does not necessarily mean failed metabolic effects. Diabetes Technol Ther. 2015;17(10):682–4.
Tuomilehto J, Lindstrom J, Eriksson JG, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344(18):1343–50.
Moyer VA. Screening for and management of obesity in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;157(5):373–8.
Carvajal R, Wadden TA, Tsai AG, et al. Managing obesity in primary care practice: a narrative review. Ann N Y Acad Sci. 2013;1281:191–206.
Acknowledgments
The authors gratefully acknowledge the grant support provided by the Foundation for Surgical Fellowships for the Minimally Invasive Bariatric Surgery and Advanced Laparoscopy Fellowship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
A HIPAA waiver of authorization was approved by our institution’s IRB.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Grover, B.T., Morell, M.C., Kothari, S.N. et al. Defining Weight Loss After Bariatric Surgery: a Call for Standardization. OBES SURG 29, 3493–3499 (2019). https://doi.org/10.1007/s11695-019-04022-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-04022-z