Abstract
Introduction
Metabolic surgery has become an accepted option for the treatment of obesity and associated metabolic diseases like hypertension and type 2 diabetes. Adipose tissue dysfunction and ectopic storage of excess lipids are thought to be involved in the underlying pathophysiological process.
Objectives
The present study aims to clarify the effect of sleeve gastrectomy (SG) on adipose tissue microvasculature and health in an animal model of adipose type 2 diabetes.
Methods
After weaning, diabetic Goto-Kakizaki rats were either fed on standard rat chow or high-calorie diet. At 4 months, animals on high-calorie diet were randomized to SG, sham surgery, or control group. Non-diabetic Wistar rats served as further controls. At 6 months, glucose and lipid metabolisms were studied in vivo. After sacrifice, periepididymal adipose tissue was collected for histology and analysis of parameters of adipose tissue metabolism and insulin sensitivity.
Results
SG decreased body and adipose tissue weight and improved glycemic and lipid profiles. Fasting glycemia, area under the curve after intraperitoneal insulin tolerance test, and insulin resistance were decreased in operated animals. SG also reduced circulating triglycerides and cholesterol while increasing serum adiponectin and adipose tissue peroxisome proliferator-activated receptor γ (PPAR-γ) and perilipin A. Additionally, surgery improved adipose tissue vascular function and markedly increased vascular endothelial growth factor, cluster of differentiation 31, and endothelial nitric oxide synthase.
Conclusions
In our obese animal model of type 2 diabetes, SG significantly improved adipose tissue health and angiogenesis while reducing insulin resistance, involving PPAR-γ and markers of sprouting angiogenesis and endothelial function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgical treatment of obesity and associated metabolic diseases has become a universally accepted option for a health problem that affects currently 650 million adults worldwide [1,2,3]. Long-term follow-up studies have shown that surgical treatment is not only effective in reducing excess weight but also moderates the prevalence and de novo incidence of associated diseases like type 2 diabetes and hypertension as well as cardiovascular mortality [4, 5]. Both sleeve gastrectomy and gastric bypass are effective in improving the control of hyperglycemia and in reducing the use of insulin in type 2 diabetic patients [6, 7]. Well-established mechanisms of action include the modified postprandial release of gut hormones that act on pancreatic beta cells and the central regulation of food intake and satiety [8,9,10,11]. Less is known regarding the effects of surgery on other pathophysiological processes that are essential for metabolic homeostasis.
In the presence of increased intake of nutrients, particularly fat and sugars, that exceed current metabolic needs, excess energy is typically stored in the form of triglycerides in adipose tissue. Recent research has shown that subsequently enlarged adipocytes will lead to relative tissue hypoxia that will drive local angiogenesis and adapting of extracellular matrix to meet existing requirements and permit further adipose tissue expansion. Whereas in healthy metabolic conditions, a new steady state will be achieved, extended excess intake of nutrients might lead to chronic hypoxia inducing unresolved inflammation, impaired angiogenesis, and fibrosis [12]. In consequence, subcutaneous fat is no longer able to adequately expand and store excess nutrients. Impaired angiogenesis is thought to play an important role in the context of inadequate subcutaneous adipose tissue expansion in response to nutrient excess leading to ectopic fat deposits in the liver, skeletal muscle, and cardiac muscle and accumulation of visceral adipose tissue. Besides being a marker for ectopic fat accumulation, secretion of inflammatory cytokines from visceral adipose may further induce insulin resistance in liver and skeletal muscle [13,14,15]. On the other hand, adequate angiogenesis and vascular remodeling in white adipose tissue will reduce secretion of cytokines, contribute to a metabolically healthy environment, and modulate insulin sensitivity [16].
In the face of the emerging evidence for adipose tissue dysfunction in the pathogenesis of type 2 diabetes, this experimental study aims to clarify the effects of the transformation of the gastrointestinal tract through metabolic surgery on adipose tissue microvasculature and function and insulin sensitivity.
Methods
Animals
After weaning, we obtained 1-month-old male diabetic Goto-Kakizaki (GK) and Wistar rats from our local breeding colonies. Animals were housed in a controlled environment with day-night cycles of 12 h, a temperature of 22–24 °C, and a relative humidity of 50–60%. Rats could feed freely on water and on either standard rat chow (AO3, Charles River, SAFE, France) or high-calorie diet (AO3-derived) enriched with sucrose (20%) and fat (20%) (HFD) (Charles River, SAFE, France), accordingly to randomization (see below).
Study Protocol
Eight non-diabetic Wistar rats were maintained on standard rat chow and 32 diabetic GK rats were randomly assigned to either standard rat chow (8 animals—GKSD) or HFD (24 animals). At the age of 4 months, rats on HFD were further randomized to either sleeve gastrectomy (GKHFDSl), sham surgery (GKHFDSh), or control group (GKHFD) and kept on HFD until sacrificed at 6 months (Fig. 1a) (reviewer#2, comment#3, and comment#5). At the age of 6 months, 2 months after sleeve gastrectomy or sham surgery, an intraperitoneal insulin tolerance test (IPITT) was carried out. Fasting glucose and lipid metabolism parameters were determined in blood from the tail vein. Subsequently, animals were sacrificed by cervical displacement and periepididymal white adipose tissue (pEAT) was collected, cleaned, weighted, and immediately stored (24 h in 10% formalin and EtOH 70% until paraffin inclusion) or frozen in liquid nitrogen to be stored at 80 °C to perform pEAT histology (Masson trichrome) or Western Blotting analysis.
Experimental design and glucose metabolism (a). Lower fasting glycemia (b) and area under the curve (c) and glycemia at 2 h (d) during the intraperitoneal insulin tolerance test in GK rats with diet-induced obesity submitted to sleeve gastrectomy. Sleeve gastrectomy also significantly decreased HOMA (e) and increased the levels of GLUT4 in the visceral adipose tissue measured by Western Blot (f). Representative Western Blots are shown in the right panel, calnexin was used as loading control. No significant alterations were observed in the expression and activation (phosphorylation at Tyr1161) of the insulin receptor. Wistar—Wistar 6 months old fed a standard diet; GKSD—Goto-Kakizaki 6 months old fed a standard diet; GKHFD—Goto-Kakizaki 6 months old fed a high-fat high-sucrose diet for 5 months; GKHFDSl—GKHFD submitted to sleeve gastrectomy at 4 months old; GKHFDSh—GKHFD submitted to sham surgery at 4 months old. Bars represent means ± SEM, n = 8 (n = 6 for Western Blots). * vs Wistar; # vs GKSD; $ vs GKHFD; & vs GKHFDSh. One symbol p < 0.05; two symbols p < 0.01; three symbols p < 0.001
Surgical Techniques
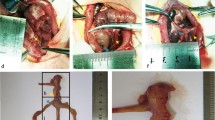
Rats in groups GKHFDSl and GKHFDSh were operated under intramuscular anesthesia using ketamine (75 mg/kg body weight, Pfizer Inc., New York, NY, USA) and chlorpromazine (3 mg/kg body weight, Laboratórios Vitória, Amadora, Portugal). After preparation of the abdomen, a midline incision was carried out. Sleeve gastrectomy was performed as described elsewhere [9, 17] and included the dissection of the greater curvature including the aglandular forestomach which was removed along with the operative specimen. The remaining stomach was closed in two layers using a 4/0 midterm absorbable synthetic glyconate monofilament thread (Monosyn®, B Braun, Aesculap AG, Tuttlingen, Germany). Sham-operated animals were submitted to explorative laparotomy while maintaining the abdomen exposed before closure for a similar period as animals submitted to sleeve gastrectomy. In both groups, the abdominal wall was closed using a running suture (3/0 short-term absorbable suture of braided and coated polyglycolic acid (Safil Quick®, B Braun, Aesculap AG, Tuttlingen, Germany), after rinsing the abdominal cavity with sterile saline and intraperitoneal administration of meloxicam (1 mg/kg body weight, Boehringer Ingelheim GmbH, Ingelheim, Germany). After surgery, operated animals (GKHFDSl and GKHFDSh) were kept under a liquid diet (Fortimel®, Nutricia, Lisbon, Portugal) with analgesia and prophylactic antibiotics until day 5 using meloxicam subcutaneously and doxycycline mixed to drinking water (5 mg/kg bodyweight, Pfizer Inc., New York, NY, USA).
Glucose and Lipid Metabolism
We assessed glucose metabolism and lipids in vivo at 6 months, before sacrifice. Cholesterol and triglycerides were measured in venous blood from the tail vein after a daytime fast of six hours using an automated system (Accutrend GCT, Roche Diagnostics, Basel, Switzerland). Additional blood samples were collected to Vacuette K3EDTA tubes and Vacuette Z Serum clot activator tubes (Greiner Bio-One, Austria) for measurement of plasma insulin and serum adiponectin using the Rat Insulin ELISA Kit (Mercodia, Sweden) and the Rat Adiponectin Duoset (R&D Systems, USA). Insulin resistance was calculated using the homeostatic model assessment (HOMA) using the fasting insulin level (U/ml) and the fasting glucose level (mmol/l) [(If) × (Gf)/22.5].
The IPITT was performed after an overnight fast using insulin per bodyweight (250 mU/kg) and evaluation of glycemia before and at 15, 30, 45, 60, and 120 min using a glucose meter and test strips (Glucometer Elite, Bayer SA, Portugal). The area under the curve (AUC) was calculated.
Western Blotting
Western Blotting was carried out using 300 mg of ice-cold homogenized pEAT. Samples were separated in a polyacrylamide gel electrophoresis and transferred to PVDF membranes. After blocking (5% BSA), membranes were incubated overnight with the respective primary antibodies and during 2 h at room temperature with the secondary antibody. We used chemiluminescent detection (Clarity Western ECL Substrate on a VersaDoc® system with Quantity One analysis software, BioRad, Hercules, CA, USA) followed by image data processing employing ImageQuant 5.0 software (Amersham Biosciences, Sunnydale, CA, USA).
Analyzed parameters of adipose tissue metabolism and insulin sensitivity included insulin receptor (IRβ) and its phosphorylated form (IRβ-Tyr1161), glucose transporter type 4 (GLUT4), AMP-activated protein kinase (AMPK) and its phosphorylated form (AMPK-Thr172), peroxisome proliferator-activated receptor γ (PPAR-γ), and perilipin A, a protein involved in the regulation of lipid storage. Furthermore, we studied markers of angiogenesis like platelet endothelial cell adhesion molecule (CD31), fibroblast growth factor receptor (FGFR), plasminogen activator inhibitor-1 (PAI-1), angiotensin II receptor type 1 (AT-1), vascular endothelial growth factor (VEGF) and its receptor type 2 (VEGFR2), angiopoietin-2 (Ang-2), and its receptor tyrosine kinase type 2 (Tie2), as well as A disintegrin and metalloproteinases 9 (ADAM9), notch-receptor Delta-like ligand 4 (DLL4), endothelial nitric oxide synthase (eNOS), and phosphorylated form (eNOS-Ser1177).
Statistical Analysis
We used IBM SPSS® Statistics Base 24.0 software for data analysis. All data are presented as mean ± standard error of the mean. Given sample size and to reduce type I errors induced by repeated tests, we used the Kruskal–Wallis test to analyze differences between groups regarding the same variable or repeated measures of a variable in the same group. We considered differences statistically significant at a level of 95% (p < 0.05).
Results
Sleeve Gastrectomy Decreases Body and Adipose Tissue Weight and Improves Glycemic and Lipid Profiles
Type 2 diabetic GK rats showed an inferior body weight in comparison to age-matched Wistar rats, but a similar food and caloric intake (Table 1). GK rats feeding on a high-calorie diet presented with an increased body weight, due to significant weight gain between the age of 4 and 6 months, in consequence of a higher caloric intake during this period (Table 1). Rats submitted to sleeve gastrectomy (GKHFDSl) showed decreased caloric intake, modest weight gain after surgery, and a decrease of body and pEAT weight at the end of the study. Rats submitted to sham surgery and GKHFD rats presented with a similar phenotype (Table 1).
GK rats in the control group showed an increased fasting glycemia and area under the curve (AUC) during 2 h after the insulin tolerance test. The disturbance of glucose metabolism was aggravated in rats under enriched high-calorie diet which showed a further increased AUC during the insulin tolerance test, an increased glycemia 2 h after insulin administration, as well as an increased insulin resistance index (Fig. 1b–e). Sleeve gastrectomy significantly reduced fasting glycemia, AUC, glycemia after 2 h during the insulin tolerance test, and insulin resistance, with an improved glycemic profile (Fig. 1b–e). Furthermore, sleeve gastrectomy significantly increased the levels of the glucose transporter GLUT4 in the adipose tissue (Fig. 1f). No significant changes were observed for the adipose tissue levels of total and activated forms of the insulin receptor (Fig. 1, right panel) and no changes were observed in the sham group.
Lean GK rats did not show alterations of fasting triglycerides and total cholesterol levels, but serum adiponectin levels and adipose tissue levels of PPAR-γ and the lipid droplet protein perilipin A were significantly decreased in comparison to non-diabetic Wistar rats (Fig. 2a–d). GK rats feeding on a high-fat diet had increased circulating triglycerides and cholesterol levels, besides further decreased serum adiponectin levels and adipose tissue levels of PPAR-γ and the lipid oxidation enzyme AMPK (Fig. 2a–e). Sleeve gastrectomy significantly reduced triglycerides and cholesterol levels, which was consistent with increased serum adiponectin levels and adipose tissue levels of PPAR-γ, perilipin A, and total AMPK levels (Fig. 2), suggesting an improvement of fatty acid storage and oxidation after the surgery.
Lipid metabolism and adipose tissue function. Sleeve gastrectomy significantly decreased fasting serum triglycerides (a) and total cholesterol levels (b). The serum levels of adiponectin were significantly decreased in GKHFD rats, but this was partially prevented by sleeve gastrectomy (c). The adipose tissue levels of PPARgamma, perilipin A (d), and AMPK (e) were analyzed by Western Blot, showing a significant improvement in rats submitted to sleeve gastrectomy. Representative Western Blots are shown in the right panel; calnexin was used as loading control. No significant alterations were observed in activated (phosphrylation at Thr172) AMPK levels. Wistar—Wistar 6 months old fed a standard diet; GKSD—Goto-Kakizaki 6 months old fed a standard diet; GKHFD—Goto-Kakizaki 6 months old fed a high-fat high-sucrose diet for 5 months; GKHFDSl—GKHFD submitted to sleeve gastrectomy at 4 months old; GKHFDSh—GKHFD submitted to sham surgery at 4 months old. Bars represent means ± SEM, n = 8 (n = 6 for Western Blots). * vs Wistar; # vs GKSD; $ vs GKHFD; & vs GKHFDSh. One symbol p < 0.05; two symbols p < 0.01; three symbols p < 0.001
Sleeve Gastrectomy Improves Adipose Tissue Vascular Function Through Increased Sprouting Angiogenesis and Vasoactivity
The accumulation of fibrotic components in the pEAT was assessed through histological staining using Masson trichrome which was increased in GK rats fed on a high-calorie diet and reduced after sleeve gastrectomy (representative images are shown in Fig. 3a). Regarding the angiogenic markers of the adipose tissue, GK rats showed decreased levels of the endothelial cell marker CD31, as well as the key factors for the sprouting angiogenesis process VEGF and Ang-2, while no changes were observed in the expression of their receptors VEGFR2 and Tie-2 (Fig. 3b–d). GK rats showed also lower adipose tissue levels of ADAM9, one of the main enzymes involved in this system, as a trend to decreased DLL4 levels. Such phenotype was further enhanced in GK rats fed a high-calorie diet, which showed decreased DLL4 levels compared to control rats (Fig. 4).
Adipose tissue vascular function and angiogenesis. Masson trichrome staining (a) was applied to adipose tissue sections showing interstitial fibrosis in GK rats submitted to the high-caloric diet, which was reversed after sleeve gastrectomy. Increased expression of the endothelial cell marker CD31 (b) and the vascular growth factors VEGF (c) and Ang-2 (d) was also increased in rats submitted to sleeve gastrectomy, as well as ANGPTL4 (e). Representative Western Blots are shown in the right panel; calnexin was used as loading control. Wistar—Wistar 6 months old fed a standard diet; GKSD—Goto Kakizaki 6 months old fed a standard diet; GKHFD—Goto-Kakizaki 6 months old fed a high-fat high-sucrose diet for 5 months; GKHFDSl—GKHFD submitted to sleeve gastrectomy at 4 months old; GKHFDSh—GKHFD submitted to sham surgery at 4 months old. Bars represent means ± SEM, n = 8 (n = 6 for Western Blots). * vs Wistar; # vs GKSD; $ vs GKHFD; & vs GKHFDSh. One symbol p < 0.05; two symbols p < 0.01
Vascular differentiation markers. Sleeve gastrectomy restored the levels of the vascular differentiation factors DLL4 (a) and ADAM9 (b). The right panel shows representative Western Blots and no differences in other components of the Delta-Notch systems, calnexin was used as loading control. Wistar—Wistar 6 months old fed a standard diet; GKSD—Goto-Kakizaki 6 months old fed a standard diet; GKHFD—Goto-Kakizaki 6 months old fed a high-fat high-sucrose diet for 5 months; GKHFDSl—GKHFD submitted to sleeve gastrectomy at 4 months old; GKHFDSh—GKHFD submitted to sham surgery at 4 months old. Bars represent means ± SEM, n = 6. * vs Wistar; # vs GKSD; $ vs GKHFD; & vs GKHFDSh. One symbol p < 0.05; two symbols p < 0.01
Rats submitted to sleeve gastrectomy showed increased levels of the endothelial marker CD31, growth factors VEGF and Ang-2, differentiation markers DLL4 and ADAM9, as well as the hypoxia response factor Angptl4 (Figs. 3b–e and 4). Such results suggest that sleeve gastrectomy improves the number of endothelial cells in the tissue through increased sprouting angiogenesis, also modulating the differentiation and maturation of new blood vessel. Besides the number of blood vessels, the vascular function of the adipose tissue also depends on the regulation of vessel tonus, which is controlled by vasoactive factors like the NO for relaxation and PAI-1 or angiotensin II for contraction. GK rats under standard and under enriched high-calorie diet showed lower adipose tissue levels of eNOS, the main enzyme involved in NO production, and lower PAI-1 and AT1, the receptors of Ang-II responsible for vessel contraction (Fig. 5). Rats submitted to sleeve gastrectomy have shown increased levels of eNOS, PAI-1, and AT1, suggesting a better vascular function of adipose tissue vessels, with a better regulation between relaxation and contraction (Fig. 5).
Vasoactive factors. Increased expression of vasoactive factors in rats submitted to sleeve gastrectomy, namely the NO-producing enzyme eNOS (a) and PAI-1 and the Angiotensin II receptor AT-1 (b). Representative Western Blots are shown in the right panel; calnexin was used as loading control. Wistar—Wistar 6 months old fed a standard diet; GKSD—Goto-Kakizaki 6 months old fed a standard diet; GKHFD—Goto Kakizaki 6 months old fed a high-fat high-sucrose diet for 5 months; GKHFDSl—GKHFD submitted to sleeve gastrectomy at 4 months old; GKHFDSh—GKHFD submitted to sham surgery at 4 months old. Bars represent means ± SEM, n = 6. * vs Wistar; # vs GKSD; $ vs GKHFD; & vs GKHFDSh. One symbol p < 0.05; two symbols p < 0.01
Discussion
Sleeve gastrectomy improved glucose metabolism in obese diabetic GK rats feeding on a high-calorie diet in a similar fashion to that observed in non-obese diabetic GK rats on standard rat chow submitted to modification of the gastrointestinal tract [18]. Improvement of glucose metabolism was associated with a significant reduction in insulin resistance estimated by homeostasis model assessment (HOMA), a mathematical estimate based on glucose and insulin values that reflects results obtained by the euglycemic clamp technique [19, 20]. In parallel, a significantly increased expression of glucose transporter GLUT4 was observed in adipose tissue of GK rats submitted to sleeve gastrectomy. As GLUT4 is an important mediator for insulin-stimulated glucose uptake [21], this finding underscores the pertinence of improved insulin sensitivity after sleeve gastrectomy. Similar results regarding the increase of GLUT4 expression have been obtained after gastric bypass in the GK rats feeding on normal rat chow and in obese Zucker rats after ileal transposition [22, 23]. Possibly, GLUT4 also plays an important role in adipose tissue health and function by securing an adequate glucose uptake [24].
GK rats on a high-calorie diet showed increased triglyceride and cholesterol and decreased adiponectin serum levels as well as decreased adipose tissue levels of PPAR-γ, perilipin A, and the lipid oxidation enzyme AMPK, suggesting an impairment of lipid storage and oxidation in the adipose tissue. Lipid profile, serum adiponectin, and adipose tissue levels of PPAR-γ, perilipin A, and AMPK were improved after surgery suggesting an improvement of lipid storage and oxidation, which is in accordance with studies in humans that showed a metabolic shift based on PPAR-γ activation after gastric bypass and vertical sleeve gastrectomy [25]. Increased adipose tissue PPAR-γ expression following sleeve gastrectomy and, to a lesser extend gastric bypass, had also been observed in obese Zucker rats [26]. PPAR-γ, which is the main target of thiazolidinediones, is responsible for the regulation of adipogenesis [27] and for the downregulation of pro- inflammatory cytokines [28, 29]. Furthermore, PPAR-γ controls the expression and secretion of adiponectin in adipose tissue which in turn might be responsible for the systemic effects of PPAR-γ [30]. It had been shown in a mouse model of obese type 2 diabetes (db/db) that the favorable effects of PPAR-γ on the endothelium-dependent relaxation of the ex vivo aorta were suppressed by either the absence of adipose tissue or by the presence of adiponectin antibody [31].
Additionally, the same study was able to demonstrate that adiponectin increased the bioavailability of nitric oxide through AMPK signaling which is in accordance with our results regarding an increased AMPK expression after surgery. Exogeneous administration of adiponectin also improved adipose tissue dysfunction and PPAR-γ expression in a rodent model of diet-induced obesity which suggests a positive feedback loop between PPAR-γ expression and serum adiponectin levels [32]. Similarly to our results, ileal transposition also increased serum adiponectin levels in obese Zucker rats [23].
In humans, obesity and type 2 diabetes are associated with decreased adiponectin serum levels that revert after bariatric surgery, in particular bilio-pancreatic diversion, correlating favorably with the acute insulin response after an intravenous glucose load, 5 years after surgery [33]. However, no association between increased postoperative levels of adiponectin and the risk of cardiovascular morbidity and mortality could be found in a cohort from the Swedish Obese Subjects study [34], although the risk of cardiovascular events and myocardial infarction was reduced after surgery [35].
In the present study, sleeve gastrectomy increased the endothelial marker CD31, markers of sprouting angiogenesis like VEGF and Ang2 and the hypoxia response factor ANGPTL4 which has been shown to promote tissue repair and angiogenesis [36]. The balance between VEGF and Ang-2 is apparently crucial for the angiogenic process, and mice with adipose-specific deletion of VEGF develop metabolic dysfunction and insulin resistance under high-fat diet [37, 38], a finding that underscores the importance of restored angiogenesis after surgery. In humans, sleeve gastrectomy was shown to modify the expression of angiopoietin 1 and 2 as well as their receptor Tie-2 in subcutaneous and visceral adipose tissue. Changes in angiopoietin signaling correlated with a decrease in inflammatory activity in adipose tissue due to lower M1 macrophage infiltration [39], an observation that is corroborated by another study that showed decreased subcutaneous adipose tissue expression of pro-inflammatory factors after sleeve gastrectomy in obese non-diabetic patients, albeit without any reference to angiogenesis [40].
Consequently, our results and previous studies in humans indicate that surgery might promote improvement of adipose tissue inflammation and metabolic profile through mechanisms that include stimulation of angiogenesis. The formation of new fully functional blood vessels depends on cell proliferation regulated by endothelial growth factors, but also on the differentiation between the tip and the stalk cell from the newly formed vessel [41]. This process is mainly regulated by the activity of delta ligands and DLL4 in the case of endothelial cells, as well as a group of enzymes involved in DLL4 cleavage to trigger intracellular signaling which were also upregulated after surgery. Vascular function improved in operated animals as shown by increased eNOS which is associated with vasodilation, vasoprotection, and prevention of atherosclerosis [42]. While insulin-induced increase of PAI-1 levels is considered detrimental, endothelial dysfunction is possibly associated with an imbalance between production of nitric oxide through increased eNOS and the presence of atherothrombotic cytokines like PAI-1 [43] or AT-1 [21]. In human patients with morbid obesity a decrease in plasma PAI-1 levels was observed after gastric bypass, albeit not statistically significant [44], and after sleeve gastrectomy [45]. However, to our knowledge, no study assessed the postoperative evolution of increased PAI-1 expression in visceral adipose tissue of patients with morbid obesity [46].
In our obese animal model of type 2 diabetes, sleeve gastrectomy had a favorable overall impact on angiogenesis and adipose tissue health at a cellular level, possibly linked to improved microvasculature, a key feature of tissue dysfunction [47]. This innovative approach sheds a new light on the role of metabolic surgery in adipose tissue health. Conceivably, surgery might lead to a reduction in ectopic fat deposits and the deleterious effects on organ function. As animals submitted to sleeve gastrectomy decreased food intake after surgery, the contribution of a reduced caloric intake alone was not assessed in the present study as there was no pair-fed group. Yet, previous studies using pair-fed mice and rats under high-fat diet have already shown that the effect of sleeve gastrectomy on glucose tolerance, liver steatosis, adipose tissue or heart rate, and hypertension cannot be explained by reduced caloric intake alone [48, 49]. However, the link between the surgical transformation of the gastrointestinal tract and the observed modulation of angiogenesis and adipose tissue function remains to be clarified and deserves attention in further studies.
Conclusion
In the present study, sleeve gastrectomy led to a profound remodeling of adipose tissue and endothelial dysfunction in an animal model of obese type 2 diabetes. Markers of lipid storage and oxidation like perilipin A and PPAR-γ increased alongside serum adiponectin levels and markers of sprouting angiogenesis like VEGF and endothelial function like CD31 and eNOS. Insulin sensitivity was markedly improved in operated animals and associated with an increased expression of GLUT4 in periepididymal white adipose tissue. Further studies will have to explore the link between the surgical procedure itself and the observed improvement of adipose tissue health.
References
WHO. Obesity and overweight [Internet]. Factsheet no. 311. 2017; Available from: http://www.who.int/mediacentre/factsheets/fs311/en/
Rubino F, Nathan DM, Eckel RH, et al. Metabolic surgery in the treatment algorithm for type 2 diabetes: a joint statement by International Diabetes Organizations. Diabetes Care. 2016;39(6):861–77.
American Diabetes Association. Standards of medical care in diabetes—2017. Diabetes Care. 2017;40(Suppl 1):S1–135.
Adams TD, Davidson LE, Litwin SE, et al. Weight and metabolic outcomes 12 years after gastric bypass. N Engl J Med. 2017;377(12):1143–55.
Sjöström L. Review of the key results from the Swedish Obese Subjects (SOS) trial – a prospective controlled intervention study of bariatric surgery. J Intern Med. 2013;273(3):219–34.
Schauer P, Bhatt D, Kirwan J, et al. Bariatric surgery versus intensive medical therapy for diabetes - 5-year outcomes. N Engl J Med. 2017;376(7):641–51.
Osland E, Yunus RM, Khan S, et al. Diabetes improvement and resolution following laparoscopic vertical sleeve gastrectomy (LVSG) versus laparoscopic Roux-en-Y gastric bypass (LRYGB) procedures: a systematic review of randomized controlled trials. Surg Endosc Other Interv Tech Springer US. 2017;31(4):1952–63.
Eickhoff H. Central modulation of energy homeostasis and cognitive performance after bariatric surgery. Advances in Neurobiology, Obesity and Brain Function. 2017:213–36.
Eickhoff H, Louro TM, Matafome PN, et al. Amelioration of glycemic control by sleeve gastrectomy and gastric bypass in a lean animal model of type 2 diabetes: restoration of gut hormone profile. Obes Surg. 2015;25(1):7–18.
Blanco J, Jiménez A, Casamitjana R, et al. Relevance of beta-cell function for improved glycemic control after gastric bypass surgery. Surg Obes Relat Dis. 2014;10(1):9–13. quiz 189-90
Manning S, Batterham RL. The role of gut hormone peptide YY in energy and glucose homeostasis: twelve years on. Annu Rev Physiol. 2014;76(1):585–608.
Crewe C, An YA, Scherer PE. The ominous triad of adipose tissue dysfunction: inflammation, fibrosis, and impaired angiogenesis. J Clin Invest. 2017;127:74–82.
Hardy OT, Czech MP, Corvera S. What causes the insulin resistance underlying obesity? Curr Opin Endocrinol Diabetes Obes. 2012;19(2):81–7.
Corvera S, Gealekman O. Adipose tissue angiogenesis: impact on obesity and type-2 diabetes. Biochim Biophys Acta - Mol Basis Dis Elsevier BV. 2014;1842(3):463–72.
Smith U. Abdominal obesity: a marker of ectopic fat accumulation. J Clin Investig PMC. 2015;125(5):1790–2.
Cao Y. Angiogenesis and vascular functions in modulation of obesity, adipose metabolism, and insulin sensitivity. Cell Metab. 2013;18:478–89.
de Bona Castelan J, Bettiol J, d’Acampora AJ, et al. Sleeve gastrectomy model in Wistar rats. Obes Surg. 2007;17(7):957–61.
Eickhoff H, Louro T, Matafome P, et al. Glucagon secretion after metabolic surgery in diabetic rodents. J Endocrinol. 2014;223(3):255–65.
Matthews DR, Hosker JR, Rudenski AS, et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia Springer. 1985;28(7):412–9.
Levy JC, Matthews DR, Hermans MP. Correct homeostasis model assessment (HOMA) evaluation uses the computer program. Diabetes Care. 1998;21(12):2191–2.
Kim J, Montagnani M, Koh KK, et al. Reciprocal relationships between insulin resistance and endothelial dysfunction. Circulation. 2006;113(15):1888–904.
Li J, Wang Y, Zhou Y, et al. Gastric bypass surgery alters the mechanisms of insulin resistance in the adipose tissue of GK rats. Mol Med Rep. 2012 Nov;6(5):1111–6.
Tomasz S, Dominika S, Iwona K-S, et al. Long-term effect of ileal transposition on adipokine serum level in Zucker (Orl)-Lepr(fa) fatty rats. Obes Surg. 2015;25(10):1848–57.
Gustafson B, Hedjazifar S, Gogg S, et al. Insulin resistance and impaired adipogenesis. Trends Endocrinol Metab. 2015;26(4):193–200.
Jahansouz C, Xu H, Hertzel AV, et al. Partitioning of adipose lipid metabolism by altered expression and function of PPAR isoforms after bariatric surgery. Int J Obes. 2018;42(2):139–46.
Kawano Y, Ohta M, Hirashita T, et al. Effects of sleeve gastrectomy on lipid metabolism in an obese diabetic rat model. Obes Surg. 2013;23(12):1947–56.
Guilherme A, Virbasius JV, Puri V, et al. Adipocyte dysfunctions linking obesity to insulin resistance and type 2 diabetes. Nat Rev Mol Cell Biol. 2008;9(5):367–77.
La Paglia L, Listì A, Caruso S, et al. Potential role of ANGPTL4 in the cross talk between metabolism and cancer through PPAR signaling pathway. PPAR Res. 2017;2017
Gealekman O, Burkart A, Chouinard M, et al. Enhanced angiogenesis in obesity and in response to PPARgamma activators through adipocyte VEGF and ANGPTL4 production. Am J Physiol Endocrinol Metab. 2008;295:E1056–64.
Ahmadian M, Suh JM, Hah N, et al. PPARgamma signaling and metabolism: the good, the bad and the future. Nat Med. 2013;19(5):557–66.
Wong WT, Tian XY, Xu A, et al. Adiponectin is required for PPARγ-mediated improvement of endothelial function in diabetic mice. Cell Metab Elsevier Inc. 2011;14(1):104–15.
Matafome P, Rodrigues T, Pereira A, et al. Long-term globular adiponectin administration improves adipose tissue dysmetabolism in high-fat diet-fed Wistar rats. Arch Physiol Biochem. 2014:1–11.
Adami GF, Gradaschi R, Andraghetti G, et al. Serum leptin and adiponectin concentration in type 2 diabetes patients in the short and long term following biliopancreatic diversion. Obes Surg Obesity Surgery. 2016;26:2442–8.
Herder C, Peltonen M, Svensson P-AA, et al. Adiponectin and bariatric surgery: associations with diabetes and cardiovascular disease in the Swedish obese subjects study. Diabetes Care. 2014;37(5):1401–9.
Romeo S, Maglio C, Burza MA, et al. Cardiovascular events after bariatric surgery in obese subjects with type 2 diabetes. Diabetes Care. 2012;35(12):2613–7.
Chong HC, Chan JSK, Goh CQ, et al. Angiopoietin-like 4 stimulates STAT3-mediated iNOS expression and enhances angiogenesis to accelerate wound healing in diabetic mice. Mol Ther. 2014 Sep;22(9):1593–604.
Sung HK, Doh KO, Son JE, et al. Adipose vascular endothelial growth factor regulates metabolic homeostasis through angiogenesis. Cell Metab. Elsevier. 2013;17(1):61–72.
Bento CF, Fernandes R, Matafome P, et al. Methylglyoxal-induced imbalance in the ratio of vascular endothelial growth factor to angiopoietin 2 secreted by retinal pigment epithelial cells leads to endothelial dysfunction. Exp Physiol. 2010 Sep 1;95(9):955–70.
Figueroa-Vega N, Jordán B, Pérez-Luque EL, et al. Effects of sleeve gastrectomy and rs9930506 FTO variants on angiopoietin/Tie-2 system in fat expansion and M1 macrophages recruitment in morbidly obese subjects. Endocrine. Springer US. 2016;54(3):700–13.
Trachta P, Dostálová I, Haluzíková D, et al. Laparoscopic sleeve gastrectomy ameliorates mRNA expression of inflammation-related genes in subcutaneous adipose tissue but not in peripheral monocytes of obese patients. Mol Cell Endocrinol. 2014;383(1–2):96–102.
Stapor P, Wang X, Goveia J, et al. Angiogenesis revisited - role and therapeutic potential of targeting endothelial metabolism. J Cell Sci. 2014;127:4331–41.
Förstermann U, Sessa WC. Nitric oxide synthases: regulation and function. Eur Heart J. 2012;33(7):829–37.
Muniyappa R, Sowers JR. Role of insulin resistance in endothelial dysfunction. Rev Endocr Metab Disord. 2013;14(1):5–12.
Domienik-Karłowicz J, Rymarczyk Z, Dzikowska-Diduch O, et al. Emerging markers of atherosclerosis before and after bariatric surgery. Obes Surg. 2015;25(3):486–93.
Gumbau V, Bruna M, Canelles E, et al. A prospective study on inflammatory parameters in obese patients after sleeve gastrectomy. Obes Surg. 2014;24(6):903–8.
Umemura A, Sasaki A, Nitta H, et al. Effects of changes in adipocyte hormones and visceral adipose tissue and the reduction of obesity-related comorbidities after laparoscopic sleeve gastrectomy in Japanese patients with severe obesity. Endocr J. 2014;61(4):381–91.
Rodrigues T, Matafome P, Seiça R. A vascular piece in the puzzle of adipose tissue dysfunction: mechanisms and consequences. Arch Physiol Biochem. 2014;120(1):1–11.
Schneck AS, Iannelli A, Patouraux S, et al. Effects of sleeve gastrectomy in high fat diet-induced obese mice: respective role of reduced caloric intake, white adipose tissue inflammation and changes in adipose tissue and ectopic fat depots. Surg Endosc Other Interv Tech. 2014;28(2):592–602.
Rodríguez A, Becerril S, Valentí V, et al. Short-term effects of sleeve gastrectomy and caloric restriction on blood pressure in diet-induced obese rats. Obes Surg. 2012;22(9):1481–90.
Funding
This study was supported by the Portuguese Foundation for Science and Technology (Consortium CNC.IBILI UID/NEU/04539/2013; SFRH/BD/101172/2014 and SFRH/BPD/104881/2014) and by the Faculty of Medicine, University of Coimbra.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Statement of Animal Rights
The study protocol regarding the use of laboratory animals was approved by the Institutional Ethics Committee. After completing the study, all animals were sacrificed by cervical displacement, according to the procedures approved by the Institutional Animal Care and Use Committee.
Informed Consent
Does not apply.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Eickhoff, H., Rodrigues, T., Neves, I. et al. Effect of Sleeve Gastrectomy on Angiogenesis and Adipose Tissue Health in an Obese Animal Model of Type 2 Diabetes. OBES SURG 29, 2942–2951 (2019). https://doi.org/10.1007/s11695-019-03935-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-03935-z