Abstract
Objective
The study was designed to examine changes of body fat distribution after laparoscopic sleeve gastrectomy (LSG) in obese male patients and to confirm whether these changes are correlated with increased testosterone.
Methods
A total of 30 obese male patients with body mass index (BMI) 30–45 kg/m2 were enrolled in this study. Data on demographic characteristics, anthropometry, metabolic parameters, and body fat distribution were collected at baseline and 6 months after LSG. Body fat distribution was assessed by dual-energy X-ray absorptiometry (DXA).
Results
Six months after surgery, the BMI of participants (age 33.0 ± 9.5) decreased from 40.2 ± 5.2 to 30.8 ± 4.4 kg/m2, total testosterone increased from 2.4 ± 1.2 to 4.5 ± 1.8 ng/mL, and the percentage of testosterone deficiency in these patients decreased from 82.7 to 23.1%. Fat mass was significantly decreased in all regions, but the loss of fat mass in the android region was more than that in any other body region. After adjusting age and the BMI, the changes in android FM% and gynoid FM% were significantly correlated with an increase in total testosterone concentration (R2 = 0.187, R2 = 0.282, respectively).
Conclusion
In obese male patients with BMI 30–45 kg/m2, an increase of total testosterone correlated to the changes in android FM% and gynoid FM% at the sixth month after LSG surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity has become a severe public health problem in the world and is an important risk factor of metabolic diseases such as diabetes, fatty liver, hypertension, and cardiovascular diseases. Male obesity can also be associated with hypogonadism, which is characterized by low testosterone level, sexual dysfunction, and sterility [1, 2]. The role of testosterone in the development of obesity has been observed. In aging males, decreased testosterone is related to increase percentage of body fat [1, 3, 4]. Male patients with prostate cancer who accepted androgen deprivation therapy have low testosterone level along with abdominal fat accumulating [5], whereas testosterone supplementation in patients with testosterone deficiency contributes to reduced fat mass as well as improvement in weight loss [6, 7].
As we know, laparoscopic sleeve gastrectomy (LSG) is a successful and safe restrictive bariatric procedure to treat morbid obesity. Recently, several studies have demonstrated that weight loss surgery could reverse testosterone levels in obese male patients, resulting in an increase in testosterone levels [8,9,10]. Meanwhile, the impact of testosterone on body fat distribution patterns has been widely observed, and low testosterone levels are associated with abdominal and visceral obesity in cross-sectional and longitudinal studies [11,12,13]. All above data suggested a bidirectional relationship between testosterone and fat mass in men. However, knowledge about the association between increased testosterone and the body fat distribution changes after LSG in men is still very limited. Thus, our study aims to evaluate the changes in body fat distribution after laparoscopic sleeve gastrectomy (LSG) and to confirm whether these changes are correlated with increased testosterone in obese male patients.
Methods
A total of 30 obese male patients were consecutively enrolled in this study. General inclusion criteria were ages 20–55 years, BMI > 35 kg/m2, or a BMI > 30 kg/m2 with two or more obesity-related comorbidities such as diabetes mellitus type 2, hypertension, hypertriglyceridemia, or non-alcoholic fatty liver disease but otherwise healthy [14]. The exclusion criteria were as follows: (1) renal dysfunction, (2) severe liver dysfunction—aspartate aminotransferase (AST) or alanine aminotransferase (ALT) levels more than three times the normal value—(3) a history of preexisting heart disease, (4) presence of malignant tumor, (5) taking medications known to affect body weight such as glucocorticoid in the 3-month period prior to this study, and (6) secondary obesity caused by endocrine disorders such as Cushing’s syndrome and hypothyroidism. Testosterone deficiency was defined as serum total testosterone below 3.0 ng/mL [15,16,17]. The operation was performed by the professional surgeon under standard procedure, and no complications was found until now. Informed consent was obtained from all individual participants included in the study.
Clinical evaluation was obtained at baseline and 6 months after the surgery. All the patients underwent a physical examination (including measurements of height, weight, waist circumference (WC), systolic blood pressure (SBP), and diastolic blood pressure (DBP)). Laboratory test parameters were obtained by serum measurement in the next morning after patients’ admission, including total cholesterol (TC), triglyceride (TG), free fatty acid (FFA), high-density lipoprotein (HDL), low-density lipoprotein (LDL), follicle-stimulating hormone (FSH), luteinizing hormone (LH), total testosterone, estradiol (E2), sex hormone-binding globulin (SHBG), glycosylated hemoglobin A1c (HbA1c), and fasting plasma glucose (glucose 0 min) and fasting C-peptide (C-peptide 0 min). SHBG was tested by means of an immunochemiluminometric assay. Free testosterone concentrations were calculated by the Sartorius’s formula, which has been widely adopted in the literature [18,19,20]. Body fat mass and fat distribution (whole body, trunk, arms, legs, android, and gynoid) were measured with high accuracy by DXA (Hologic QDR4500, USA) at baseline and 6 months after the surgery. Percentage of fat mass (%FM) was calculated by the whole fat mass or each tested body region divided by the total weight of the whole body or each region, respectively. Trunk FM% is the sum of android FM% and gynoid FM%.
Statistical Analysis
All analyses were performed using SPSS 20.0 software. All continuous values were expressed as means ± standard deviation (SD) for normal distribution and median (upper and lower quartiles) for skewed distribution. Standard t test was used to compare the indexes at baseline and 6 months after LSG. Pearson’s correlation analysis was used to investigate the relationship of two indices. Linear regression analysis was performed to analyze the association between the changes in different regions of fat mass and variance of total testosterone. A value of P < 0.05 was considered statistically significant.
Results
Clinical Characteristics and Changes in Anthropometric Variables
Clinical characteristics of 30 men participating in the study are summarized in Table 1. Mean age of the population was 33.0 ± 9.5 years old, the mean body weight was 125.0 ± 18.1 kg, and the mean BMI was 40.2 ± 5.2 kg/m2. Hormonal analyses at baseline showed a mean TT of 2.4 ± 1.2 ng/mL, with values below the 3 ng/mL in 82.7% of patients. Six months after the surgery, participants’ BMI, HbA1c, fasting glucose, fasting C-peptide, and TG decreased significantly, while HDL, TT, cFT, and SHBG increased significantly, and the percentage of patients of testosterone deficiency (< 3 ng/mL) reduced to 23.1% (P < 0.001). TC, LDL, LH, FSH, and E2 failed to reach a statistical significance after 6 months.
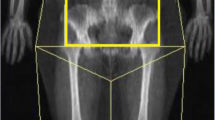
Body Fat Distribution at Baseline and 6 Months After LSG Surgery
As is shown in Fig. 1a, there was a significant decrease in all regions of fat mass at the sixth month after LSG, including total, trunk, android, gynoid, arm, and leg (P < 0.001). The loss of percentage of fat mass in whole body, trunk, android, gynoid, arm, and leg was significantly decreased 6 months later compared to the baseline (Fig. 1b). The more loss of fat mass (7.5%) in the android region was observed than in any other body region (Fig. 1b).
Body fat distribution at baseline and 6 months after LSG surgery. *P < 0.001. a There was a significant decrease in all regions of fat mass at the sixth month after LSG, including total, trunk, android, gynoid, arm, and leg (P < 0.001). b The loss of percentage of fat mass in whole body, trunk, android, gynoid, arm, and leg was significantly decreased 6 months later compared to the baseline
Correlation Between the Change in Total Testosterone and Body Fat Distribution After LSG Surgery
As shown in Table 2, increased total testosterone was significantly correlated with the variation in total fat, trunk fat, android fat, gynoid fat, arm fat, and leg fat, respectively (P < 0.05). In order to evaluate the contribution of fat loss in each body parts and its relationship with total testosterone concentration, the linear regression analysis was performed (Table 3). Fat mass and percentage of fat in four regions (arm, leg, android, and gynoid) were analyzed. After adjusting the age and the BMI, the changes in the percentage fat mass of android and gynoid were significantly correlated with total testosterone concentration variation (R2 = 0.187, R2 = 0.282, respectively).
Discussion
Many observational studies have reported that male obesity is often accompanied with low testosterone level, and marked weight loss is helpful to improve testosterone level in male [10, 20]. However, the association between increased testosterone and changes in body fat distribution after weight loss in men is still limited. In the present study, we provided the first evidence that the changes of android and gynoid fat in obese male patients with BMI 30–45 kg/m2 were significantly correlated with the improvement of total testosterone concentration after LSG.
In our study, the mean BMI for those patients was 40.58 ± 5.88 kg/m2, and 82.7% of them were considered to have testosterone deficiency before surgery. The findings were consistent with previous studies that showing approximately 75% of men with obesity grade III awaiting bariatric surgery had testosterone deficiency [10]. We also observed that an increase in testosterone levels and a decrease in the percentage of testosterone deficiency (P < 0.001) after LSG 6 months later were in line with previous studies [8, 9, 21]. It was reported that an increase in total testosterone levels after bariatric surgery was greater than expected based on weight loss [9, 10], suggesting a close association between increased testosterone levels and weight loss. Moreover, the effect of testosterone on body fat distribution has been widely observed, and low testosterone levels are associated with abdominal and visceral obesity [6]. Thus, we further evaluated the change of body fat distribution after LSG and tried to verify whether these changes are correlated with increased testosterone in obese male patients. All the patients were measured by DXA to accurately determine the body fat distribution and central obesity [22,23,24].
Our findings indicate that there was a significant decrease in the total and regional fat mass as well as the percentage of fat mass of the whole body at the sixth month after LSG. Although all the fat mass of the whole body decreased significantly, the change of fat mass loss in the android region was more than that in any other body region. This is in consistent with the findings by others [25]. As we know, android fat mass represents central obesity and this result suggested that central obesity was improved more after LSG, which was also supported by significantly decreased waist circumference after LSG in those patients.
In our study, although variations in body fat in each tested body region were associated with the improvement in total testosterone, only the percentage of fat mass decreasing in android and gynoid was significantly correlated with an increase in total testosterone independent of age and BMI. The findings were generally in line with previous studies showing that males have a greater amount of abdominal fat mass compared with both premenopausal and postmenopausal women [26,27,28,29] and males could lead to significant reductions in abdominal fat mass after testosterone supplementation [30, 31]. However, whether an increased total testosterone was due to a decrease in abdominal subcutaneous adipose tissue and/or visceral adipose tissue is unclear. Considering that visceral fat could increase leptin levels and easily leads to hypogonadism, reducing leptin levels by visceral fat loss could contribute to an increase in gonadotropin release, leading to increased testosterone [32].
It was reported that both aromatase levels and activity might be down-regulated by rapid weight loss, leading to increased testosterone and reduced estrogen levels [33]. In addition, elevated SHBG levels could be also related to an increase in total testosterone. Our data showed a significant increase in SHBG after surgery, which might, at least partly, explain the improvement in total testosterone. There were no significant differences between variations in LH, E2, and total testosterone levels, suggesting that the effects of these two hormones on increased testosterone are limited.
However, the underlying pathophysiology of the improvement in total testosterone after marked decrease in abdominal fat mass is still unclear. Many studies have shown that androgens may alter adipose tissue mass in a depot-specific manner by site-specific modulation of preadipocyte proliferation and/or differentiation as well as lipid synthesis and/or lipolysis in mature adipocytes [11, 34]. It is uncertain whether decreased abdominal fat mass affecting testosterone level could occur through the same mechanism.
There were still some limitations in our study. The clinical features of testosterone deficiency were not included in our study and 6 months might be too early to determine the real changes of body fat and the need for a longer follow-up. More observational studies are required to confirm the findings.
Conclusion
In the population of Chinese obese male with BMI 30–45 kg/m2, the relative change of fat mass loss in the android region was more than that in any other body region after LSG 6 months later, and increased total testosterone correlated to the more loss in android and gynoid fat.
References
Tajar A, Forti G, O'Neill TW, et al. Characteristics of secondary, primary, and compensated hypogonadism in aging men: evidence from the European male ageing study. J Clin Endocrinol Metab. 2010;95(4):1810–8. https://doi.org/10.1210/jc.2009-1796.
Kelly DM, Jones TH. Testosterone and obesity. Obes Rev. 2015;16(7):581–606. https://doi.org/10.1111/obr.12282.
Bann D, Wu FC, Keevil B, et al. Changes in testosterone related to body composition in late midlife: findings from the 1946 British birth cohort study. Obesity (Silver Spring). 2015;23(7):1486–92. https://doi.org/10.1002/oby.21092.
Couillard C, Gagnon J, Bergeron J, et al. Contribution of body fatness and adipose tissue distribution to the age variation in plasma steroid hormone concentrations in men: the HERITAGE Family Study. J Clin Endocrinol Metab. 2000;85(3):1026–31. https://doi.org/10.1210/jcem.85.3.6427.
Foulkes SJ, Daly RM, Fraser SF. The clinical importance of quantifying body fat distribution during androgen deprivation therapy for prostate cancer. Endocr Relat Cancer. 2017;24(3):R35–48. https://doi.org/10.1530/ERC-16-0505.
Frederiksen L, Hojlund K, Hougaard DM, et al. Testosterone therapy decreases subcutaneous fat and adiponectin in aging men. Eur J Endocrinol. 2012;166(3):469–76. https://doi.org/10.1530/EJE-11-0565.
Giannoulis MG, Martin FC, Nair KS, et al. Hormone replacement therapy and physical function in healthy older men. Time to talk hormones? Endocr Rev. 2012;33(3):314–77. https://doi.org/10.1210/er.2012-1002.
Botella-Carretero JI, Balsa JA, Gomez-Martin JM, et al. Circulating free testosterone in obese men after bariatric surgery increases in parallel with insulin sensitivity. J Endocrinol Investig. 2013;36(4):227–32. https://doi.org/10.3275/8469.
Calderon B, Galdon A, Calanas A, et al. Effects of bariatric surgery on male obesity-associated secondary hypogonadism: comparison of laparoscopic gastric bypass with restrictive procedures. Obes Surg. 2014;24(10):1686–92. https://doi.org/10.1007/s11695-014-1233-y.
Luconi M, Samavat J, Seghieri G, et al. Determinants of testosterone recovery after bariatric surgery: is it only a matter of reduction of body mass index? Fertil Steril. 2013;99(7):1872–9 e1871. https://doi.org/10.1016/j.fertnstert.2013.02.039.
O'Reilly MW, House PJ, Tomlinson JW. Understanding androgen action in adipose tissue. J Steroid Biochem Mol Biol. 2014;143:277–84. https://doi.org/10.1016/j.jsbmb.2014.04.008.
Navarro G, Allard C, Xu W, et al. The role of androgens in metabolism, obesity, and diabetes in males and females. Obesity (Silver Spring). 2015;23(4):713–9. https://doi.org/10.1002/oby.21033.
Mammi C, Calanchini M, Antelmi A, et al. Androgens and adipose tissue in males: a complex and reciprocal interplay. Int J Endocrinol. 2012;2012:789653.
Rosenthal RJ, International Sleeve Gastrectomy Expert P, Diaz AA, et al. International Sleeve Gastrectomy Expert Panel Consensus Statement: best practice guidelines based on experience of >12,000 cases. Surg Obes Relat Dis. 2012;8(1):8–19. https://doi.org/10.1016/j.soard.2011.10.019.
Li Y, Zhang M, Liu X, et al. Correlates and prevalence of hypogonadism in patients with early- and late-onset type 2 diabetes. Andrology. 2017;5(4):739–43. https://doi.org/10.1111/andr.12360.
Cooper LA, Page ST, Amory JK, et al. The association of obesity with sex hormone-binding globulin is stronger than the association with ageing—implications for the interpretation of total testosterone measurements. Clin Endocrinol. 2015;83(6):828–33. https://doi.org/10.1111/cen.12768.
Bhasin S, Cunningham GR, Hayes FJ, et al. Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010;95(6):2536–59. https://doi.org/10.1210/jc.2009-2354.
Sartorius G, Ly LP, Sikaris K, et al. Predictive accuracy and sources of variability in calculated free testosterone estimates. Ann Clin Biochem. 2009;46(Pt 2):137–43. https://doi.org/10.1258/acb.2008.008171.
Ly LP, Sartorius G, Hull L, et al. Accuracy of calculated free testosterone formulae in men. Clin Endocrinol. 2010;73(3):382–8. https://doi.org/10.1111/j.1365-2265.2010.03804.x.
Keelan JA, Mattes E, Tan H, et al. Androgen concentrations in umbilical cord blood and their association with maternal, fetal and obstetric factors. PLoS One. 2012;7(8):e42827. https://doi.org/10.1371/journal.pone.0042827.
Aarts E, van Wageningen B, Loves S, et al. Gonadal status and outcome of bariatric surgery in obese men. Clin Endocrinol. 2014;81(3):378–86. https://doi.org/10.1111/cen.12366.
Corona G, Rastrelli G, Monami M, et al. Body weight loss reverts obesity-associated hypogonadotropic hypogonadism: a systematic review and meta-analysis. Eur J Endocrinol. 2013;168(6):829–43. https://doi.org/10.1530/EJE-12-0955.
Mouser JG, Loprinzi PD, Loenneke JP. The association between physiologic testosterone levels, lean mass, and fat mass in a nationally representative sample of men in the United States. Steroids. 2016;115:62–6. https://doi.org/10.1016/j.steroids.2016.08.009.
Morrison SA, Goss AM, Azziz R, et al. Peri-muscular adipose tissue may play a unique role in determining insulin sensitivity/resistance in women with polycystic ovary syndrome. Hum Reprod. 2017;32(1):185–92. https://doi.org/10.1093/humrep/dew279.
Li W, Zhu L, Mo Z, et al. Effect of laparoscopic Roux-en-Y gastric bypass on body composition and insulin resistance in Chinese patients with type 2 diabetes mellitus. Obes Surg. 2014;24(4):578–83. https://doi.org/10.1007/s11695-013-1116-7.
Krotkiewski M, Bjorntorp P, Sjostrom L, et al. Impact of obesity on metabolism in men and women. Importance of regional adipose tissue distribution. J Clin Invest. 1983;72(3):1150–62. https://doi.org/10.1172/JCI111040.
Tchernof A, Despres JP. Pathophysiology of human visceral obesity: an update. Physiol Rev. 2013;93(1):359–404. https://doi.org/10.1152/physrev.00033.2011.
Kvist H, Chowdhury B, Grangard U, et al. Total and visceral adipose-tissue volumes derived from measurements with computed tomography in adult men and women: predictive equations. Am J Clin Nutr. 1988;48(6):1351–61. https://doi.org/10.1093/ajcn/48.6.1351.
Kuk JL, Lee S, Heymsfield SB, et al. Waist circumference and abdominal adipose tissue distribution: influence of age and sex. Am J Clin Nutr. 2005;81:1330–4.
Gruenewald DA, Matsumoto AM. Testosterone supplementation therapy for older men: potential benefits and risks. J Am Geriatr Soc. 2003;51(1):101–15; discussion 115. https://doi.org/10.1034/j.1601-5215.2002.51018.x.
Wittert GA, Chapman IM, Haren MT, et al. Oral testosterone supplementation increases muscle and decreases fat mass in healthy elderly males with low-normal gonadal status. J Gerontol A Biol Sci Med Sci. 2003;58:618–25.
Caprio M, Fabbrini E, Isidori AM, et al. Leptin in reproduction. Trends Endocrinol Metab. 2001;12(2):65–72. https://doi.org/10.1016/S1043-2760(00)00352-0.
Laughlin GA, Ix JH, Cummins K, et al. Extremes of an aromatase index predict increased 25-year risk of cardiovascular mortality in older women. Clin Endocrinol. 2012;77(3):391–8. https://doi.org/10.1111/j.1365-2265.2011.04287.x.
Blouin K, Boivin A, Tchernof A. Androgens and body fat distribution. J Steroid Biochem Mol Biol. 2008;108(3-5):272–80. https://doi.org/10.1016/j.jsbmb.2007.09.001.
Acknowledgments
The present study would not have been possible without the participation of these patients. This study is supported by grants from the Chinese National Natural Science Foundation (No. 81601269) and Shanghai Sailing Program (16YF1408900).
Author information
Authors and Affiliations
Contributions
JG and MZ analyzed the data and drafted the manuscript. JG, MZ, and SQ designed the study and directed implementation and data collection. JG, CZ, XW, and YZ collected the data. QL and LL provided necessary logistical support. DZ performed the surgery and participated in the discussion of this manuscript. MZ and SQ edited the manuscript for intellectual content and provided critical comments on the manuscript.
Corresponding author
Ethics declarations
Informed consent was obtained from all individual participants included in the study. The study was approved by the ethics committee of Shanghai Tenth People’s Hospital.
Conflict of Interest
The authors declare no competing interests.
Rights and permissions
About this article
Cite this article
Gao, J., Zhang, M., Zhu, C. et al. The Change in the Percent of Android and Gynoid Fat Mass Correlated with Increased Testosterone After Laparoscopic Sleeve Gastrectomy in Chinese Obese Men: a 6-Month Follow-Up. OBES SURG 28, 1960–1965 (2018). https://doi.org/10.1007/s11695-018-3116-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3116-0