Abstract
Background
The best alimentary and biliopancreatic limb (BPL) lengths in the Roux-en-Y gastric bypass (RYGB) still remain unclear. The aim of this study was to compare the effect of a BPL of 70 vs 120 cm, with a constant AL of 150 cm on long-term weight loss, remission of comorbidities, and supplementation needs after RYGB.
Patients and Methods
A prospective randomized study of morbidly obese patients undergoing RYGB was performed. Patients were randomized into two groups: those patients undergoing RYGB with a BPL of 70 cm (BPL 70 cm) and those ones undergoing RYGB with a BPL of 120 cm (BPL 120 cm). BMI, excess BMI loss (EBMIL), remission of comorbidities and specific vitamin and mineral supplementation needs at 1, 2, and 5 years were analyzed.
Results
Two hundred fifty-three patients were included in each group. There were no significant differences in BMI, EBMIL and the remission of diabetes mellitus, hypertension, and dyslipidemia between groups at 1, 2, and 5 years after surgery. Patients from group BPL 120 cm required greater specific supplementation of vitamin B12, folic acid, and vitamin A during all the follow-up.
Conclusion
A RYGB with 120 cm BPL does not achieve greater weight loss or remission of comorbidities than a RYGB with 70 cm BPL but is associated with greater deficiencies of vitamin B12, vitamin A, and folic acid.
Trial Registration
ClinicalTrials.gov Identifier NCT03607305. https://clinicaltrials.gov/.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Roux-en-Y gastric bypass (RYGB) is actually the second most frequently performed bariatric procedure worldwide, after sleeve gastrectomy [1]. Since its introduction 50 years ago, there have been many variations to RYGB in the purpose to achieve greater weight loss with a minimum of nutritional complications [2]. Most studies have reported alimentary limbs (AL) length of 100 to 150 cm and biliopancreatic limb (BPL) length of 50 to 120 cm, often with an unmeasured common limb length [3, 4]. Usually, a mean excess weight loss (EWL) of 70 to 80% can be expected, but recent studies have demonstrated that long-term weight regain is more frequent than expected [5].
In bariatric malabsorptive or mixed procedures, such as RYGB, bowel length determines the bowel’s caloric absorptive capacity and its ability to absorb micronutrients and, theoretically, the weight loss achieved, the improvement in obesity-related comorbidities, and the postoperative micronutrient deficiencies should be correlated with the length of the bypassed bowel. Actually, the best jejunal and ileal lengths to be left in alimentary continuity still remain unclear [6, 7]. The lack of standardization in performing RYGB poses further problems with interpretation and comparison of scientific literature [8].
Though both bypassed bowel segments limit the absorption of nutrients, BPL provides complete loss of absorptive capacity, as there is no transit of nutrients through this bowel segment, whereas AL may still absorb some nutrients that do not require further digestion by biliopancreatic secretion [7].
The aim of this study was to compare the effect of a BPL of 70 vs 120 cm, which are two common measures of BPL at our medium, with a constant AL of 150 cm on long-term weight loss, remission of comorbidities, and supplementation needs after RYGB.
Patients and Methods
A prospective randomized clinical study was performed, including morbidly obese patients, undergoing RYGB as primary bariatric procedure, between June 2009 and June 2013.
Inclusion criteria were body mass index (BMI) > 40 kg/m2 or BMI > 35 kg/m2 with the presence of comorbidities associated to obesity and age older than 18 years. Exclusion criteria were patients undergoing other bariatric techniques than RYGB, patients undergoing RYGB with different BPL or AL lengths than that reported for this study, any other surgical procedure added to the bariatric surgery, and impossibility to comply with pre-established clinical follow-up.
Given that we have no previous data of our institutions with 5 years follow-up, the sample size calculation was based on historic data of our centers of excess BMI loss (EBMIL) 2 years after RYGB of 68.2% with a BPL of 70 cm (control group) and an expected increase up to 80% EBMIL 2 years after RYGB with a BPL of 120 cm (experimental group). At 80% power and a significance level of p = 0.05, it was calculated that 215 patients were required in each arm of the study. Anticipating a 15% of loss of patients at follow-up, finally, 253 patients were included in each group.
Patients were randomly assigned using a random-number table into two groups: those patients undergoing RYGB with a BPL of 70 cm and those ones undergoing RYGB with a BPL of 120 cm. AL was constant in both groups (150 cm).
Preoperative Evaluation
A multidisciplinary team, including surgeons, endocrinologists, dieticians, endoscopists, radiologists, anesthesiologists, psychologists, and specialized nurse staff, performed a combined medical, nutritional, and endocrinological work-up to evaluate potential surgical candidates. Preoperative assessment included abdominal ultrasound, upper gastrointestinal endoscopy, polysomnography, and analytical evaluation of the nutritional status. Psychologists assessed additional interviews to evaluate the implication of the patient in following a strict diet in the postoperative course. A dietician established a diet consisting in a total daily energy intake of 1200 Kcal. A weight loss of at least 10% of the patient’s weight was considered an indispensable condition to undergo the surgery.
Patients received information about possible perioperative complications and necessary postoperative nutritional supplementation.
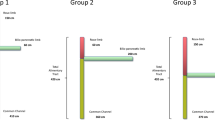
Surgical Technique
The operations were performed by four surgeons, following the same surgical technique. All procedures were performed laparoscopically. Five ports were placed in right hypochondrium (12 mm), left hypochondrium (12 mm), epigastrium (11 mm), subxyphoideal (11 mm), and left flank (5 mm). A 6-cm-long gastric pouch was performed, calibrating it with a 36-Fr bougie, with a linear stapler (I-Drive with Tri-staple cartridges, Medtronic, USA). A 70-cm BPL in one group and a 120-cm BPL in the other group were performed. A 150-cm alimentary limb was performed uniformly. A mark was performed in the graspers used for the bowel measurement, indicating 10 cm, assuring the homogeneity in all the patients. Gastro-enteral anastomosis was performed with circular stapler using the Orvil-probe and EEA 25 mm. Entero-enteral anastomoses were performed with linear stapler (I-Drive with Tri-staple cartridges, Medtronic, USA), and the enterotomy was sutured with continuous barbed suture V-Loc 2/0 (Medtronic, USA). Mesenteric defects were not closed in any of the cases. Anastomosis integrity was verified with methylen blue dye test. Common limb was not measured in any of the cases.
Before hospital discharge, the two groups of patients received identical postoperative counseling, support, diet, and exercise instructions. Multivitamin and mineral supplements were uniformly prescribed in the two groups (two tablets/day).
Follow-Up
All the patients were followed up by the surgeon and endocrinologist 1, 2, and 5 years after surgery. Primary outcomes were number of BMI units lost and excess BMI loss (EBMIL), whereas secondary outcomes were the remission of comorbidities and needs for specific supplementations, according to the deficiencies observed at analytical blood tests.
Medical treatment, such as antidiabetic, antihypertensive, and hypolipemiant drugs, was adjusted according to the current needs of the patient. Multivitamin and minerals were uniformly prescribed (Multicentrum, Pfizer, USA), two tablets per day.
Remission of Comorbidities
Complete remission of type 2 diabetes mellitus (T2DM) was defined as plasma glucose below 100 mg/dL and glycated hemoglobin (HbA1c) below 6% in the absence of hypoglycemic treatment. Remission of hypertension (HT) was defined as blood pressure below 135/85 mmHg in the absence of anti-hypertensive treatment; remission of dyslipidemia (DL) was defined as fasting plasma triglycerides below 200 mg/dL, total cholesterol below 200 mg/dL, and high-density lipoprotein cholesterol over 40 mg/dL in the absence of pharmacological therapy.
Variables
All the variables were analyzed at baseline (preoperative values) and 1, 2, and 5 years after surgery. Anthropometric variables included BMI, number of BMI units lost, and EBMIL. Complete remission of comorbidities (T2DM, HT, and DL) was monitored. Specific vitamin and mineral supplementation needs were recorded, according to the deficiencies observed in the laboratory data.
Statistical Analysis
Statistical analysis was performed with SPSS 22.0 for Windows. Quantitative variables that followed a normal distribution were summarized by means and standard deviations. For non-Gaussian variables, median and range were used. Qualitative variables were summarized by number and percentage of cases. Comparison of qualitative variables was performed with the chi-square test; in cases with fewer than 5 observations in the cell, the Fisher exact probability method was used. Means were compared with the Student t test (Mann-Whitney test if the quantitative variable did not follow a Gaussian distribution). Values of p < 0.05 were considered significant.
Results
A total of 506 patients were included in the study, 253 in each group. There were no significant differences in age, gender, preoperative weight and BMI, and distribution of comorbidities between groups (Table 1).
Postoperative complications included 1 hemoperitoneum and 1 gastrojejunal anastomotic leak in RYGB 70, and 1 gastrojejunal anastomotic leak and 2 jejuno-jejunal anastomotic leaks in RYGB 120, all of them requiring reintervention (Non significant: NS).
Follow-up rate was 100% (506 patients) after 1 year, 96.8% (490 patients) after 2 years, and 93.1% (471 patients) after 5 years, without differences between groups.
Postoperative Anthropometric Measurements
One year after surgery, BMI after RYGB with 70 cm BPL (RYGB 70) was 31.9 + 6.1 kg/m2 and after RYGB with 120 cm BPL (RYGB 120) 30.7 + 5.2 kg/m2,with EBMIL of 68.6 + 13 and 70.2 + 9.9%, respectively (NS). Mean BMI units lost were 12.3 + 2 kg/m2 after RYGB 70 and 13.4 + 1.9 kg/m2 after RYGB 120 (NS).
Two years after surgery, BMI after RYGB with 70 cm BPL (RYGB 70) was 31.4 + 5.1 kg/m2 and after RYGB with 120 cm BPL (RYGB 120) 30.1 + 5.2 kg/m2, with EBMIL of 69.5 + 13 and 70.5 + 11%, respectively (NS). Mean BMI units lost were 12.8 + 2.1 kg/m2 after RYGB 70 and 14 + 2 kg/m2 after RYGB 120 (NS).
Five years after surgery, BMI after RYGB with 70 cm BPL (RYGB 70) was 34.8 + 6.8 kg/m2 and after RYGB with 120 cm BPL (RYGB 120) 34.2 + 5.9 kg/m2, with EBMIL of 51.8 + 14.1 and 52.9 + 12.3%, respectively (NS). Mean BMI units lost were 9.4 + 1.6 kg/m2 after RYGB 70 and 9.9 + 1.5 kg/m2 after RYGB 120 (NS).
There were no significant differences in the remission of T2DM, HT, and DL between groups at 1, 2, and 5 years after surgery (Table 2). The greatest complete remission rate for T2DM and DL was observed the first year after surgery, whereas the maximal remission rate of HT was obtained the second year. Recurrences of T2DM were initially treated with Metformin, whereas 25.4% of the patients required the addition of insulin (without differences between groups). Eighty percent of the patients in RYGB 70 group, who were preoperatively under treatment with insulin, showed a relapse, while 73.7% of the patients in RYGB 120.
Recurrences of HT were managed with angiotensin-converting enzyme inhibitors and recurrences of DL with statins.
Specific Vitamins and Minerals Supplementation Needs (Table 3)
One year after surgery, there were no significant differences in the specific supplementation needs between groups, excepting for vitamin B12, folic acid, and vitamin A, which were greater in the RYGB with BPL 120 cm. Similarly, 2 years postoperatively, vitamin B12, folic acid, and vitamin A supplementation needs were greater in the RYGB 120. Five years after surgery, supplementation needs of vitamin B12 and vitamin A were greater in RYGB 120, but significant differences could not be observed for folic acid.
Discussion
Lengths of BPL, AL, and common limb (CL) that will produce maximum effect on hunger and satiety and provide an optimum threshold for absorptive capacity, effective for most patients, remain to be determined, and the hormonal pathways that can help us to quantify and measure these changes have only just begun to be explored [9].
The normal percentage of short-term EBMIL is around 70 to 80% after RYGB, but there are also patients with insufficient weight loss or weight regain after initial loss. According to Reinhold’s criteria, inadequate long-term weight loss (BMI over 35 kg/m2 and excess weight loss below 50%) after standard RYGB can be observed in up to 40% of the cases [10, 11]. Several theories have tried to explain the insufficient weight loss after RYGB, including the hypertrophy of the mucosal surface area, the adaption of the AL, and an increase of the diameter of the AL and common limb, which can increase the absorption of nutrients [12].
In an evidence-based review, Stefanidis et al. came to the conclusion that AL length does not play a significant role in weight loss after RYGB, but these authors have failed to take in consideration the common limb length, which could be a determinant factor for malabsorption and therefore weight loss [13]. Tacchino has defended that in malabsorptive procedures, it is wise to measure the length of the bowel that remains distal to the excluded segment, rather than to infer its length after measuring the excluded portion. The measurement of the CL has demonstrated to be more associated with the final weight loss rather than the determination of the BP limb [6]. In contrast, in the study of Navez et al. [14], with standardized AL length of 150 cm and BPL length of 75 cm, no correlation could be demonstrated between the anatomical variation of the common limb length and weight loss, suggesting a limited impact of malabsorption on weight loss after RYGB. The fact that gastric bypass could be more a restrictive rather than a malabsorptive procedure has also been supported by other authors [15]. However, the shorter the common channel, the more malabsorption and metabolic problems can be expected.
There is little doubt that BPL and AL in RYGB behave differently when it comes to the loss of absorptive capacity. BPL provides complete loss of absorptive capacity, whereas AL may still absorb some nutrients. Nergaard et al. [16] carried out a prospective randomized study, comparing a RYGB with 200 cm-BPL and 60 cm-AL, with a RYGB with 60 cm-BPL and 150 cm-AL. They observed that weight loss was significantly greater in the patients with longer BPL, with less long-term weight regain, but mineral and vitamin supplementation needs were also greater among these patients. Significant differences in the remission of comorbidities between groups could not be observed. We agree with these authors in the fact that longer bypassed limbs, especially longer BPL, do not correlate with the remission of comorbidities. It has been demonstrated that their resolution is often independent of the weight loss achieved and hormonal theories have been postulated. The modification of the gastrointestinal tract exposes the distal gut to increase the delivery of non-digested nutrients. Over-stimulated enteroendocrine L cells respond by secreting glucagon-like peptide-1 (GLP-1) and peptide tyrosine-tyrosine (PYY). These two hormones play a major role independently of restrictive and malabsorptive effects. GLP-1 slows gastric emptying, promotes insulin release, inhibits glucagon secretion, inhibits gastric acid secretion, and acts on the central nervous system to induce satiety and decrease food intake. Similar to GLP-1, PYY delays gastric emptying and inhibits gastric acid secretion as well. Other endocrine modifications have been described as foregut exclusion theory and ghrelin secretion by the X/A-cells of the stomach [17,18,19].
Mahawar et al. [20] performed a recent systematic review, evaluating the effect of the different limb lengths of RYGB on weight loss. In contrast to what would be expected, that bypassing longer small bowel length would be associated with more malabsorption and superior weight loss, the findings of their review confirmed that malabsorption does not make an important contribution to weight loss, as most of the weight loss is successfully achieved with small bowel bypass length of as short as 100–200 cm, and bypassing more than 200 cm does not significantly improve weight loss outcomes for most patients. They hypothesized that it is the bypass of most of jejunum which is more important for weight loss purposes. This could further explain why bypassing more than 200 cm does not significantly improve weight loss as that will usually take us past jejunum in most patients. Tacchino has previously observed that the length of jejunum is directly correlated with preoperative weight, and an adequate bypass of jejunum in a RYGB is associated with optimal weight loss. He determined in his study that mean jejunum length was 170.4 cm (minimum109.5 cm and maximum 266.7 cm) [6]. According to these data, in both groups of our study, more than 200 cm of small bowel have been bypassed and probably jejunum was completely bypassed in most patients of the BPL70 group. Further malabsorption is not associated with greater weight loss.
Notwithstanding, in our BPL 120 group, we have observed significantly greater supplementation needs for vitamin B12, folic acid, and vitamin A. Nergaard et al. observed in their patients with longer BPL more iron and calcium deficiencies, but these elements are known to be primarily absorbed from the proximal part of the intestines, and most patients undergoing an RYGB, independently of the limb lengths, need frequent adjustments of their supplementation long-life [16]. Folic acid deficiency might appear in up to 40% of the patients undergoing an RYGB. Folic acid is mostly absorbed in jejunum. The longer the bypassed bowel segment, the lower is the segment of the remaining jejunum, or even absent, and consequently, lower absorption of folic acid would be achieved. Deficiencies in vitamin B12 after RYGB have been described in up to 80% of the cases. The reduction of the stomach decreases the production of intrinsic factor, which is the main vehicle for vitamin B12 absorption in the terminal ileum. Thus, vitamin B12 must be absorbed along the whole small bowel, and the shorter the bowel that remains distal to the excluded segment, the lower will be the absorption of vitamin B12. Finally, vitamin A, similarly to vitamin D, is a fatty soluble vitamin and RYGB is a selective procedure for fat malabsorption. Differences in vitamin D are not observed as more than 90% of the patients required supplementation in both groups. Vitamin A deficiencies are less frequent than vitamin D ones, but they are strongly associated with the length of bypassed segment and finally the degree of malabsorption [21].
It is widely known that better results are obtained, in terms of weight loss and remission of comorbidities, after pure malabsorptive procedures, such as biliopancreatic diversion-duodenal switch (BPD-DS), one anastomosis gastric bypass (OAGB), or single anastomosis duodenoileal bypass (SADIS), but on the other hand, these approaches are associated with greater nutritional deficiencies [1]. It is true that in most of these procedures, BPL is much longer than 120 cm and in OAGB and SADIS, the BPL is the only bypassed bowel segment. As previously mentioned, the AL in RYGB has a certain absorption ability and probably this is increased with the pass of the time related with an adaptation process, so that the only real bypassed segment would be the BPL and 70 cm or even 120 cm are not a length enough for obtaining results comparable to that after pure malabsorptive procedures. However, we have to assume as limitations of this study that a difference of 50 cm of BPL (70 vs 120) cannot be enough to obtain significant differences in weight loss and remission of comorbidities, despite that significant differences were observed in several micronutrient deficiencies. Moreover, the number of diabetic patients included in both groups is probably not high enough to capture significant differences and this small sample size prevents us for achieving significant results in the stratification analysis, regarding evolution time of T2DM or preoperative insulin resistance. Further studies must be conducted in order to evaluate these issues and confirm our results.
Conclusion
We failed to demonstrate significant differences in weight loss and remission of comorbidities between RYGB with 120 cm BPL and RYGB with 70 cm BPL, with constant 150 cm AL. However, RYGB with 120 cm BPL is associated with greater deficiencies of vitamin B12, vitamin A, and folic acid.
References
Schauer PR, Kashyap SR, Wolski K, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med. 2012;366:1567–76.
Mason EE, Ito C. Gastric bypass. Ann Surg. 1969;170:329–39.
Madan AK, Harper JL, Tichansky DS. Techniques of laparoscopic gastric bypass: on-line survey of American Society for Bariatric Surgery practicing surgeons. Surg Obes Relat Dis. 2008;4:166–72.
Elder KA, Wolfe BM. Bariatric surgery: a review of procedures and outcomes. Gastroenterology. 2007;132:2253–71.
Higa K, Ho T, Tercero F, et al. Laparoscopic Roux-en-Y gastric bypass: 10-year follow-up. Surg Obes Relat Dis. 2011;7:516–25.
Tacchino RM. Bowel length: measurement, predictors and impact on bariatric and metabolic surgery. Surg Obes Relat Dis. 2015;11:328–34.
Stefanidis D, Kuwada TS, Gersin KS. The importance of the length of the limbs for gastric bypass patients–an evidence-based review. Obes Surg. 2011;21:119–24.
Mahawar KK, Kumar P, Parmar C, et al. Small bowel limb lenghts and Roux-en-Y gastric bypass: a systematic review. Obes Surg. 2016;26:660–71.
Rubino F, Gagner M, Gentileschi P, et al. The early effect of the roux-en-Y gastric bypass on hormones involved in body weight regulation and glucose metabolism. Ann Surg. 2004;240:236–42.
Christou NV, Look D, Maclean LD. Weight gain after short- and long-limb gastric bypass in patients followed for longer than 10 years. Ann Surg. 2006;244:734–40.
Suter M, Calmes JM, Paroz A, et al. Results of Roux-en-Y gastric bypass in morbidly obese vs superobese patients: similar body weight loss, correction of comorbidities, and improvement of quality of life. Arch Surg. 2009;144:312–8.
Mumphrey MB, Patterson LM, Zheng H, et al. Roux-en-Y gastric bypass surgery increases number but not density of CCK-, GLP-1-, 5-HT-, and neurotensin-expressing enteroendocrine cells in rats. Neurogastroenterol Motil. 2013;25:e70–9.
Stefanidis D, Kuwada TS, Gersin KS. The importance of the length of the limbs for gastric bypass patients—an evidence-based review. Obes Surg. 2011;21:119–24.
Navez B, Thomopoulos T, Stefanescu I, et al. Common limb length does not influence weight loss after standard laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2016;26:1705–9.
Papadia F. Effect of standard versus extended Roux limb length on weight loss outcomes after laparoscopic Roux-en-Y gastric bypass. Surg Endosc. 2004;18:1683.
Nergaard BJ, Leifsson BG, Hedenbro J, et al. Gastric bypass with long alimentary limb or long pancreato-biliary limb—long-term results on weight loss, resolution of co-morbidities and metabolic parameters. Obes Surg. 2014;24:1592–602.
Karra E, Yousseif A, Batterham RL. Mechanisms facilitating weight loss and resolution of type 2 diabetes following bariatric surgery. Trends Endocrinol Metab. 2010;21:337–44.
Beckman LM, Beckman TR, Earthman CP. Changes in gastrointestinal hormones and leptin after roux-en-Y gastric bypass procedure: a review. J Am Diet Assoc. 2010;110:571–84.
Konturek PC, Konturek JW, Cześnikiewicz-Guzik M, et al. Neuro-hormonal control of food intake: basic mechanisms and clinical implications. J Physiol Pharmacol. 2005;56:5–25.
Mahawar KK, Kumar P, Parmar C, et al. Small bowel limb lengths and Roux-en-Y gastric bypass: a systematic review. Obes Surg. 2016;26:660–71.
Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient—2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery. Surg Obes Relat Dis. 2013;9:159–91.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study.
Statement of Human Rights
All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ruiz-Tovar, J., Vorwald, P., Gonzalez-Ramirez, G. et al. Impact of Biliopancreatic Limb Length (70 cm vs 120 cm), with Constant 150 cm Alimentary Limb, on Long-Term Weight Loss, Remission of Comorbidities and Supplementation Needs After Roux-En-Y Gastric Bypass: a Prospective Randomized Clinical Trial. OBES SURG 29, 2367–2372 (2019). https://doi.org/10.1007/s11695-019-03717-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-03717-7