Abstract
Aims
To compare the perioperative parameters and excess weight loss between patients operated by laporoscopic Roux-en-Y gastric bypass (LRYGB), as a primary operation or a revisional, for insufficient weight loss after vertical banded gastroplasty (VBG) or adjustable gastric banding (AGB).
Methods
A retrospective analysis of all patients who underwent a LRYGB was performed for the period 2004–2011. Demographics, preoperative body mass index (BMI), co-morbidities, operation time, conversion rate, perioperative complications, hospitalization period, and % of excess BMI loss (%EBMIL) were investigated and compared between groups.
Results
Three hundred forty-two laparoscopic gastric bypass operations were performed, 245 were primary, and 97 revisional. Median follow-up was 30 months (range 0–108 months). Mean BMI (kg/m2) before bypass was 45.2 for primary laparoscopic Roux-en-Y gastric bypass (pLRYGB) and 41.1 for revisional laparoscopic Roux-en-Y gastric bypass (rLRYGB). Median operative time and length of stay were longer for rLRYGB 157.5 versus 235 min (p < 0.001) and 6 versus 6.5 days (p = 0.05). Conversion to laparotomy was performed in eight patients, 0.4% of primary and 7.2% of revisional. Morbidity rate was 6.5% in pLRYGB versus 10% in rLRYGB (NS). There was one death in the primary group. Percentage of EBMIL was significantly lower in the revisional group at 12, 18, and 24 months of follow-up.
Conclusions
Revisional and primary gastric bypass have no statistical differences in terms of morbidity. The % of excess BMI loss is lower after revisional gastric bypass during the first 2 years of follow-up. The trend of weight loss or weight regain was similar in both groups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alongside the increasing prevalence of morbid obesity and bariatric surgical procedures, there are increasing numbers of insufficient weight loss after bariatric procedures, leading to revisional surgery [1,2,3]. Adjustable gastric banding (AGB) and vertical banded gastroplasty (VBG) were, till recently, the most widely performed restrictive procedures for treating obesity. Roux-en-Y gastric bypass is now considered the procedure of choice for treating obesity, as well as for revisional surgery of failed restrictive procedures or insufficient weight loss [4,5,6].
For these procedures, failure is defined as insufficient weight loss or weight regain. Reasons for failure include procedural complications such as band migration or band slippage and gastrogastric fistula and pouch dilatation.
Complications such as esophageal dilatation and Barrett esophagus, as well as septic complications are not unusual, while weight regain, cachexia, and excessive weight loss are also reported [7,8,9].
Recently, many surgical teams are trying to evaluate revisional bariatric surgery. A systematic review identified that most of the published series lack long-term follow-up and sufficiently homogenous samples [10].
In this study, our aim was to compare the postoperative results of a consecutive series of patients that had all undergone primary or revisional laparoscopic gastric bypass procedures during a defined period. To avoid bias, we selected only the insufficient weight loss after AGB and VBG procedures. All operations were performed by laparoscopy, by a single surgeon and a single technique. We compare the success rate of revisional gastric bypass, defined as final body mass index (BMI) and the percentage of excess BMI loss (%EBMIL), to our primary gastric bypass operations. We also examined changes in these parameters over long-term follow-up.
Patients and Methods
We retrospectively reviewed all the collected data of our patients treated by laporoscopic Roux-en-Y gastric bypass (LRYGB).
All patients with a prior AGB or VBG, who had undergone a revisional bariatric procedure, were identified.
Patients with multiple previous bariatric operations were excluded. Primary gastroplasties included in our series had previously been performed by either open or laparoscopic access.
Postoperative outcomes and detailed weight data (BMI changes, BMI before initial gastroplasty, BMI before and after LRYGB) were obtained via medical records, postal questionnaire, or direct telephone calls.
Revision surgery was indicated in cases of insufficient weight loss or weight regain with excess weight loss (EWL) < 50% or BMI > 35 despite diet adaptation [11]. Seven patients with initial BMI < 35 that were operated for reasons other than insufficient weight loss were excluded from analysis of weight loss (medical resistant gastroesophageal reflux, symptomatic hiatal hernia, excessive weight loss, and alimentary intolerance). Preoperatively, all patients underwent upper GI endoscopy with Helicobacter pylori testing and eradication if necessary. An upper GI contrast study was additionally performed in all revisional cases. A multidisciplinary team had evaluated and approved operations in all cases.
Patients were followed up clinically at our institution at 1 week and 1 month postoperatively, every 3 months during the first year, every 6 months for the second year, and yearly thereafter. Body weight and BMI were calculated, as well as the %EBMIL with reference to the patient’s initial weight before LRYGB. For revision surgery, the %EBMIL was also calculated with reference to initial BMI before the restrictive procedure [12].
Surgical Procedure
Primary LRYGB
Pneumoperitoneum was established with Veress needle. A 6-trocar technique was applied (two 5-mm and four 12-mm optical trocars). Identification of the Treitz ligament, section of the omentum with ultrasonic scissors, and measurement of a 75-cm long, biliopancreatic limb. The gastric pouch was dissected with ultrasonic scissors and divided by consecutive applications of cutting endostaplers (60 mm/3.5–4.2 mm) to create a 25- to 30-ml gastric pouch. End to side gastrojejunal anastomosis was performed by two continuous Maxon 2/0 running sutures, in one layer. An alimentary limb of 150 cm was accurately measured from that point. A jejuno-jejunal anastomosis was performed semi-mechanically with an endostapler (60/2.5 mm) and a continuous suture of Maxon 2/0. Mesenteric space was closed by non-absorbable suture, and the jejunum between the two anastomoses was finally transected. Petersen space was closed. Finally, methylene blue was injected to control gastrojejunal anastomosis and exclude leakage from the jejunal transection line. A paraanastomotic silastic drain was placed until postoperative day 2 and removed after a negative Gastrografin swallow.
Revisional LRYGB
In cases of previous gastroplasty, thorough dissection and adhesiolysis were performed. Once the stomach was well dissected and separated from surrounding tissues, a healthy gastric wall was selected to create the gastric pouch.
Revisional GB After Adjustable Gastric Banding
The gastric band was transected and removed from its capsule with a thorough attempt to eliminate fibrotic tissue. Gastric band was extracted, and previous gastric plication was released. Creation of the gastric pouch was performed by cutting endostaplers (60/4.2 mm).
Revisional GB After Vertical Banded Gastroplasty
The gastric pouch was created after thorough dissection of the previous gastroplasty. Either a simple resection of the band with the staple line, or a complete resection of the fundus with the band and the staple line was performed. The procedure was completed by the same anastomosis in a healthy, not-previously stapled gastric wall. The alimentary and biliopancreatic limb and anastomosis were of the same length. Patients were discharged when clinical and biochemical parameters were restored and when alimentation with liquid diet was tolerated. A daily subcutaneous low-molecular-weight heparin injection for a total of 20 days and a proton pump inhibitor for 3 months were prescribed. Vitamin, calcium, ferric, or other supplementations were administered depending on biology exams during follow-up.
Data Collection and Statistics
Continuous variables are presented with mean and standard deviation (SD) or with median and interquartile range (IQR). Quantitative variables are presented with absolute and relative frequencies. For the comparison of proportions, chi-square and Fisher’s exact tests were used. For the comparison of study variables between the primary and the revisional bypass, the non-parametric Mann-Whitney test was computed for non-normal variables and the Student’s t test for normal variables.
%EBMIL was calculated as following by the type: (initial BMI – follow-up BMI)/(initial BMI - ideal BMI), while ideal BMI is considered the 25 kg r/m2 [13,14,15,16]. Two different ways were used for the revisional operations, considering as initial BMI the one before initial gastroplasty (pre-gastroplasty BMI) or the BMI before revisional surgery (pre-gastric bypass BMI). To longitudinally assess changes in BMI and EWL, mixed linear regression models spline with time (knot was selected at 1.5 years) were fitted that accounts for multiple measurements per individual obtained at different time points. All analyses were conducted using a random coefficient model with the intercept being random and a covariance structure of variance components. The covariates that were considered for potential inclusion into the models were age at surgery, sex, and type of surgery (primary versus revisional). Possible interactions of variables were tested via regression models. Kaplan–Meier survival estimates for the outcome of EWL < 50% (measurement of surgical success) were graphed over the follow-up period and compared using log-rank tests. All p values reported are two-tailed. Statistical significance was set at 0.05, and analyses were conducted using STATA statistical software (version 11.0).
Results
A total of 342 patients with mean age 43.8 years (SD = 11.2 years), 108 men and 234 women were included in the study. The mean follow-up period was 34 months (SD = 23.4) with median equal to 30 months (interquartile range 15 to 50 months). All patient data points were used up until 60 months after operation. Sample characteristics in total, and for the two different groups, primary laparoscopic Roux-en-Y gastric bypass (pLRYGB) and revisional laparoscopic Roux-en-Y gastric bypass (rLRYGB) are presented in Table 1. More women than men had a rLRYGB, while patients with rLRYGB were significantly older. Mean BMI at the time of gastric bypass was greater for the pLRYGB group. Operative time and duration of hospitalization were greater for revisional group. Also, conversion to open surgery was more frequent in the revisional operations. Number and type of complications are shown in Table 2. Twenty-six patients (7.6%) had postoperative complications, 16 patients (6.5%) in pLRYGB group, and 10 patients (10.3%) in rLRYGB group (p = 0.235). One patient from the pLRYGB died from acute necrotizing pancreatitis. Most frequent complications were fistula (1.2%) and intestinal obstruction (1.2%). No leak was observed from the gastrojejunal anastomosis itself. One leak was observed from the vertical staple line of the gastric pouch, just beneath the angle of His, two leaks from the staple line of the blind loop of the intestinal resection margin and one leak from the jejuno-jejunal anastomosis.
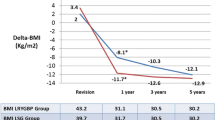
Table 3 shows BMI and % EBMIL for all-time points.
Revisional LRYGB group had significantly greater BMI at 12, 18, and 24 months of follow-up compared to pLRYGB group. %EBMIL for rLRYGB group as calculated by using the initial BMI before gastroplasty was significantly lower compared to pLRYGB group for all-time points except at 36 months. On the other hand, %EBMIL for rLRYGB group as calculated using the BMI before revision was significantly lower for the revisional group only the first 12, 18, and 24 months of follow-up and not after.
Linear prediction of BMI and %EBMIL at the time of revision and before initial gastroplasty for rLRYGB and for pLRYGB groups were reported in Figs. 1, 2, 3, and 4.
Discussion
The main finding of our study is that the %EBMIL was significantly lower in revisional RYGBP, compared to primary procedures, at almost all-time points, as found by most of other investigators in the literature [17,18,19,20,21,22,23]. We documented a diminishing efficacy of bariatric operations over time, both primary and revisional, as shown by the increase in BMI and the decrease of %EBMIL. Our unique finding was that the progress of weight loss in the first period and weight regain afterwards are similar in both groups. We identified the time of 18 months after bypass (either primary or revisional) as a critical point when minimum BMI and maximal weight loss were achieved. From that point on, both groups had a similar trend of weight regain. Gradual increase of BMI and decrease of the %EBMIL implied a progressive regain of weight in almost the same manner in both groups over a 1.5-year follow-up. An interesting point was the tendency of the rLRYGB group to have a smaller increase of BMI and lower decrease of EBMIL after this period, which indicates a more stable weight over time, comparing to pLRYGB. Further studies are probably needed to confirm this result.
Weight loss calculations using the Acholonu formulas and taking as initial weight, the weight before initial restrictive surgery, and the weight before revision [12]. We used %EBMIL as a more precise and indicative formula. We believe that weight loss calculations should be done by considering the weight before any bariatric surgery as the initial weight.
As our study is not a case-matched analysis, patients of different groups have different starting point of initial weight and variable comorbidities, which could influence the final postoperative body weight. Data collection was done retrospectively, including all patients operated and monitored by the same surgeon, therefore tracking the entire relevant group with no exclusions, though there may be other sources of bias.
Revisional bariatric surgery and especially by laparoscopic access has been considered a high risk and demanding surgery that should be performed by experienced surgeons in specialized referral centers. We presented a statistically longer operative time, a half day longer duration of hospitalization and a higher conversion rate for revisional bypass operations, comparing to primary operations, similar to other investigators [26,25,26,27,28,29,30,31,34].
The overall complication rate of 7.6% was similar to some previously published studies [6, 23, 35]. Other investigators suggested a higher complication rate for revisional surgery up to 50% [28] or from 0 to 39.9% in the comparative studies [18, 33]. In a case-matched analysis, Mor et al. [20] reported a higher morbidity rate of 27 versus 8.1% in primary operations. Perathoner et al. reported an early postoperative complication rate of 10.2 and 26% of re-operations in revisional cases [35].
Anastomotic leakage is the main cause of morbidity in bariatric surgery. We found no significant difference in leakage rates between primary and revisional operations. Leakage rate was 2.1% in revisional operations, comparable to the 3.3 and 3.6% in other studies [22, 36]. In a recent retrospective review of 3828 gastric bypass procedures, anastomotic leaks following revisional operations occurred in 8% of cases, while after primary LRYGB, the leak rate was 5.2% [37].
In this series, we reported less than 1% of gastrojejunal stricture in both groups, compared to 5.5% following primary and 18.5% following secondary operations in the series reported by Cadiere et al. [17]. We believe the hand-sewn standardized technique by a single surgeon in this series does play a major role in the low incidence [38, 39]. A conclusive view of surgical techniques and suturing has always been difficult, and not many comparable studies exist. A more thorough investigation between different techniques could offer valuable information on problems such as leaking and stenosis.
In our study, we reported a non-statistically significant difference of actual BMI between both groups of investigation after 5 years of follow-up (33.1 kg/m2 for revisional versus 31.5 for primary), comparable with the longest follow-up in the literature [35]. Several other investigators presented similar results [17, 22,23,24,27, 29].
At 5 years follow-up, Perathoner et al. [35] reported final EBMIL percentages of 79% of weight before initial procedure and 70% of weight before revision. In our study, at 5 years follow-up, revisional operations had 60.5% of EBMIL in total and only 44.4% of initial weight before revision. The corresponding EBMIL for primary operations in our study was 72% at 5 years, not significantly higher if we consider initial weight before any restrictive operation (Table 3).
Topart et al. [23] reported comparable results for weight loss and morbidity between revisional LYRGB after failed AGB, and primary LRYGB at 1-year follow-up, with reference to initial BMI before any surgery [23]. Mor et al. showed a significantly lower EWL in the revisional LRYGB in all periods examined (3, 6, and 12 months).
In conclusion, in this comparative study, we clearly showed that trends of weight loss and weight regain were similar in both revisional and primary bypass, with a crucial point of 1.5 years after surgery, when weight regain started. We also show that revisional gastric bypass after AGB and VGB has acceptable, satisfactory, and comparable results with the primary gastric bypass in the long term.
These results can clarify the limits of revisional surgery results in achieving weight loss and the risk of weight regain over long time periods.
A clear understanding of the patterns of weight loss over time can help physicians and patients to select appropriate medical and lifestyle adaptations to optimize their results.
References
Sarr M. Reoperative bariatric surgery. Surg Endosc. 2007;21:1909–13.
Behrns KE, Smith CD, Kelly KA, et al. Reoperative bariatric surgery: lessons learned to improve patient selection and results. Ann Surg. 1993;218:646–53.
Nesset EM, Houghton SG, Mai JL, et al. A two-decade spectrum of revisional bariatric surgery at a tertiary referral center. Surg Obes Relat Dis. 2007;3:25–30.
van Gemert WG, van Wersch MM, Greve JW, et al. Revisional surgery after failed vertical banded gastroplasty: restoration of vertical banded gastroplasty or conversion to gastric bypass. Obes Surg. 1998;8(1):21–8.
Fournier P, Gero D, Dayer-Jankechova A, et al. Laparoscopic Roux-en-Y gastric bypass for failed gastric banding: outcomes in 642 patients. Surg Obes Relat Dis. 2016;12(2):231–9.
Slegtenhorst BR, van der Harst E, Demirkiran A, et al. Effect of primary versus revisional Roux-en-Y gastric bypass: inferior weight loss of revisional surgery after gastric banding. Surg Obes Relat Dis. 2013;9(2):253–8.
Suter M, Calmes JM, Paroz A, et al. A 10-year experience with laparoscopic gastric banding for morbid obesity: high long-term complication and failure rates. Obes Surg. 2006;16:829–35.
Weber M, Müller MK, Michel JM, et al. Laparoscopic Roux-en-Y gastric bypass, but not rebanding, should be proposed as rescue procedure for patients with failed laparoscopic gastric banding. Ann Surg. 2003;238(6):827–33.
Vasas P, Dillemans B, Van Cauwenberge S, et al. Short- and long-term outcomes of vertical banded gastroplasty converted to Roux-en-Y gastric bypass. Obes Surg. 2013;23(2):241–8.
Elnahas A, Graybiel K, Farrokhyar F, et al. Revisional surgery after failed laparoscopic adjustable gastric banding: a systematic review. Surg Endosc. 2013;27(3):740–5.
Reinhold RB. Critical analysis of long term weight loss following gastric bypass. Surg Gynecol Obstet. 155:385–94.
Acholonu E, McBean E, Court I, et al. Safety and short-term outcomes of laparoscopic sleeve gastrectomy as a revisional approach for failed laparoscopic adjustable gastric banding in the treatment of morbid obesity. Obes Surg. 2009;19(12):1612–6.
Deitel MD, Gawdat K, Melissas J. Reporting weight loss 2007. Obes Surg. 2007;17:565–8.
Dixon JB, McPhail T, O’ Brien PE. Minimal reporting requirements for weight loss: current methods not ideal. Obes Sirg. 2005;15:1034–9.
American Society for Bariatric Surgery Standards Committee, 2004–2005, Oria HE, Carrasquilla C, et al. Guidelines for weight calculations and follow-up in bariatric surgery. Surg Obes Relat Dis. 2005;1(1):67–8.
Kuczmarski RJ, Flagel KM. Criteria for definition of overweight in transition: background and recommendations for the United States. Am J Clin Nutr. 2000;72:1074–81.
Cadiere GB, Himpens J, Bazi M, et al. Are laparoscopic gastric bypass after gastroplasty and primary laparoscopic gastric bypass similar in terms of results? Obes Surg. 2011;21:692–8.
Jennings NA, Boyle M, Mahawar K, et al. Revisional laparoscopic Roux-en-Y gastric bypass following failed laparoscopic adjustable gastric banding. Obes Surg. 2013;23(7):947–52.
Zingg U, McQuinn A, DiValentino D, et al. Revisional vs. primary Roux-en-Y gastric bypass—a case-matched analysis: less weight loss in revisions. Obes Surg. 2010;20:1627–32.
Mor A, Keenan E, Portenier D, et al. Case-matched analysis comparing outcomes of revisional versus primary laparoscopic Roux-en-Y gastric bypass. Surg Endosc. 2013;27(2):548–52.
Martin MJ, Mullenix PS, Steele SR, et al. A case-match analysis of failed prior bariatric procedures converted to resectional gastric bypass. Am J Surg. 2004;187:666–670 discussion 670–671.
te Riele WW, Sze YK, Wiezer MJ, et al. Conversion of failed laparoscopic gastric banding to gastric bypass as safe and effective as primary gastric bypass in morbidly obese patients. Surg Obes Relat Dis. 2008;4:735–9.
Topart P, Becouarn G, Ritz P. One-year weight loss afterprimary or revisional Roux-en-Y gastric bypass for failed adjustable gastric banding. Surg Obes Relat Dis. 2009;5(4):459–62.
Delko T, Köstler T, Peev M, et al. Revisional versus primary Roux-en-Y gastric bypass: a case-matched analysis. Surg Endosc. 2014;28(2):552–8.
Spyropoulos C, Kehagias I, Panagiotopoulos S, et al. Revisional bariatric surgery: 13-year experience from a tertiary institution. Arch Surg. 2010;145:173–7.
Jones Jr KB. Revisional bariatric surgery—potentially safe and effective. Surg Obes Relat Dis. 2005;1:599–603.
Khoursheed MA, Al-Bader IA, Al-Asfar FS, et al. Revision of failed bariatric procedures to Roux-en-Y gastric bypass (RYGB). Obes Surg. 2011;21:1157–60.
Schwartz RW, Strodel WE, Simpson WS, et al. Gastric bypass revision: lessons learned from 920 cases. Surgery. 1988;104:806–12.
Owens BM, Owens ML, Hill CW. Effect of revisional bariatric surgery on weight loss and frequency of complications. Obes Surg. 1996;6:479–84.
Suter M, Giusti V, Heraief E, et al. Laparoscopic Roux-en-Y gastric bypass initial 2-year experience. Surg Endosc. 2003;17:603–9.
Sugerman HJ, Kellum Jr JM, DeMaria EJ, et al. Conversion of failed or complicated vertical banded gastroplasty to gastric bypass in morbid obesity. Am J Surg. 1996;171:263–9.
Mognol P, Chosidow D, Marmuse JP. Roux-en-Y gastric bypass after failed vertical banded gastroplasty. Obes Surg. 2007;17:1431–4.
Gagner M, Gentileschi P, de Csepel J, et al. Laparoscopic reoperative bariatric surgery: experience from 27 consecutive patients. Obes Surg. 2002;12:254–60.
Deylgat B, D'Hondt M, Pottel H, et al. Indications, safety, and feasibility of conversion of failed bariatric surgery to Roux-en-Y gastric bypass: a retrospective comparative study with primary laparoscopic Roux-en-Y gastric bypass. Surg Endosc. 2012;26(7):1997–2002.
Perathoner A, Zitt M, Lanthaler M, et al. Long-term follow-up evaluation of revisional gastric bypass after failed adjustable gastric banding. Surg Endosc. 2013 Jun;27:4305–12.
Hedberg J, Gustavsson S, Sundbom M. Long-term follow-up in patients undergoing open gastric bypass as a revisional operation for previous failed restrictive procedures. Surg Obes Relat Dis. 2012;8:696–701.
Lee S, Carmody B, Wolfe L, et al. Effect of location and speed of diagnosis on anastomotic leak outcomes in 3828 gastric bypass cases. J Gastrointest Surg. 2007;11:708–13.
Kravetz AJ, Reddy S, Murtaza G, et al. A comparative study of handsewn versus stapled gastrojejunal anastomosis in laparoscopic Roux-en-Y gastric bypass. Surg Endosc. 2011;25(4):1287–92.
Gonzalez R, Lin E, Venkatesh KR, et al. Gastrojejunostomy during laparoscopic gastric bypass: analysis of 3 techniques. Arch Surg. 2003;138:181–4.
Author information
Authors and Affiliations
Contributions
Dimitrios Dardamanis: has done the study design and the data collection, and participated in the operations and follow-up consulting and writing of the manuscript.
JulieNavez: data collection, follow-up consulting, and data analysis.
Laurent Coubeau: data collection and follow-up consultation.
Benoit Navez: has performed all the operations, coordinated the team, final corrections.
All authors approve the final version of the submission.
Corresponding author
Ethics declarations
Conflicts of Interest Statement
The authors declare that they have no conflict of interest.
Ethical Approval Statement
For this type of study, formal consent is not required.
Informed Consent
Does not apply.
Rights and permissions
About this article
Cite this article
Dardamanis, D., Navez, J., Coubeau, L. et al. A Retrospective Comparative Study of Primary Versus Revisional Roux-en-Y Gastric Bypass: Long-Term Results. OBES SURG 28, 2457–2464 (2018). https://doi.org/10.1007/s11695-018-3186-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3186-z