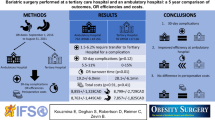
Abstract
Background
Bariatric surgery has become an increasingly popular method for weight loss and mitigation of co-morbidities in the obese population. Like any field, there is a desire to standardize and accelerate the postoperative period while maintaining safe outcomes.
Methods
All laparoscopic sleeve gastrectomies (LSG) and gastric bypasses (LGB) were performed over a 5-year period were logged along with several aspects of postoperative care. Trends were followed in aspects of postoperative care over years as well as any documentation of complications or re-admissions.
Results
A total of 545 LSGs and LBPs were performed between 2012 and 2016. Improvements were noted in nearly every field over time, including faster Foley removal, decreased length of hospital stay, decreased use of patient controlled analgesics (PCAs), and faster advancement of diet. There was also an abandonment of utilization of the ICU and step down setting for these patients, leading to significant decreases in hospital cost. There was no change in complications, re-operations, or re-admission in this time period.
Conclusions
The surgeons involved in this project have built a busy bariatric surgery practice, while continually evolving the postoperative algorithm. Nearly every aspect of postoperative care has been deescalated while decreasing length of stay and cost to the hospital. All of this has been obtained without incurring any increase in complications, re-operations, or re-admissions. The authors of this paper hope to use this article as a launching point for a formal advanced recovery pathway for bariatric surgery at their institution and others.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bariatric surgery has been demonstrated to provide significant weight loss and improvement in medical co-morbidities. This field involves complex procedures performed on patients with multiple co-morbidities, but when performed at high volume centers yield excellent results. With rising incidence of obesity and obesity-related diseases, recent attention has been paid to streamlining patient care to provide affordable and efficient care without compromising patient safety. Fast track protocols have been established in other areas of surgery for this reason, and recent literature has been aimed at demonstrating a fast track protocol for bariatric procedures. Laparoscopic sleeve gastrectomy (SG) and laparoscopic Roux-en-Y gastric bypass (LRYGB) are the most common procedures performed at this institution, with over 500 such procedures performed between 2012 and 2016. In this study, the authors analyze the evolution of the recovery protocol for patients undergoing bariatric surgery, evaluate patient outcomes in light of changing postoperative care, and identify possible areas for future improvement.
Materials and Methods
A retrospective chart review was performed at a community medical center. All patients that underwent SG or LRYGB between January 2012 and September 2016 with two bariatric surgeons were identified. The charts of these patients were then analyzed for length of hospital stay, postoperative floor and nursing ratio, pain control, Foley removal, advancement of diet, postoperative complications, and 30-day re-admission rate. Patient data was also recorded including age, sex, and BMI. The mean values for each of the above variables were recorded where applicable. Surgical complications were recorded in the immediate postoperative period and were scored according to the Clavien-Dindo classification of surgical complications [1]. Finally, the study population was divided into two groups: before and after May 1st 2015, when a dedicated surgical floor was opened in our institution.
Pre-operative Care
All patients are initially evaluated in bariatric clinic by one of the two bariatric surgeons. The patient’s eligibility for bariatric surgery is established using the guidelines published by the American Society for Metabolic and Bariatric Surgery, which use criteria of a BMI > 40 or a BMI > 35 with at least one obesity-related co-morbidity. When eligibility criteria are met, the patient attends information sessions where the procedures are described, and potential patients meet with patients that have already undergone the described procedure. The potential patients then undergo a pre-operative workup, which includes endoscopy, right upper quadrant ultrasound, medical and cardiac clearance (as indicated), and psychiatric screening. The patients also meet with a nutritionist as well as document their attempts at weight loss through diet and exercise. Once clearance is obtained, the patient proceeds to surgery. The bariatric center’s preoperative check list is included, as in Fig. 1.
Operative Technique
All bariatric procedures are assisted by residents at this institution. In the preoperative area, the patient is given 5000 units of heparin subcutaneously and sequential compression devices are placed to bilateral lower extremities. An anxiolytic is then given, and the patient is taken back to the operating room. A Foley catheter is placed after general anesthesia is placed.
The basic operative technique for the SG includes mobilization of the greater curvature of the stomach to the angle of His, mobilization and retraction medially of Belsey’s fat pad to expose the entirety of the fundus, and stapling beginning approximately 4 cm from the pylorus and concluding at the angle of His around a 36 French bougie. This usually requires 4–5 staple loads of a 60-mm stapler. In earlier portions of the study, the staple line was tested with air and methylene blue. These tests were no longer utilized in latter portions of the study.
Basic operative technique for LRYGB includes dividing the small bowel approximately 40 cm from the ligament of Treitz, creating a roughly 150 cm roux limb, creating a side-to-side anastomosis between the biliopancreatic and common limb, dividing the omentum, creating an anti-colic Roux limb, transecting the stomach roughly 7 cm from the gastroesophageal junction and creating the gastric pouch around a 32 French bougie, and performing an end-to-side hand-sewn anastomosis. The anastomosis is then tested with air and 60 cm3 of methylene blue delivered via orogastric tube. All patients with fatty infiltration of the liver on preoperative evaluation undergo liver biopsy to rule out non-alcoholic steatohepatitis.
At the conclusion of the procedure, in earlier portions of the study, patients had simple infiltration of local anesthetic in the port sites. In the latter portions of the study, patients now undergo bilateral rectus sheath block with Exparel. Additionally, patients would remain with Foley catheters earlier in the study, while in the latter portions of the study the Foley catheter is removed before the patient leaves the operating room.
Postoperative Care
After recovering in the PACU, the patient is transported to a surgical unit. As the years past, the patient was observed postoperatively in the surgical intensive care unit or step down unit, and more recently, patients have been observed on a dedicated surgical floor. Early ambulation and incentive spirometer use in encouraged immediately postoperatively. For pain control, in the earlier years of the study, patients were placed on patient-controlled analgesia (PCA) with either morphine or dilaudid. In more recent years of the study, patients are given as needed IV pushes of either dilaudid or morphine and are given exparel injection in the rectus sheath at time of surgery. The Foley catheter is now removed in the operating room, where during earlier portions of the study the catheter remained in place until the first postoperative day. Patients are kept strictly nil per os (NPO) until their first postoperative day, when an upper gastrointestinal series (UGI) is performed with gastrograffin. A test is considered negative if there is no extravasation of contrast. Patients are then started on 30 cm3 bariatric diet. Patients with delayed transit or edema are not delayed from starting their diet.
After the patient demonstrates ability to tolerate their initial 30 cm3 diet and water, their diet is advanced to a 90-cm3 meal. In the earlier portion of the study, patients received a 30-cm3 diet on the first postoperative day and were advanced to a 60- or 90-cm3 diet on the second postoperative day. In more recent years, patients have received their 90 cm3 meal at dinner time on the first postoperative day. Once tolerating a 90-cm3 diet and water in an amount adequate to remain hydrated, patients are eligible for discharge. Adequate hydration is based on clinical grounds such urine output and vital signs. Patients are seen for follow-up appointments at 1 week, 1 month, 3 months, 6 months, 1 year, and then annually for follow-up.
Results
Variables analyzed in this study included nursing ratio, length of hospital stay, Foley duration, modality of postoperative pain control, and advancement of diet. Outcomes measured included postoperative complications and 30-day re-admission rate.
The floor in which SGs were admitted to postoperatively is recorded in Table 1. Prior to May of 2015 when the surgical floor opened, no patient went to a floor with a nursing ratio of less than 3:1. Patients were either sent to ICU or a step down unit. After opening the surgical floor in 2015, which carries a nursing ratio of 5:1, 93% of patients with SG were cared for on the surgical floor. In 2016, 100% of these patients spent the hospital admission on the surgical floor.
Table 2 represents postoperative floor for LRYGB patients. Prior to May of 2015, no patients were admitted to a floor with a nursing ratio less than 3:1, with a majority of patients going to ICU. After the surgical floor opened in 2015, 78% of patients were admitted to the surgical floor, with 100% being admitted to the surgical floor in 2016.
Length of stay was also analyzed with a trend towards decreasing length of stay in more recent years. Table 3 represents the day of discharge for SG. For example, LOS of 3 days or less were 42.3% in 2012, compared to 93% in 2016. A similar trend was noted in LRYGB, as displayed in Table 4. Although there were only three bypass procedures performed in 2012, all three patients had a LOS over 3 days, while in 2016 93% of patients were discharged home in 3 days or less. For all procedures after the surgical unit was opened, 35.3% of patients were discharged on the first postoperative day, and 90.2% of patients were discharged by the second postoperative day. These rates were improved from earlier in the study when patients were observed in step down units, when 7.8% of patients were discharged on the first postoperative day, and 68.4% being discharged by the second postoperative day.
Timing for Foley catheter removal is represented in Tables 5 and 6 for SG and LRYGB, respectively. Practice early in the study was to leave the urinary catheter in overnight until the UGI was completed on the first postoperative day. As of 2016, 90% of SG and 93% of LRYGB patients had the urinary catheter removed prior to leaving the operating room. Of note, there were no catheter-associated urinary tract infections noted with any patient in this study.
Evolution in postoperative pain control is outlined in Tables 7 and 8. Overall, a significant transition from the use of PCA to the use of intermitted IV medications on the day of operation followed by use of oral pain medications after a normal UGI performed on the first postoperative day.
Tables 9 and 10 represent alterations in advancement of diet postoperatively. As noted in both patients undergoing SG and LRYGB, a stepwise progression from 30 cm3 to 60 cm3 to 90 cm3 per day has been abandoned in favor of progressing to 90 cm3 on the first postoperative day (Table 11).
Complications and Re-admissions
Complications that occurred in the immediate postoperative period were recorded in this study using the Clavien-Dindo classification for surgical complications. In the immediate postoperative period, there were 18 Grade I complications, 7 Grade II complications, and 1 Grade III complication. Examples of these complications are listed in Table 12, and the complications that occurred in this study are outlined in Table 13. Within 30 days, there were 20 re-admissions, for an overall re-admission rate of 3.6%. There were 16 patients re-admitted for dehydration or pain control for 24 h, 3 patients were re-admitted and diagnosed with DVT/PE. One patient was re-admitted with a fever and was diagnosed with a leak on upper GI series, which was controlled endoscopically.
When comparing postoperative complications between the time periods before and after the dedicated surgical unit opened, there were 4 (2.6%) grade I complications and 3 (2.0%) grade II complications after the surgical unit opened compared to 14 (3.5%) grade I complications and 4 (1.0%) grade II complications before it opened. Of the 20 patients that were re-admitted during the course of the study, only 6 were re-admitted in the latter portions of the study, after the surgical floor had been opened. This is a re-admission rate of one every 25.5 cases, compared with a re-admission rate of one every 28.5 cases in the earlier portion of the study.
Cost is an important topic when discussing hospital-based protocols. The authors analyzed cost between patients that were observed in ICU or step down units in earlier portions of the study to those observed on the surgical floor; after the study, average cost was calculated. Given the average length of stay of 2.25 days before opening the surgical unit, for room and board in a ICU and step down unit, the average cost was calculated to be $3462.75. Given an average length of stay of 1.79 days after the surgical unit opened, the average cost for room and board on the surgical unit is $778.65. These calculations are based on an average room and board cost of $435/day in the surgical unit and $1539/day in the ICU and step down units. This indicates significant cost savings with a decreased nursing ratio.
Chi square analysis was used to determine if shorter hospital stays in more recent periods of the study after the surgical floor opened resulted in an increase in complications. Grades 1 and 2 complications were pooled and analyzed. There was found to be no significant difference between earlier and later portions of the study in terms of complications (p = 0.674). These data indicate that a shorter hospital stay did not increase complication rates.
Discussion
Obesity and obesity-related diseases are a significant cause of morbidity in the USA. With the increasing prevalence of these diseases, bariatric surgery is utilized for the purpose of limiting morbidity and possibly curing patients of obesity-related illness. Compared with other non-surgical treatments, bariatric surgery offers more sustained weight loss and higher remission rates for medical co-morbidities like type 2 diabetes [2]. While the field of bariatric surgery has been demonstrated to be both cost effective and safe for the treatment of obesity, recent studies have aimed to identify enhanced recovery protocol for these patients. Previous studies have demonstrated effectiveness in cost, safety, and patient satisfaction of enhanced recovery protocols in other fields of surgery [3,4,5].
In this study, the evolution of the perioperative protocol for the care of the bariatric patient is outlined, including changes to the protocol over the years and their effects on patient outcomes as well as cost. What the authors have found in this study is a trend towards more cost-effective, efficient care without compromising patient safety.
The pre-operative evaluation is an important aspect of care of the bariatric patient. All patients meet initially in interest and support meetings to familiarize themselves with the procedures offered at this institution as well as what to expect following surgery. Patients then undergo medical clearance, right upper quadrant ultrasound, and upper endoscopy. The latter is important to determine the presence of Helicobacter pylori, ulcer disease, hiatal hernia, esophagitis, or gastritis, as the presence of any of these findings may alter the course of treatment [6, 7]. The presence or absence of hiatal hernia is important, as studies have demonstrated patients undergoing bariatric procedures with pre-existing reflux have been demonstrated to have improvement of their symptoms with concomitant hiatal hernia repair [8, 9].
When evaluating the nursing level of care delineated to patients after their operation, initial periods of the study saw patients being sent to ICU and step down units, with nursing ratios of 2–3:1. These were not dedicated surgical floors, and medical and surgical patients were mixed. Currently, nearly every patient goes to the dedicated surgical floor, where the nursing ratio is 5:1. This reflects an increasing level of comfort with the surgeons and nursing staff and has resulted in significant cost savings without compromising patient care.
Foley catheters are utilized intra-operatively to monitor and maintain fluid status. Laparoscopy in morbidly obese patients results in depressed cardiac function and decreased urinary output due to increased abdominal pressure compared to non-obese patients [10]. Therefore, Foley catheters are used to assess adequate volume. In initial portions of the study, the catheter remained for 24 h until the upper GI series was completed. This practice was abandoned in favor of removing the catheter at the end of the operative case. Having a Foley postoperatively was a hindrance to early ambulation and served as a possible nidus for infection. There were no reported urinary tract infections in any patients included in this study.
In terms of pain control, multimodal pain control with local infiltration of anesthetics at time of surgery has been demonstrated to be efficacious [11, 12]. In initial portions of the study, patients were maintained on PCA (patient controlled analgesia) machines with either morphine or dilaudid. If the upper GI series on the first postoperative day was normal, the PCA was discontinued in favor of oral Percocet, which would be the discharge pain regimen for the patient. In more recent periods of the study, Exparel (liposomal bupivocaine) has been used in the operating room, diluted to 60 cm3 with 20 cm3 injected into bilateral rectus sheaths and the remaining 40 cm3 locally infiltrated into port sites. Ofirmev has also been demonstrated to have a decrease in subjective pain [13] and has been included in the post operative pain control of patients in later portions of the study. These changes have resulted in a virtual abandonment in use of PCA machines, with morphine available for rescue pain control. Patients are then switched to oral pain medications and discharged with oral medications for breakthrough pain at home.
The next portion of the protocol has remained the same during all parts of the study, and that is the utilization of an upper GI series on postoperative day #1 to evaluate for a leak, as well as to obtain a baseline study for comparison to future studies if need be. Early postoperative upper gastrointestinal series was demonstrated in one study to identify radiographic leaks that would otherwise progress to clinically significant leaks, thereby minimizing the morbidity associated with the most feared complication after these surgeries [14]. There were no leaks identified on immediate postoperative upper gastrointestinal series in this study. The one patient that suffered a leak presented to the emergency department weeks after discharge with fever, tachycardia, and dyspnea. An upper gastrointestinal series that demonstrated delayed passage of contrast altered a patient’s postoperative course by delaying initiation of their diet.
In all portions of the study, after the upper gastrointestinal series is read as normal, the patient is initiated on a volume controlled diet, starting with 30 cm3 and advancing to 90 cm3 as tolerated. Home PO medications are then started as well as PO pain medications. This process tends to occur during the course of the first postoperative day. The patients are then discharged home when their pain is well controlled and tolerating enough PO to maintain adequate hydration. This process has become more streamlined with the opening of the dedicated surgical floor, resulting in faster time to discharge in the latter portions of the study.
Recent studies have aimed to evaluate the safety of early discharge after bariatric surgery and have used that information to establish standards for postoperative care. Elnahas et al. performed at retrospective cohort analysis of patients in the ACS-NSQIP registry and found that discharge on the first postoperative day for patients undergoing laparoscopic sleeve gastrectomy did not have a worse rate of 30-day adverse events compared to patients discharged on the second postoperative day [15]. Raftopoulos et al. evaluated the safety of 23 h hospital stay for patients that underwent LRYGB. In their study, nearly 72% of patients that underwent LRYGB were discharged within 24 h without an increase in 30-day morbidity, mortality, re-admission, or re-operation [16]. Interestingly, a recent study by Lois et al. demonstrated that not only was early discharge not associated with an increased rate of re-admission within 30 days, but that patients with longer hospital stays after bariatric surgery were more likely to be re-admitted [17].
Given this information for safe early discharge of the bariatric patient, several postoperative protocols have been proposed to expedite postoperative care. These studies have demonstrated that efficient postoperative care is feasible, cost-effective, and does not increase preoperative morbidity, mortality or re-admission [18,19,20]. Our study supports these results, as streamlining patient care at our institution has lead to shorter hospital stays without compromising patient care.
An area of our study that deserves critique is the use of the postoperative upper gastrointestinal series. A postoperative gastrograffin study was not utilized in any of the enhanced recovery studies referenced above. The surgeons in the present study utilize the test both to evaluate for leak or stricture and to serve as a comparison for future studies. However, it should be noted that there was not a single leak noted on these studies. One patient that had a leak presented to the hospital weeks after discharge with fevers. Delayed passage of contrast on upper GI was one of the parameters included in grade I complications, as it delayed the advancement of the patient’s diet. Recent studies evaluating the utility of a routine postoperative upper GI have found that these studies have limited utility in the postoperative setting and can lead to unnecessary intervention based on false positive results [21]. With this in mind, these studies recommend use of physiologic markers like tachycardia and respiratory distress to raise suspicion for a leak [22]. Given the recent published data regarding protocols without an upper gastrointestinal series as well as studies demonstrating their limited utility, an additional measure to streamline patient care postoperatively would be to eliminate this study.
This series is limited in that it is retrospective in nature and at a single institution. It does however display a large number of cases over 5 years and is controlled in the sense it is the same two surgeons performing all the operations.
Conclusion
This study examines the evolution of the postoperative protocol for patients undergoing LRYGB and SG at a bariatric surgical center of excellence over a 5-year period. In recent years and since opening a dedicated surgical floor, shorter hospital stays with higher nursing ratios have not led to an increase in postoperative complications or re-admissions. There have also been improvements in time to Foley removal, advancement of diet, and de-escalating of pain control. An additional measure to further streamline patient care would be to eliminate the upper GI series on the first postoperative day, leading to more timely discharge at lower cost to the patient without compromising patient care.
References
Dindo D, Demartines N, Clavien P. Classification of surgical complications. Ann Surg. 2004;240(2):205–13.
Gloy BL, Briel M, Bhatt DL, et al. Bariatric surgery versus non-surgical treatment for obesity: a systematic review and meta-analysis of randomized controlled trials. BMJ. 2013;347:f5934.
Miller TE, Thacker JK, White WD, et al. reduced length of hospital stay in colorectal surgery after implementation of an enhanced recovery protocol. Anesth Analg. 2014;118(5):1052–61.
Roulin D, Donadini A, Gander S, et al. Cost effectiveness of the implementation of an enhanced recovery protocol for colorectal surgery. BJS. 2013;100(8):1108–14.
Arumainayagam N, Mc Grath J, Jefferson KP, et al. Introduction of an enhanced recovery pathway for radical cystectomy. BJU. 2008;101(6):698–701.
Sharaf RN, Weinshel EH, Bini EJ, Rosenberg J, et al. Endoscopy plays an important role in bariatric surgery. Obes Surg. 2004;14(10):1367-72.
Madan AK, Speck KE, Hiler ML. Routine pre-operative upper endoscopy for laparoscopic gastric bypass: is it necessary? Am Surg. 2004;70(8):684–6.
Soricelli E, Iossa A, Casella G, et al. Sleeve gastrectomy and crural repair in obese patients with gastroesophageal reflux disease and/or hiatal hernia. Surg Obes Relat Dis. 2013;9(3):356–61.
Sucandy I, Chrestiana D, Bonanni F, et al. Gastroesophageal reflux symptoms after laparoscopic sleeve gastrectomy for morbid obesity. The importance of pre-operative evaluation and selection. North Am J Med Sci. 2015;7(5):189.
Nguyen NT, Wolfe BM. The physiologic effects of pneumoperitoneum in the morbidly obese. Ann Surg. 2005;241(2):219–26.
Lam KK, Mui WL. Multimodal analgesia model to achieve low postoperative opioid requirement following bariatric surgery. Hong Kong Med J. 2016;22(5):428–34.
Ruiz-Tovar J, Munoz JL, Gonzalez J, et al. Postoperative pain after laparoscopic sleeve gastrectomy: comparison of three analgesic schemes (isolated intravenous analgesia, epidural analgesia associated with intravenous analgesia and port-sites infiltration with bupivocaine associated with intravenous analgesia). Surg Endosc. 2017;31(1):231–6.
Strode MA, Sherman W, Mangieri CW, et al. randomized trial of OFIRMEV versus placebo for pain management after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2016;12(4):772–7.
Serafini F, Anderson W, Ghassemi P, et al. The utility of contrast studies and drains in the management of patients after roux En Y gastric bypass. Obes Surg. 2002;12(1):34–8.
Elnahas A, Okrainec A, Quereshy FA, et al. Safety of next day discharge following laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2015;11(3):525–9.
Raftopoulos I, Ginnakou A, Davidson E. Prospective 30-day outcome evaluation of a fast track-protocol for 23-hour ambulatory primary and revisional laparoscopic roux-en-Y gastric bypass in 820 consecutive unselected patients. J Am Coll Surg. 2016;222(6):1189–200.
Lois AW, Frelich MJ, Sahr NA, et al. The relationship between duration of stay and readmissions in patients undergoing bariatric surgery. Surgery. 2015;158(2):501–7.
Barreca M, Renzi C, Tankel J, et al. Is there a role for enhanced recovery after laparoscopic bariatric surgery? Preliminary results from a specialist obesity treatment center. Surg Obes Relat Dis. 2016;12(1):119–26.
Awad S, Carter S, Purkayastha S, et al. Enhanced recovery after bariatric surgery (ERABS): clinical outcomes from a tertiary referral bariatric centre. Obes Surg. 2014;24(5):753–8.
Simonelli V, Goergen M, Orlando GG, et al. Fast-track in bariatric and metabolic surgery: feasability and cost analysis through a matched-cohort study in a single Centre. Obes Surg. 2016;26(8):1970–7.
Doraiswamy A, Rasmussen JJ, Pierce J, et al. The utility of routine post-operative upper GI series following laparoscopic gastric bypass. Surg Endosc. 2007;21(12):2159–62.
Quartararo G, Facchiano E, Scaringi S, et al. Upper gastrointestinal series after Roux-en-Y gastric bypass for morbid obesity: effectiveness in leakage detection. A Systematic Review of the Literature. Obes Surg. 2014;24(7):1096–101.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
None of the authors have any financial disclosures or conflicts of interest to disclose.
Informed Consent
In retrospective study and for this type of study, formal consent from patients is not required.
Rights and permissions
About this article
Cite this article
Shea, B., Boyan, W., Botta, J. et al. Five Years, Two Surgeons, and over 500 Bariatric Procedures: What Have We Learned?. OBES SURG 27, 2742–2749 (2017). https://doi.org/10.1007/s11695-017-2873-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-2873-5