Abstract
Early and clear recovery from anesthesia is the crux for preventing perioperative complications in the obese undergoing bariatric surgery. Volatile inhalation agents by virtue of high lipid solubility are expected to produce residual anesthetic effects. Prospective randomized trials comparing desflurane and sevoflurane used for anesthesia maintenance (electroencephalograph guided) during bariatric surgery published till 1st of July 2017 were searched in the medical database. Comparisons were made for surrogate markers of recovery from anesthesia that included time to eye-opening (TEo), time to tracheal-extubation (TEx), and Aldrete scores on immediately shifting to recovery (Ald-I). Five trials were included in the final analysis. Patients receiving desflurane began to respond faster by opening eyes on command (five trials) by 3.80 min (95%CI being 1.83–5.76) (random effects, P < 0.01, I2 = 78.61%), and tracheal extubation was also performed earlier (four trials) by 4.97 min (95%CI being 1.34–8.59). This meant a reduction of 37% in TEo and 33.60% in TEx over sevoflurane. Ald-I scores were higher/better with desflurane by 0.52 (95%CI being 0.19–0.84) (Fixed-effects, P < 0.01, I2 = 6.67%). Publication bias is likely for TEo (Egger’s Test, X-intercept = − 8.57, P = 0.02). No airway-related complications were reported with desflurane’s expedited recovery. Use of desflurane compared to sevoflurane for maintenance of anesthesia in morbidly obese patients allows attaining verbal contact faster, and tracheal extubating can be performed earlier without compromising safety. The benefits of better recovery extend into the immediate postoperative phase with patients being more awake upon shifting to the recovery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Anesthesia for bariatric surgery and obese patients poses many unique challenges for the anesthesiologist. The perioperative plan needs to be tailored with utmost care to avoid anesthesia-related complications. A well-established fact that can help avoid airway and pulmonary complications in obese is to have the patient as awake as possible in the operating room prior to tracheal extubation [1]. Although one cannot directly control the wearing off of the anesthetic effects. the type of drugs used are the prime modifiable factors that have attracted significant research. Avoiding opioids or using short-acting opioids along with adjuvants has already shown to improve outcomes by decreasing residual effects of anesthesia exposure [2, 3]. Research has also established that avoiding or minimizing the need of neuromuscular blocking agents can directly cut down the number of postoperative pulmonary complications in obese [4] The relatively less explored yet potential modifiable factor is the type of maintenance anesthetic used. Emergence profile comparisons have been made between total intravenous anesthesia (TIVA) and gas-based general anesthesia. No clear superiority of one over the other (gas vs TIVA) has been established, rather the expertise of the anesthesiologist in using these techniques seems to guide emergence profile more strongly [5, 6]. Further, the search for the best anesthetic vapor during gas anesthesia has eluded many researchers. Although many clinical studies have tried to address this, results for obese patients are not entirely clear.
Intuitively based solely upon the blood gas partition coefficients, one may be inclined to choose desflurane as the best agent. This however may not be appropriate especially in obese patients considering the role of oil/gas partition coefficient in residual effects of anesthesia. Desflurane’s blood gas coefficient being 0.42 to 0.57 (lowest) might seem like a clear winner [7]. However, in obese patients, increased body fat percentage could play a vital role in prolonging the residual effects of anesthesia. So, what may be true in the lean population cannot be extrapolated to the obese population without strong clinical evidence. In this meta-analysis, we consolidate and evaluate the evidence comparing the two preferred anesthetic vapors (desflurane versus sevoflurane) used in obese patients. We attempt to compare and quantify the benefits (if any) during the immediate recovery phase from anesthesia for obese patients undergoing bariatric surgery.
Objective
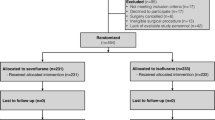
Our aim was to perform this meta-analysis in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) scheme (Fig. 1) and The Cochrane handbook for systematic reviews of interventions [8, 9]. Our primary aim was to compare desflurane with sevoflurane used during maintenance of anesthesia in obese patients. Both these agents were compared in terms of immediate post-anesthesia recovery profiles. The parameters documented consistently across trials were planned to be pooled together and used to quantify recovery efficiency.
Methods
The systematic review was conducted based upon the recommendations of The Cochrane Collaboration.
For identification of the potential studies that could be included in our analysis, we used the PICOS (Population, Intervention, control and outcome study) design. After literature search, trials were abstracted into a standardized PICOS format and relevance to our present study question was assessed by two independent reviewers.
Published trials were evaluated in the perspective of the three dimensions of possible risks of errors: design errors (that could lead to systematic errors indirectly via errors in outcomes, comparators, etc.), bias or systematic error, and random errors (“the play of chance” in the reported outcomes). These evaluations were also performed based upon the directions of The Cochrane collaboration [10, 11].
Eligibility Criterion
Randomized controlled trials involving adult patients (age > 18 years) with body mass index > 35 kg/m2 comparing the use of desflurane to sevoflurane for anesthesia maintenance during bariatric surgery were included. Trials that made comparisons with TIVA or any other anesthetic volatile agent were excluded. Studies were also excluded if they did not report immediate recovery-related outcomes [12, 13]. There were no restrictions on the nature of the bariatric procedure being performed during the study. We did not place any limitation on trials being included based upon the language they were published in. We also planned to include conference abstracts and research letters if they met the above criterion and were peer reviewed prior to publication. The following study types were planned to be excluded: quasi-randomized trials, observational trials, cross-over trials, and studies comparing non-bariatric procedures. The trial evaluating inhalation agents in obese use electroencephalogram (EEG) or clinical criterion-based titration of anesthesia; we restricted ourselves to trials using objective titration of anesthetic depth. We planned to exclude trials maintaining anesthesia based solely upon clinical criteria to avoid performance bias across studies.
Search Strategy
We searched the Cochrane Central Register of Controlled Trials (CENTRAL) in the Cochrane library, Embase, PubMed/Medline, Cinahl, Google Scholar, and Web of Science. The reference lists of the included trials and systematic reviews were manually searched for possible trials missed by electronic search. We also explored for ongoing trials on the topic of interest on the following websites: www.controlled-trials.com, www.centerwatch.com and www.clincaltrials.gov. We placed no restrictions on the time of publication and included all published trials until the 30th of June 2017. The following medical subject heading (MeSH) terms were searched for in the above said database: sevoflurane Vs desflurane, bariatric surgery, wakeup time, time to extubation, recovery profile inhalation agents, Aldrete score bariatric surgery. We excluded the following terms from the search string: isoflurane, general surgery, hemodynamic comparison, TIVA.
Study Selection and Data Extraction
Two authors independently reviewed all the identified titles and abstracts. Initial screening was done by them to exclude clearly irrelevant search hits. The decision to include a trial into final analysis was based upon the independent assessment of these two independent authors. Any disagreements between the two were harmonized by consensus and arbitration by a third neutral author.
Data were extracted from the full-text article of each included study, using a standardized data-extraction form prepared in Microsoft Excel (Microsoft inc, USA). The following data was extracted from each of the included trial—year and country of publication, study design, patient demographic profile, inhalation agent used during anesthesia maintenance, type of bariatric surgery, method used to titrate anesthesia depth, amount of opioid and neuromuscular blocker consumed (wherever reported), time to eye opening after surgery, time to tracheal extubation, Aldrete scores (upon shifting and at various time intervals in the recovery), post-anesthesia care unit (PACU) stay, and specific immediate adverse events directly related to anesthesia. We attempted to extract frequency data of individual complications for detailed analysis; however, reporting was very inconsistent among trials with most trials just grouping complications and thus an analysis was not possible. If in any study the relevant data was found to be missing, attempts were made to contact the corresponding author via e-mail for the required data. In the studies, if data of interest was expressed in terms of median and interquartile range, authors were contacted for the mean and SD values. In case no response was obtained, we estimated the mean and standard deviation using the validated Hozo’s formula [14, 15]. In few of the studies, if variance associated with means for some variables were not available, authors were contacted for the same. If no response was received, we imputed these variances as per Cochrane collaboration recommendations using mean from available variances from other included studies [16, 17].
Outcomes
Primary outcome was the analysis of recovery profile immediately after weaning off from anesthesia. The parameters that were consistently documented across trials were as follows:
-
1.
Time to eye opening—This was defined in all the studies as the time duration between switching off of the anesthetic vapor and patient’s opening of eyes on verbal command
-
2.
Time to extubation of trachea—This was defined in the included studies as the time duration between switching off the anesthetic vapor and extubation of the trachea, once the anesthesiologist was satisfied with the recovery and was confident that the patient would be able to maintain the airway unassisted.
As an explorative objective, we were able to meaningfully analyze/compare mean Aldrete scores in patients shifted to recovery upon immediate arrival. All trials that reported the patient recovery state in the recovery room used Aldrete score to report the same. For reader’s reference, it is provided as the supplementary Table 1. We also attempted to pool the results for Aldrete score at 10 min and immediately prior to discharge from recovery. However, only two studies reported these variables and pooling less than three groups is statistically not very useful. For the same reason, our attempts to pool values for total length of hospital stay and PACU stay were not successful.
Risk of Bias Assessment
All publications found during the search were manually and independently reviewed by two independent reviewers. Criteria that were used for assessing the risk of bias were based upon the recommendations of the Cochrane Collaboration [18] and included method of randomization; concealed treatment allocation; blinding during pre-, peri-, and postoperative care; blinded data collection and analysis; blinded adjudication of study endpoints; and completeness of data. The graphical synopsis of the above assessment was constructed using the software Review Manager 5 (Cochrane Collaboration).
Studies were also assessed for a possible publication bias initially using a funnel plot and later quantified using the Egger’s test.
Statistical Analysis
The statistical analysis of the pooled data was performed using Comprehensive Meta-analysis-Version 3 (Biostat Inc., USA). Meta-analysis was performed using fixed-effect modeling and subsequently random-effect modeling if heterogeneity was found to be higher than > 40%. Heterogeneity among trials was explored using the Chi-squared test with significance set at P value of 0.10. The heterogeneity was quantified using the inconsistency factor “I2.” Values of I2 < 40% were considered non-significant, 40–60% were considered to represent moderate heterogeneity, and 60–90% was reported as high heterogeneity. Wherever, heterogeneity was found to be higher than 40% and results from random-effect modeling were reported. Results were expressed as pooled means/pooled mean difference for continuous variables with 95% CI. P value of less than 0.05 was considered statistically significant.
Results
During our preliminary search, we found 128 studies matching our search criterion in the above-said database. The search results from independent authors were combined, and duplicates were removed automatically using Endnote (Thompson Reuters, USA). During our search, we did not find any non-English trials suitable meeting our search criterion. No conference/proceeding abstract or research letter was found to match the inclusion criterion. The study by Arain et al. [19] did include some bariatric procedures, but the authors included any abdominal surgery that lasted for more than 2 h. Thus, due to other abdominal surgeries also being included in their data, we excluded this study from our analysis. Trials by Ozdogan et al. [13] and De Baerdemaeker [12] compared desflurane and sevoflurane in morbidly obese patients undergoing bariatric surgery but did not report any parameter relevant to immediate recovery profile and thus had to be excluded from our analysis.
We could include five trials in our pooled analysis of the primary parameters. All the included trials titrated the intraoperative anesthetic agents based upon an EEG parameter. Four of these five trials used Bispectral (BIS) index to adjust inhalation anesthetic concentration and one use Patient State Index (PSI) for the same (Table 1). Time to eye opening was reported by all the five trials and time to tracheal extubation was reported in four trials. Three trials reported the Aldrete scores immediately on arrival in recovery and thus we could generate pooled results for this parameter as an exploratory objective.
The results were analyzed under the following subheadings:
-
1.
Time to eye opening
All the available times from the study were converted and reported in “minutes.” Values were available from five trials that included 118 and 114 patients in desflurane and sevoflurane groups, respectively. The pooled mean duration of time to eye opening was shorter in desflurane group by 3.80 min (95% CI being 1.83 to 5.76) (P < 0.01). The heterogeneity for the above pooled comparison was 78.61% (Fig. 2). The pooled mean eye-opening time with desflurane was 6.04 min and that with sevoflurane was 10.26. The use of desflurane lowered the eye-opening time by nearly 37%.
We performed a sensitivity analysis to explore for the high heterogeneity in the above pooled result. Using the “single study removal sensitivity analysis,” we found that almost all studies contributed equally to the reported heterogeneity. The study by Strum et al. had the highest contribution (9.42%) in the heterogeneity, and all other studies had contribution that varied between 6 and 8%.
-
2.
Time to tracheal extubation
Reported duration in all the trials was converted into minutes. Four trials included 98 and 94 patients in the desflurane and sevoflurane group, respectively. The pooled mean tracheal extubation time in desflurane was 9.32 min and that in sevoflurane group was 14.80 min. Patients who got desflurane as the maintenance anesthetic had tracheal extubation time lowered by 4.97 min (95% being 1.34 to 8.59) (P = 0.01). This meant a reduction of 33.60%. The heterogeneity for the above comparison was 92.64% (Fig. 3).
For the exploration of heterogeneity, the sensitivity analysis with single study removal method showed that the trial by La Colla et al. contributed the most to heterogeneity. Its removal led to drop in heterogeneity to 78.22% without significant alteration in the net effect size variable.
-
3.
Aldrete score immediately on shifting to the PACU
Three trials reported the values on immediate shifting to the PACU that included 79 patients in desflurane groups and 75 patients in sevoflurane group. Patients in the desflurane group had better recovery with pooled mean Aldrete scores being higher by 0.52 (95% CI being 0.19 to 0.84) units, P < 0.01. (Fig. 4) This pooled result had heterogeneity of 6.67%.
Assessment of Publication Bias
Publication bias was evaluated for the primary variables. The possibility of publication bias in time to eye opening was likely. Funnel plot for this variable is shown in Fig. 5. Egger’s regression test showed an X-axis intercept at − 8.57 with P value (two-tailed) being 0.017. The publication bias in “time to tracheal extubation variable” was unlikely as Egger’s regression test showed a value of intercept on X-axis at − 8.39 with a P value (two-tailed) of 0.11.
Study Quality Assessment
Quality assessment for bias in the included studies was carried out as per other published meta-analysis and the guidelines laid by the Cochrane Collaboration. These results are shown in Fig. 6. We used Revman version 5 (Cochrane Collaboration) for this evaluation and image generation.
Discussion
Our results have many direct and indirect clinical consequences. Desflurane clearly demonstrated a decrease in the eye-opening time that indirectly points towards the patient’s ability to comprehend verbal commands and to react to them. All anesthesiologists would agree that an awake patient is much less prone to have acute airway-related complications. This is even truer for bariatric patients where airway collapse is the most dreaded complication resulting from obesity-related anatomical alterations. The pooled 37% or 3.80-min reduction in our results might seem small at first glance. The benefit this reduction however extends beyond patient safety alone. Saving of operating room time for each bariatric patient can have lasting effect on hospital economy. It is estimated that each minute of operating room is billed at around US$62 [20]. Considering this, the yearly number of bariatric procedures totals to around 500,000 across the globe [21]. The cumulative savings originating out of this single parameter even without considering other parameters we analyzed would amount be enormous.
Time to tracheal extubation also showed a similar decrease with the use of desflurane. This further substantiates the ability of desflurane to allow expedited recovery. A similar trend was reported by meta-analysis in non-obese patients by Macario et al. [22]. It is however interesting to note that the expected benefits with the use of desflurane are much more pronounced in the obese. As per the Macario’s meta-analysis, the mean patient responsiveness time was better by 1.7 min and the tracheal extubation could be performed 1.3 min earlier in patients receiving desflurane. Our corresponding values in obese were found to be 3.80 and 4.97 min, respectively. This makes an even stronger point to use desflurane especially in the obese. The above results are also in coherence with the expectations based upon oil gas solubility coefficient of the volatile anesthetics. Obese patients have higher body fat percentage and are likely to show more marked difference among anesthetic agents with different fat solubility coefficients. Our meta-analysis helps to provide clinical evidence for this intuitive hypothesis.
One of the most promising results of our analysis is the finding that immediate Aldrete scores in the PACU were higher in the desflurane group. This further demonstrates the ability of desflurane-based anesthesia to wear off faster than other volatile anesthetics. In obese, the incidence of postoperative atelectasis, pneumonia, and aspiration is already higher than the lean counterpart [4, 23]. Presence of residual anesthetic effects can increase these complications, predisposing to higher perioperative morbidity [24]. A partially sedated obese patient can develop airway obstruction or can have worsening of obstructive sleep apnea (OSA) [25]. In a recent trial, Wani et al. concluded that the higher the Aldrete score immediately after endoscopy, the lower was the postoperative complication rate in obese patients [26]. We planned to analyze serial Aldrete scores during the first 6 h of PACU stay. Although individual trials did demonstrate benefit with desflurane as the Aldrete scores continued to remain higher, a mathematical pooling was not possible due to the insufficient number of trials reporting this variable. Vallejo et al. found that Aldrete scores reassessed at 10 min and at the time of discharge from PACU continues to be slightly higher with desflurane [27]. In the light of the above findings, it is prudent that future clinical trials would be able to demonstrate sustained benefit with the use of desflurane (at least during the early PACU stay). Other benefits reported by isolated trials in obese patients undergoing desflurane-based anesthesia include faster and better recovery of muscle strength (hand grip) [28], shorter hospital length of stay [29], and lower hemodynamic variation and better pulmonary function profile. [12]
Limitations
Our analysis had many limitations. The heterogeneity across the pooled primary variables was high. We attempt to explore this based upon sensitivity analysis yet it continued to remain high. This is most likely related to the individual methodological variations across the studies. Further, the variety of bariatric procedures included could have added to the high heterogeneity. We planned to perform a meta-regression stratifying based upon the nature of bariatric procedure, but with the small number of studies meeting the inclusion criterion, this was not feasible. We also attempted to compute and compare the total amount of opioids and neuromuscular blockers used during the intra-operative period. Unfortunately, included studies used predefined opioid infusions/regimen and poorly documented the total number of blouses used. Thus, we were not able to get accurate total opioid consumption during the study and pooling these values was not appropriate. None of the trials reported any airway-related complication with the use of desflurane or sevoflurane; thus, faster attempts to wean off anesthesia were equally safe in both the groups. As no study documented specific adverse events, an analysis (although planned) was not possible. Due to the small number of available studies, the possibility of a type I error cannot be completely negated. Time to eye-opening variable showed a possible publication bias; this can also be related to the small number of studies included in the analysis.
Conclusion
Use of desflurane compared to sevoflurane for maintenance of anesthesia in morbidly obese patients undergoing bariatric surgery allows the patients to attain verbal contact faster, and tracheal extubating can be performed earlier without compromising safety. The benefits of better recovery extend into the immediate postoperative phase with patients being more awake upon shifting to the recovery.
References
Singh PM, Panwar R, Borle A et al. Efficiency and safety effects of applying ERAS protocols to bariatric surgery: a systematic review with meta-analysis and trial sequential analysis of evidence. Obesity Surgery 2016; doi https://doi.org/10.1007/s11695-016-2442-3.
Thorell A, MacCormick AD, Awad S et al. Guidelines for perioperative care in bariatric surgery: enhanced recovery after surgery (ERAS) society recommendations. World J Surg 2016; doi https://doi.org/10.1007/s00268-016-3492-3.
Singh PM, Panwar R, Borle A, Mulier JP, Sinha A, Goudra B. Perioperative analgesic profile of dexmedetomidine infusions in morbidly obese undergoing bariatric surgery: a meta-analysis and trial sequential analysis. Surgery for Obesity and Related Diseases: Official Journal of the American Society for Bariatric Surgery 2017; doi https://doi.org/10.1016/j.soard.2017.02.025.
Alvarez A, Goudra BG, Singh PM. Enhanced recovery after bariatric surgery. Curr Opin Anaesthesiol. 2017;30:133–9.
Sinha AC, Singh PM. Controversies in perioperative anesthetic management of the morbidly obese: I am a surgeon, why should I care? Obes Surg. 2015;25:879–87.
Salihoglu Z, Karaca S, Kose Y, et al. Total intravenous anesthesia versus single breath technique and anesthesia maintenance with sevoflurane for bariatric operations. Obes Surg. 2001;11:496–501.
Esper T, Wehner M, Meinecke C-D, et al. Blood/gas partition coefficients for isoflurane, sevoflurane, and desflurane in a clinically relevant patient population. Anesth Analg. 2015;120:45–50.
Higgins JP, Green S. Guide to the contents of a Cochrane protocol and review. In: Fellow JPHSSV, Director SGF, editors. Cochrane handbook for systematic reviews of interventions. Ltd: John Wiley & Sons; 2008. p. 51–79.
Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews. 2015;4:1.
Higgins JP, Altman DG. Assessing risk of bias in included studies. In: Fellow JPHSSV, Director SGF, editors. Cochrane handbook for systematic reviews of interventions. Ltd: John Wiley & Sons; 2008. p. 187–241.
Higgins JPT, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
De Baerdemaeker LEC, Jacobs S, Den Blauwen NMM, et al. Postoperative results after desflurane or sevoflurane combined with remifentanil in morbidly obese patients. Obes Surg. 2006;16:728–33.
Ozdogan HK, Cetinkunar S, Karateke F, et al. The effects of sevoflurane and desflurane on the hemodynamics and respiratory functions in laparoscopic sleeve gastrectomy. J Clin Anesth. 2016;35:441–5.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13.
Singh PM, Arora S, Borle A, et al. Evaluation of etomidate for seizure duration in electroconvulsive therapy: a systematic review and meta-analysis. The Journal of ECT. 2015;31:213–25.
Thiessen Philbrook H, Barrowman N, Garg AX. Imputing variance estimates do not alter the conclusions of a meta-analysis with continuous outcomes: a case study of changes in renal function after living kidney donation. J Clin Epidemiol. 2007;60:228–40.
Chowdhry AK, Dworkin RH, McDermott MP. Meta-analysis with missing study-level sample variance data. Stat Med. 2016;35:3021–32.
Lundh A, Gøtzsche PC. Recommendations by Cochrane review groups for assessment of the risk of bias in studies. BMC Med Res Methodol. 2008;8:1–9.
Arain SR, Barth CD, Shankar H, et al. Choice of volatile anesthetic for the morbidly obese patient: sevoflurane or desflurane. J Clin Anesth. 2005;17:413–9.
Macario A. What does one minute of operating room time cost? J Clin Anesth. 2010;22:233–6.
de Raaff CAL, Gorter-Stam MAW, de Vries N et al. Perioperative management of obstructive sleep apnea in bariatric surgery: a consensus guideline. Surg Obes Relat Dis: Off J Am Soc Bariatric Surg 2017; doi https://doi.org/10.1016/j.soard.2017.03.022.
Macario A, Dexter F, Lubarsky D. Meta-analysis of trials comparing postoperative recovery after anesthesia with sevoflurane or desflurane. American Journal of health-system pharmacy: AJHP: Official Journal of the American Society of Health-System Pharmacists. 2005;62:63–8.
Singh PM, Borle A, Shah D et al. Optimizing prophylactic CPAP in patients without obstructive sleep apnoea for high-risk abdominal surgeries: a meta-regression analysis. Lung2016 Feb 19; doi https://doi.org/10.1007/s00408-016-9855-6.
Boucher BA, Witt WO, Foster TS. The postoperative adverse effects of inhalational anesthetics. Heart Lung: J Crit Care. 1986;15:63–9.
Wadhwa A, Singh PM, Sinha AC. Airway management in patients with morbid obesity. Int Anesthesiol Clin. 2013;51:26–40.
Wani S, Azar R, Hovis CE, et al. Obesity as a risk factor for sedation-related complications during propofol-mediated sedation for advanced endoscopic procedures. Gastrointest Endosc. 2011;74:1238–47.
Vallejo MC, Sah N, Phelps AL, et al. Desflurane versus sevoflurane for laparoscopic gastroplasty in morbidly obese patients. J Clin Anesth. 2007;19:3–8.
Kaur A, Jain AK, Sehgal R, et al. Hemodynamics and early recovery characteristics of desflurane versus sevoflurane in bariatric surgery. J Anaesthesiol Clin Pharmacol. 2013;29:36–40.
La Colla L, Albertin A, La Colla G, et al. Faster wash-out and recovery for desflurane vs sevoflurane in morbidly obese patients when no premedication is used. Br J Anaesth. 2007;99:353–8.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Statement of Human and Animal Rights
Not applicable.
Electronic supplementary material
ESM 1
Aldrete Scoring used in the studies to quantify recovery parameters. (DOCX 13 kb)
Rights and permissions
About this article
Cite this article
Singh, P.M., Borle, A., McGavin, J. et al. Comparison of the Recovery Profile between Desflurane and Sevoflurane in Patients Undergoing Bariatric Surgery—a Meta-Analysis of Randomized Controlled Trials. OBES SURG 27, 3031–3039 (2017). https://doi.org/10.1007/s11695-017-2929-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-2929-6