Abstract
Background
Laparoscopic adjustable gastric banding (LAGB) placements have progressively decreased in recent years. This is related to poor long-term weight loss outcomes and necessity for revision or removal of these bands. Long-term outcome results following LAGB are limited. The aim of our study was to determine the long-term outcome after LAGB at our institution.
Objectives
The aim of our study was to determine the long-term outcome after LAGB at our institution.
Setting
The setting of this is Academic Center, Israel.
Methods
Patients who underwent LAGB between 1999 and 2004 were reviewed. Patient comorbidities and weight loss parameters were collected preoperatively and at defined postoperative periods. Improvement in weight loss was defined as percent excess weight lost, and improvement in comorbidities was defined based on standardized reporting definitions.
Results
In total, 74 (80%) patients who underwent LAGB met inclusion criteria. The mean age at LAGB placement was 50.5 ± 9.6 years, and the mean body mass index (BMI) was 45.5 ± 4.8 kg/m2. Preoperative comorbidities were diabetes mellitus (13.5%), hypertension (32%), hyperlipidemia (12.1%), obstructive sleep apnea (5.4%), joints disease (10.8%), mood disorders (5.4%), and gastro-esophageal reflux disease (GERD) symptoms (8.1%). The mean follow-up was 162.96 ± 13.9 months; 44 patients (59.4%) had their band removed, and 22 (30%) had another bariatric surgery. The follow-up BMI was 35.7 ± 6.9 (p < 0.001), and the % total weight loss was 21.0 ± 0.13. There was no improvement in any of the comorbidities. GERD symptoms worsened at long-term follow-up (p < 0.001). Undergoing another bariatric procedure was associated with a higher weight loss (OR 12.8; CI 95% 1.62–23.9; p = 0.02).
Conclusion
LAGB required removal in the majority of our patients and showed poor resolution of comorbidities with worsening of GERD-related symptoms. Patients who go on to have another bariatric procedure have more durable weight loss outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bariatric surgery continues to be the most effective treatment for obesity and its associated comorbidities [1, 2]. Since 2015, sleeve gastrectomy (SG) is the most common bariatric procedure performed in the USA (53.8%) followed by Roux-en-Y gastric bypass (RYGB) (23.1%) and laparoscopic adjustable gastric banding (LAGB) (5.7%) [3]. In stark contrast to these statistics, LAGB represented 35.4% of the bariatric surgeries in the USA in 2011 [3]. The sharp decline in LAGB placement is related to moderate weight lost over the short term compared to the weight loss afforded by either RYGB or SG [4]. In addition, severe complications and band malfunctions, including slippage, erosions, and penetrations, have negatively affected patient quality of life and did not quite define LAGB as a reversible procedure [5,6,7].
Long-term outcome results after LAGB varies within the literature. There are some studies that claim that LAGB is a safe and effective long-term treatment option for obesity and that it is a safer procedure compared to other bariatric surgeries [8]. On the other hand, however, some studies actually report that weight loss and comorbidity results worsen over time [9,10,11,12]. Still, most case series report only relatively early results with a significant percentage of patients who were lost to follow-up. Due to the paucity of, and conflicting, long-term studies evaluating the effectiveness of LAGB, we investigated the long-term outcomes (over 10 years) of patients undergoing LAGB at our institution with respect to weight lost, cardiometabolic comorbidities, band complications, and reoperations.
Materials and Methods
Following the Hospital ethical committee approval, we retrospectively reviewed all patients who underwent LAGB from 1999 through 2004 at a single, university-affiliated teaching institution. Preoperative data collection included age, sex, weight, body mass index (BMI), and patient comorbidities. We specifically looked into the more common cardiometabolic comorbidities, including diabetes mellitus (DM), hypertension (HTN), hyperlipidemia (HPL), obstructive sleep apnea (OSA), joint disease (JD), mood disorders (MD), and gastro-esophageal reflux disease (GERD) symptoms. GERD symptoms included heartburn, epigastric pain, and dysphagia.
Procedure Technique
The procedure was done using four trocars and a 10-mm, 30° angled scope. The Lap-band® (Bioenterics, Carpinteria, CA, USA) or the Swedish adjustable gastric band—SAGB® (Ethicon Endo-Surgery, Obtech Medical, Zug, Switzerland)—were placed using the pars flaccida technique. This technique entailed opening of the lesser omentum, dissection at the base of the right crus, and creation of a retro-gastric channel around which the band was placed. The injection port was secured to the anterior rectus sheath and muscle with non-absorbable sutures. All bands were placed as elective procedures, and all patients were routinely discharged home on post-operative day number 1 after proved PO tolerance. The bands were not filled at the time of placement, and upper gastrointestinal contrast studies were not routinely performed before discharge.
Band adjustments were performed on an outpatient basis under radiological guidance. The band was filled during the first month appointment, and further adjustments were performed during follow-up as needed. Patients were also referred to the nutritionist in our service. Patients who failed to attend for their appointments and could not be reached by telephone or refused to attend the telephone questionnaire were excluded from the study.
Only patients who completed the follow-up requirements were included. Patients who remained with the band in place and those who had their band removed with or without a revision or subsequent bariatric procedure were included. The follow-up period was defined as 10 years minimum. Outcomes of interest included weight loss parameters at 1 year postoperatively and at long-term follow-up, success and failure rates of the band for resolution of comorbidities, and indication for band extraction and revisions. Weight loss parameters included percent of total weight lost (%TWL), percentage of excess weight lost (%EWL), and change in BMI. We calculated the excess weight (EW) from the weight before surgery minus the ideal body weight (IBW) for a BMI of 25 kg/m2. Resolutions of comorbidities were based on the ASMBS standardized outcome reporting in metabolic and bariatric surgery [13]. Data was abstracted from printed and electronic patient charts that recorded hospitalizations and office visits. A standardized telephone questionnaire was conducted for those patients who were lost to follow-up in order to collect information regarding their well-being, additional operations, current weight, and associated comorbidities. Patients were excluded from this analysis if they were lost to follow-up and unavailable for, or chose not to participate in, the follow-up phone questionnaire.
The indications for band extraction were classified into four groups. Technical failure was defined as tube or port displacement or infection. Band intolerance was defined as severe dysphagia or pain while the band was deflated and in normal position. Band erosion or penetration was diagnosed as visualization of the band through the stomach wall on upper endoscopy or CT scan. Slippage of the band was demonstrated on X-ray, upper GI, or CT scan as a dilated stomach cardia with a more horizontal or vertical angle of the band.
Data are presented as mean ± standard deviation. Comparisons between paired and unpaired parameters were performed using Student’s t test for continuous variables and chi-square test for categorical variables. A linear regression analysis was performed for correlation between weight loss and comorbidities before surgery and at the follow-up time. P < 0.05 was considered statistically significant, and 95% confidence interval (95% CI) was reported as a measure of precision.
Results
We identified 92 patients who underwent LAGB at our institution during the defined study period, of which 74 (80%) met the inclusion criteria. Most patients were female, 54 (72.9%), and the mean age at the time LAGB placement was 50.5 ± 9.6 years. The mean weight and mean BMI at the time of LAGB placement was 126.6 ± 16.8 kg and 45.5 ± 4.8 kg/m2, respectively. The prevalence of DM was 13.5%, HTN 32.0%, HPL 12.1%, OSA 5.4%, JD 10.8%, MD 5.4%, and GERD symptoms 8.1% (Table 1). All procedures were performed laparoscopically.
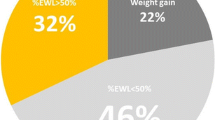
The long-term outcomes of LAGB in the study group are presented in Table 2. The average follow-up time was 162.96 ± 13.9 months (range 139.13–192.56 months). The %TWL 1 year after LAGB was 28.0 ± 0.16 and 21.0 ± 0.13 at the long-term follow-up. The mean BMI dropped from 45.5 ± 4.8 to 35.7 ± 6.9 kg/m2 (p < 0.001). The %EWL average was 31.7 ± 21.0%. There was not a statistically significant improvement in any of the preoperative comorbidities at the time of the long-term follow-up. Furthermore, GERD symptoms had significantly worsened from 6 (8.1%) to 29 (39.1%), p < 0.001.
The band was ultimately removed in 44 (59.4%) patients. Table 3 shows the indication for band extraction. The most common cause was technical failure of the band (40.9% from extracted bands, 24.3% from the entire cohort), followed by band intolerance (29.5, 17.5%), erosion or penetration (22.7, 13.5%), and slippage (6.8, 4.0%). The average time to band extraction was 63.3 ± 43.5 months. Among the patients who had their band removed, 22 (50.0%) patients underwent revision to another bariatric surgery. Table 4 details the bariatric procedures that were performed in these patients. Most of the revisions were to SG (n = 18, 81.8%) followed by RYGB (n = 2, 9.0%), biliopancreatic diversion (BPD) or Scopinaro procedure, and band replacement were performed in one patient each (n = 1, 4.5%). In six patients (27.2%), the bariatric revision was performed at the time of gastric band removal. All patients who underwent a simultaneous bariatric procedure underwent SG.
In an attempt to identify a correlation between clinical factors and weight lost following LAGB, we conducted a multivariate analysis (Table 5). The only significant factor that was positively associated to weight loss at the follow-up time was a revision of the band to another bariatric surgery (OR 12.8; CI 95% 1.62–23.9; p = 0.02).
Discussion
The introduction of laparoscopic gastric banding in 1993 has played a major role in the development of bariatric surgery. As a procedure performed using a minimally invasive technique, it has encouraged both patients and physicians to consider surgery as a valid option in the management of morbid obesity. The enthusiasm for LAGB was supported by the early results of this procedure, including low morbidity, almost no mortality, and weight loss that was comparable to purely restrictive procedures [14, 15]. Nevertheless, studies detailing the long-term outcomes following LAGB have produced contradictory results. While these papers report follow-up at a mean of 5 years or less post-procedure, our study is able to determine the true-long-term results following LAGB. With a minimum follow-up of 11.5 years, we have found that weight loss and comorbidity resolution is not durable over the long term following LAGB placement.
Our data show a relatively poor weight loss outcome with an average %EWL of 31.7%. Other long-term follow-up studies also reports unfavorable results in regard to resolution of comorbidities and weight loss [11, 12, 16,17,18]. Resolution of comorbidities following LAGB is often seen in the first 2 years after surgery. This improvement however is not maintained over the long term [9, 16]. In our study, we observed a significant worsening in GERD symptoms. This is explained by the fact that LAGB by its nature worsen reflux and even forms de novo in patients who previously were asymptomatic [16, 19]. GERD can also induce dietary incompliance and decrease weight loss after LAGB [18].
Band extraction was indicated in 59.4% of our patient’s population. We had quite a higher rate of technical problems (40.9%) in this group, which included tube and port displacement or infection. Compared to other studies, this kind of complication was usually reported as less than 10% [11, 17]. Furthermore, this observation contrasts the most commonly reported indication for band extraction in the literature. The most commonly reported indication for band extraction has been band migration or slippage causing pouch dilatation and symptoms of GERD and dysphasia. This difference in the indication for band removal might be due to the fact that band migration and slippage is more commonly associated with the perigastric technique [20]. Since all our cases were performed with the pars flaccida technique, we have seen less of migration complications.
At the end of our follow-up period, we basically had three groups: those who remained with the band throughout the entire follow-up, those who had their band removed only, and those who had their band removed with a revision to another bariatric procedure. Suter et al. [9] showed a rate of band removal of only 21.7% at about 8 years of follow-up, but they also stated that each further year of follow-up added 3–4% of major complications leading to band removal. O’Brien et al. [8] published long-term results up to 16 years in a cohort of 3227 patients with only 5.6% of bands removed. A thorough analysis of data, however, shows that 46% of patients at 10-year and 76% of patients at 15-year follow-up underwent surgical revision with replacement of the band.
We found that patients who had their band removed along with another bariatric procedure were almost 13 times more likely to achieve a greater weight loss compare to the other two groups mentioned. This finding is supported by a recent study by Himpens et al. who also report a favorable results of RYGB after failed LAGB that reached %EWL of 64% in a long-term follow-up compared with the 48% observed when the band was still in place [17]. Furthermore, Suter et al. and Aarts et al. showed that only one from five patients will benefit from LAGB in the long-term [9, 16].
Despite our results, this study has several limitations, which are worth mentioning. First, this is a retrospective study with a small sample size of patients. Furthermore, this study is not based on intent-to-treat but rather on long-term follow-up. This creates the potential for selection bias. Furthermore, we did not compare our group of patients to a control group of patients who had primary SG and RYGB. Rather, we performed a regression analysis to help identify factors that could contribute to the outcome measures, which we hope has sufficiently controlled for any confounding factors. Finally, while we were able to make comparisons between our three groups of patients, we recognize that there may be some surgeon influence into the patients that go on to undergo revision from LAGB to SG or RYGB.
Conclusions
Our long-term retrospective analysis of LAGB shows a high rate of band complications that progressed to band extraction in the majority of patients. Our data also demonstrates poor resolution of comorbidities and aggravation of GERD symptoms over the years. For patients currently with a band in place, band extraction and performance of another bariatric procedure may improve weigh loss outcome in this patient population.
Change history
01 December 2017
In the original article the spelling of author Naama Kafri was incorrect.
References
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–37.
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes—3-year outcomes. N Engl J Med. 2014;370(21):2002–13.
ASMBS web site; Estimate of bariatric surgery numbers, 2011–2015. https://asmbs.org/resources/estimate-of-bariatric-surgery-numbers [database on the Internet]. 2016.
Mognol P, Chosidow D, Marmuse JP. Laparoscopic gastric bypass versus laparoscopic adjustable gastric banding in the super-obese: a comparative study of 290 patients. Obes Surg. 2005;15(1):76–81.
Smoot TM, Xu P, Hilsenrath P, et al. Gastric bypass surgery in the United States, 1998-2002. Am J Public Health. 2006;96(7):1187–9.
Poulose BK, Griffin MR, Zhu Y, et al. National analysis of adverse patient safety for events in bariatric surgery. Am Surg. 2005;71(5):406–13.
Toolabi K, Golzarand M, Farid R. Laparoscopic adjustable gastric banding: efficacy and consequences over a 13-year period. Am J Surg. 2016;212(1):62–8.
O'Brien PE, MacDonald L, Anderson M, et al. Long-term outcomes after bariatric surgery: fifteen-year follow-up of adjustable gastric banding and a systematic review of the bariatric surgical literature. Ann Surg. 2013;257(1):87–94.
Suter M, Calmes JM, Paroz A, et al. A 10-year experience with laparoscopic gastric banding for morbid obesity: high long-term complication and failure rates. Obes Surg. 2006;16(7):829–35.
Arapis K, Tammaro P, Parenti LR, et al. Long-term results after laparoscopic adjustable gastric banding for morbid obesity: 18-year follow-up in a single university unit. Obes Surg. 2017;27(3):630–40.
Carandina S, Tabbara M, Galiay L, et al. Long-term outcomes of the laparoscopic adjustable gastric banding: weight loss and removal rate. A single center experience on 301 patients with a minimum follow-up of 10 years. Obes Surg. 2017;27(4):889–95.
Vinzens F, Kilchenmann A, Zumstein V, et al. Long-term outcome of laparoscopic adjustable gastric banding (LAGB): results of a Swiss single-center study of 405 patients with up to 18 years' follow-up. Surg Obes Relat Dis. 2017;
Brethauer SA, Kim J, el Chaar M, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Surg Obes Relat Dis. 2015;11(3):489–506.
Belachew M, Zimmermann JM. Evolution of a paradigm for laparoscopic adjustable gastric banding. Am J Surg. 2002;184(6B):21S–5S.
Favretti F, Segato G, Ashton D, et al. Laparoscopic adjustable gastric banding in 1,791 consecutive obese patients: 12-year results. Obes Surg. 2007;17(2):168–75.
Aarts EO, Dogan K, Koehestanie P, et al. Long-term results after laparoscopic adjustable gastric banding: a mean fourteen year follow-up study. Surg Obes Relat Dis. 2014;10(4):633–40.
Himpens J, Cadiere GB, Bazi M, et al. Long-term outcomes of laparoscopic adjustable gastric banding. Arch Surg. 2011;146(7):802–7.
Kowalewski PK, Olszewski R, Kwiatkowski A, et al. Life with a gastric band. Long-term outcomes of laparoscopic adjustable gastric banding—a retrospective study. Obes Surg. 2016;
Naik RD, Choksi YA, Vaezi MF. Impact of weight loss surgery on esophageal physiology. Gastroenterol Hepatol (N Y). 2015;11(12):801–9.
Singhal R, Bryant C, Kitchen M, et al. Band slippage and erosion after laparoscopic gastric banding: a meta-analysis. Surg Endosc. 2010;24(12):2980–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
We declare that all the information that was collected in this study was in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of Interest
All authors declare that they have no conflict of interest.
Informed Consent
Informed consent was obtained from all individual participants included in the study who were asked to respond to a telephone questionnaire.
Rights and permissions
About this article
Cite this article
Froylich, D., Abramovich-Segal, T., Pascal, G. et al. Long-Term (over 10 Years) Retrospective Follow-up of Laparoscopic Adjustable Gastric Banding. OBES SURG 28, 976–980 (2018). https://doi.org/10.1007/s11695-017-2952-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-2952-7