Abstract
Purpose
The purpose of this study is to evaluate the results of routine fluoroscopic swallowing study (FSS) imaging 24 h after surgery and computed tomography (CT) on demand based on clinical data, in diagnosing complications after bariatric surgery.
Material and Methods
This retrospective study includes 9386 patients that underwent bariatric surgery. A total of 3241 (34.53%) patients underwent FSS imaging following the surgical procedure, and 106 (1.13%) patients underwent CT.
Results
Sleeve gastrectomy was performed in 8093 patients (75.81%), gastric bypass was performed in 1281 patients (12%), duodenal switch or biliopancreatic diversion was performed in 12 patients (0.11%), and gastric banding was performed in 1289 patients (12.07%), which were excluded from the study as no imaging modality was used in any of these patients. The sensitivity for FSS was 71.43% and the specificity was 99.85%. An analysis of disease prevalence revealed a value of 0.43% with a positive predictive value of 66.67%. The sensitivity for CT was 71.42% and the specificity was 98%. A disease prevalence analysis revealed a value of 6.60% with a positive predictive value of 83.33%. A comparison of the two modalities showed that FSS has higher specificity values (p < 0.02) and a higher accuracy (p < 0.0001) than CT.
Conclusion
CT and FSS have a similar sensitivity for diagnosing complications after bariatric surgery. However, the specificity and accuracy of FSS are superior to that of CT. This study was approved by the instructional ethics committee (Helsinki board) and was registered on the National Institutes of Health (ClinicalTrials.gov) web site with identifier NCT02813122.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Obesity is adiposity based chronic disease characterized by an increase in the energy reserves in the form of fat [1] and consequently, an increase in weight resulting from a complex relationship between genetic, socioeconomic, and cultural influences [2]. Obesity is a worldwide epidemic causing serious deterioration in global health, affecting people of all ages, and leading to many preventable deaths. Any degree of overweight of obese people compared to normal weight persons is associated with significantly higher all-cause mortality [3]; therefore, member states of the World Health Organization (WHO) adopted in 2013 the Prevention and Control of Non-Communicable Diseases Global Action Plan including nine global targets to halt the increase in obesity by 2020 [4].
Obesity can be treated through medication [5], diet [6], physical activity [7], and behavioral changes [8]. Non-surgical management of obesity can effectively induce 5–10% weight loss and improve health in severely obese individuals [9]. However, non-surgical treatments for obesity are ineffective for long-term weight control [10].
Bariatric surgery for severe obesity is an effective treatment that results in the improvement and remission of much obesity-related comorbidity, provides sustained weight loss, and improves the patient’s quality of life [11]. Bariatric surgery induces a weight loss greater than 50% in morbidly obese individuals. It provides substantial and sustained weight loss effects and ameliorates obesity-attributable comorbidities in the majority of bariatric patients, although risks of complication, re-operation, and death exist [12]. Complication rates associated with bariatric surgery are in the range of 10 to 17%, and re-operation rates are approximately 7%; nonetheless, mortality associated with surgery is generally low (0.08–0.35%) [12]. Identification of complications should be done as soon as possible to prevent serious consequences.
This study aims to statistically compare the performance of a routine fluoroscopic swallowing study (FSS) imaging 24 h after surgery and computed tomography (CT) on demand based on clinical data, in diagnosing complications after bariatric surgery.
Materials and Methods
This study is a retrospective analysis of patients that underwent bariatric surgery at a private medical center from January 2013 to October 2016. We examined the effect of routine FSS imaging of the upper gastrointestinal tract using an oral administration of a water-soluble contrast agent 24 h after surgery, and computed tomography (CT) on demand during hospitalization, based on suspicious clinical signs, to diagnose postoperative complications after bariatric surgery. Laparoscopic gastric banding patients were excluded from this study as no imaging modality was used in these patients.
A comparison of clinical measures between patients who performed and did not perform FSS and CT was conducted.
Statistical Analysis
Statistical analyses were performed using SPSS software version 23. The continuous variables are presented as means ± SD, and the dichotomous/categorical variables are presented as percentages. The Kolmogorov-Smirnov test was used to assess the normality of the continuous variables’ distribution. If normality was rejected, non-parametric tests were used. p < 0.05 was selected as the p value for statistical significance. A specificity-sensitivity model was used to compare the FSS and CT modalities.
Ethical Approval Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Informed Consent Statement
Does not apply.
Results
Basic Demographics of the Study Population
Overall, 10,675 bariatric procedures were performed between January 2013 and October 2016. The mean age of the patients was 41 years (range, 18–81 years). The study sample included 3630 men (34%) and 7045 women (66%). The mean body mass index (BMI) was 41.52 kg/m2 (range 21 to 81 kg/m2). Patients who underwent surgery and have a BMI below 35 were those who needed conversion of a previous bariatric surgery and represent 2% (215 patients) of the cohort.
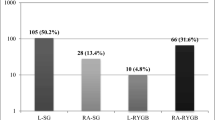
The distribution of the type of bariatric surgery performed was sleeve gastrectomy—8093 patients (75.81%), gastric bypass—1281 patients (12%), duodenal switch or biliopancreatic diversion—12 patients (0.11%), and gastric banding—1289 patients (12.07%). Laparoscopic surgery was successfully performed in 10,661 cases (99.87%). Open surgery was performed in 12 cases of revisional bariatric surgery, and in two cases, the laparoscopic sleeve gastrectomy was converted to open surgery. Gastric banding procedures were excluded from the study because most of them were released on the day of surgery without any imaging study needed, reducing the total number of cases included in the statistical analysis to 9386.
A total of 3241 (34.53%) patients underwent FSS following the surgical procedure, and 6145 patients (65.47%) did not undergo FSS. A total of 106 (1.13%) patients underwent CT following surgery, and 9280 (98.87%) patients did not undergo CT.
A total of 107 (1.14%) patients had complications that required re-operation with 27 (25.23%) of the 107 patients undergoing FSS and 80 (74.77%) undergoing CT.
Twenty-two of the sleeve gastrectomy patients and five gastric bypass patients that underwent FSS required postoperative surgical revision for complications. Fifty-nine of the sleeve gastrectomy patients, 20 of the gastric bypass patients, and one duodenal switch patient that underwent CT required additional surgical revisions for complications.
There were several reasons why additional surgery was required. The most common reasons were leaks in 27 cases (25.23%), bleeding in 50 cases (46.73%), gastric outlet obstruction in 14 cases (13.08%), and other reasons in 16 cases (14.95%). The calculated rates of complications that required re-operations are leak rate of 0.29%, bleeding rate of 0.53%, and obstruction rate of 0.15%. The basic demographics, complications, and re-operations are presented in Table 1.
Fluoroscopic Swallow Study (FSS) and Clinical Signs
We then evaluated the feasibility of FSS in locating possible complications among patients that underwent bariatric surgery. A comparison was conducted between the three most common types of complications (leaks, bleeding, and obstruction) in relation to the use of FSS or clinical evaluation alone: white blood cell (WBC) count, hemoglobin (HBG), fever, heart rate, pain evaluation, and days of hospitalization. We found a significant difference in the number of days of hospitalization between patients that underwent FSS and those that did not undergo FSS. The number of hospitalization days was significantly lower in complicated patients who did not undergo FSS (5.81 vs. 10.88, p < 0.05). No significant difference in terms of hemoglobin, white blood cells, fever, heart rate, or pain evaluation was found between these two groups. Table 2 presents the differences between the two groups.
Sensitivity and Specificity
In order to evaluate the diagnostic tools, we conducted a sensitivity and specificity analysis. We evaluated the true positive, false positive, true negative, and false negative findings of the imaging modalities among patients who underwent postoperative surgical revision due to complications. Our analysis examined FSS and CT modalities and conducted a comparison between the two methods.
Fluoroscopic Swallow Study (FSS)
The sensitivity for FSS was 71.43% and the specificity was 99.85%. An analysis of the disease prevalence revealed a value of 0.43% with the positive predictive value being 66.67%. The sensitivity and specificity data of the FSS are presented in Table 3.
For the next phase of the study, we aimed to achieve a better understanding of the specificity and sensitivity of FSS by comparing the most common complications. We divided the patients into three main groups based on the most common complications: leaks, bleeding, and obstruction. For the leaks group, the FSS sensitivity value was 83.33% and the specificity value was 100%. An analysis of the disease prevalence revealed a value of 0.19%, and the positive predictive value was 100%. For the bleeding group, the FSS sensitivity value was 0% and the specificity value was 100%. An analysis of the disease prevalence revealed a value of 0.43%. For the obstruction group, the FSS sensitivity value was 71.43% and the specificity value was 100%. An analysis of the disease prevalence revealed a value of 0.22% and the positive predictive value was 100%. A comparison of the accuracy between the different complication groups did not reveal any significant effect (p = 0.98).
Computed Tomography (CT)
The CT sensitivity was 71.42% and the specificity was 98%. An analysis of the disease prevalence revealed a value of 6.60% with a positive predictive value of 83.33%. The CT sensitivity and specificity data are presented in Table 4.
Comparison of FSS and CT
We performed a comparison of the sensitivity, specificity, and accuracy between the two imaging modalities. Significant differences were found in the specificity and accuracy. The FSS modality had higher levels than the CT modality for both parameters (p < 0.02 for specificity and p < 0.0001 for accuracy).
In addition, we compared all of the previously mentioned clinical parameters between complicated patients that underwent FSS and those that underwent CT. Our findings demonstrated a significant difference in pain evaluation. Patients who underwent a CT reported higher levels of pain than patients who underwent FSS. Furthermore, the length of hospital stay was significantly lower in complicated patients that underwent CT in comparison to those that underwent FSS (6.1 vs. 10.88, p < 0.05).
Discussion
Catastrophic consequences can occur due to complications after bariatric surgery [13, 14]. Based on a large number of patients, we evaluated the contributions of FSS and CT in diagnosing complications after bariatric surgery.
Among bariatric surgeons, there is still controversy whether to carry out imaging studies as FSS routinely or based only on the patient’s clinical parameters after the operation.
FSS is better used for detecting specific intraluminal problems in the stomach, anastomosis, or small bowel, and bariatric surgery patients commonly undergo a postoperative fluoroscopic evaluation for complications, including leaks, so that they can progress towards oral intake and recovery [15]. Figures 1, 2, and 3 show common complications as seen during the operation (Fig. 1) or on FSS (Figs. 2 and 3).
During the FSS, indirect signs could be observed as an unusual amount of pneumoperitoneum as suspicious of leakage (Fig. 4).
CTs can detect indirect extra-luminal signs of complications, such as small bubbles of free air, fatty tissue inflammation, small quantities of liquids, and the presence of abscesses. This has been demonstrated both in our work (Figs. 5 and 6) and in the literature [15,16,17].
It is initially important to analyze whether imaging studies should be conducted routinely or selectively. In reviewing the published medical literature, we found discrepancies in the usefulness of radiological studies to diagnose early complications after bariatric surgery [18, 19]. In our center, we have routinely performed FSS 24 h after an operation in third of the patients, operated by bariatric surgeons who believe that FSS adds a value in diagnosing early leaks and obstructions, yields rapid re-operation, and improves outcome. However, our study found that those who had a complication and performed FSS actually stayed longer, and had the same clinical parameters as those that did not perform FSS (Table 2), so we cannot conclude that routine FSS improves outcome.
The sensitivity and specificity values reported for FSS differ in different publications. Our study demonstrated an FSS sensitivity value of 71.43% and a specificity value of 99.85%. Bertelson [19] reported an FSS specificity of 100% for leaks and obstruction, agreeing with our results, and Upponi [20] described an FSS sensitivity of 100%, well above our results. Our results are in disagreement with Hamilton’s report of the low sensitivity of FSS to diagnose leaks [21]. The differences in the findings from these studies and ours can be explained by the number of patients included in the study. Our study had a large number of patients that underwent different bariatric procedures whereas Hamilton’s had 210 patients after gastric bypass.
Obstructions, leaks, and bleeding are the most frequent complications of bariatric surgery. When separately comparing the FSS results for each type of complication, no significant differences were found.
In our study, FSS was performed using only a water-soluble contrast agent, not barium. Use of barium may increase the FSS sensitivity, as proposed by Swanson [22]. The use of barium to enhance FSS sensitivity is problematic because it produces artifacts, in case that CT is necessary, and if the barium spills into the abdominal cavity, it may cause peritonitis, abscess, and granulomas [23,24,25].
When there is clinical evidence of suspected complications, CT offers a sensitivity of 71.42% which is similar to the sensitivity of FSS. Lainas proposed the routine use of CT on the second day after the operation and reported an overall sensitivity of 91.4% in detecting bleeding and hematomas. However, the CT sensitivity for leaks was found to be 46.4% [26]. These conflicting results do not justify the routine use of CTs. Rather, we agree with Mizrahi that CTs should only be used for selected cases taking into account the cost of a CT and the overload of unnecessary imaging studies [27].
Studies comparing FSS with CTs found significant differences in favor of CT in terms of specificity and accuracy. Binghman [28] reported that CT is a superior modality in comparison to an upper gastrointestinal (UGI) series for detecting staple line leaks following bariatric surgery, which is at odds with the findings in our study. Other authors have reported poor FSS results. Rawlins reported a very low sensitivity of 25% for FSS [29]. This outcome could be explained by the radiation values applied during the FSS, the amount of contrast medium given, and the experience of the radiologist.
Our results demonstrated statistically significant higher specificity and accuracy for FSS than CT in detecting postoperative complications. However, by comparing clinical parameters of complicated patients between those who underwent FSS and those who did not, our data demonstrate no significant difference in terms of fever, hemoglobin, pain, heart rate above 120, white blood cells count, and favorable hospitalization stay results for those who did not have FSS (Table 2). Our data rejects the use of FSS on a routine use since there is no difference in clinical parameters between the two groups.
This present study did not find any advantages in performing a routine FSS or CT to look for complications.
The use of the FSS has lost its validity in the last years with the advance of modern technologies. Fluoroscopy has evolved from the most simplistic of non-invasive imaging methods to a very sophisticated technology with advanced 3-D capabilities [30].
Limitations of our study include its retrospective nature, not being prospective and randomized. However, it shows that FSS and CT are still valuable tests.
Conclusion
CT and FSS have a similar sensitivity for diagnosing complications after bariatric surgery. However, the specificity and accuracy of FSS are superior to that of CT. Alterations in clinical signs and symptoms of the patient are still the best index to suspect complications. We believe that both imaging modalities should be used in diagnosing complications after bariatric surgery as complementary to the clinical features of the patient. New advanced equipment should be evaluated in the future.
References
Barbany M, Foz M. Obesity: concept, classification and diagnosis. An Sist Sanit Navar. 2002;25(Suppl 1):7–16.
Apovian CM. Obesity: definition, comorbidities, causes, and burden. Am J Manag Care. 2016;22:s176–85.
Flegal K, Kit B, Orpana H, et al. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309:71–82.
Follow-up to the political declaration of the high-level meeting of the General Assembly on the Prevention and Control of Non-Communicable Diseases, 2013. Geneva: World Health Assembly. http://apps.who.int/gb/ebwha/pdf_files/WHA66/A66_R10-en.pdf. Accessed 26 Jan 2014.
Li Z, Maglione M, Tu W, et al. Meta-analysis: pharmacologic treatment of obesity. Ann Intern Med. 2005;142(7):532–46.
Foster GD, Wyatt HR, Hill JO, et al. A randomized trial of a low-carbohydrate diet for obesity. N Engl J Med. 2003;348:2082–90.
Wing RR. Physical activity in the treatment of the adulthood overweight and obesity: current evidence and research issues. Med Sci Sports Exerc. 1999;31:S547–52.
Penick S, Filion R, Fox S, et al. Behavior modification in the treatment of obesity. Psychosom Med. 1971;33(1):49–55.
Ryan DH, Johnson WD, Myers VH, et al. Nonsurgical weight loss for extreme obesity in primary care settings: results of the Louisiana Obese Subjects Study. Arch Intern Med. 2010;170:146–54.
Chang SH, Pollack LM, Colditz GA. Obesity, mortality, and life years lost associated with breast cancer in nonsmoking US women, National Health Interview Survey, 1997–2000. Prev Chronic Dis. 2013;10:E186.
Nguyen N, Varela E. Bariatric surgery for obesity and metabolic disorders: state of the art. Nat Rev Gastroenterol Hepatol. 2016; https://doi.org/10.1038/nrgastro.2016.170.
Chang SH, Stoll CR, Song J, et al. The effectiveness and risks of bariatric surgery—an updated systematic review and meta-analysis, 2003–2012. JAMA Surg. 2014;149(3):275–87.
Patel S, Szomstein S, Rosenthal RJ. Reasons and outcomes of reoperative bariatric surgery for failed and complicated procedures (excluding adjustable gastric banding). Obes Surg. 2011;21:1209–19.
Comeau E, Gagner M, Inabnet WB, et al. Symptomatic internal hernias after laparoscopic bariatric surgery. Surg Endosc. 2005;19:34–9.
Xu T, Rosculet N, Steele K, et al. Comparison of upper gastrointestinal fluoroscopy versus computed tomography for evaluation of post-operative leak in a bariatric surgery patient. BJR Case Rep. 2016;2:20160076.
Shah S, Shah V, Ahmed AR, et al. Imaging in bariatric surgery: service set-up, post-operative anatomy and complications. Br J Radiol. 2014;84(998):101–11.
Kim TH, Kim JH, Shin CI, et al. CT findings suggesting anastomotic leak and predicting the recovery period following gastric surgery. Eur Radiol. 2015;25(7):1958–66.
Triantafyllidis G, Lazoura O, Sioka E, et al. Anatomy and complications following laparoscopic sleeve gastrectomy: radiological evaluation and imaging pitfalls. Obes Surg. 2011;21(4):473–8.
Bertelson NL, Myers JA. Routine postoperative upper gastrointestinal fluoroscopy is unnecessary after laparoscopic adjustable gastric band placement. Surg Endosc. 2010;24(9):2188–91.
Upponi S, Ganeshan A, D'Costa H, et al. Radiological detection of post-oesophagectomy anastomotic leak—a comparison between multidetector CT and fluoroscopy. Br J Radiol. 2008;81:545–8.
Hamilton EC, Sims TL, Hamilton TT, et al. Clinical predictors of leak after laparoscopic Roux-en-Y gastric- bypass for morbid obesity. Surg Endosc. 2003;17:679–84.
Swanson JO, Levine MS, Redfern RO, et al. Usefulness of high-density barium for detection of leaks after esophagogastrectomy, total gastrectomy, and total laryngectomy. Am J Roentgenol. 2003;181(2):415–20.
Leopold GR, Asher M. Deleterious effects of gastrointestinal contrast material on abdominal echography 1. Radiology. 1971;98(3):637–40.
Vessal K, Montali RJ, Larson SM, et al. Evaluation of barium and gastrografin as contrast media for the diagnosis of esophageal ruptures or perforations. AJR Am J Roentgenol. 1975;123(2):307–19.
Zheutlin N, Lasser EC, Rigler LG. Clinical studies on effect of barium in the peritoneal cavity following rupture of the colon. Surgery. 1952;32:967–79.
Lainas P, Tranchart H, Gaillard, et al. Prospective evaluation of routine early computed tomography scanner in laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2016;12(8):1483–90.
Mizrahi I, Tabak A, Grinbaum R, et al. The utility of routine postoperative upper gastrointestinal swallow studies following laparoscopic sleeve gastrectomy. Obes Surg. 2014;24(9):1415–9.
Bingham J, Shawhan R, Parker R, et al. Computed tomography scan versus upper gastrointestinal fluoroscopy for diagnosis of staple line leak following bariatric surgery. Am J Surg. 2015;209(5):810–4.
Rawlins L, Penn R, Schirmer B, et al. Accuracy of routine postoperative swallow study in predicting leak or obstruction after gastric bypass. Surg Obes Relat Dis. 2015;11(1):1–4.
Lottrup C, Gregersen H, Liao D, et al. Functional lumen imaging of the gastrointestinal tract. J Gastroenterol. 2015;50(10):1005–16.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Informed consent statement does not apply.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Susmallian, S., Folb, E., Barnea, R. et al. Comparison of Imaging Modalities for Detecting Complications in Bariatric Surgery. OBES SURG 28, 1063–1069 (2018). https://doi.org/10.1007/s11695-017-2970-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-2970-5