Abstract
Objective
Bariatric surgery has been shown to be the most effective method of achieving weight loss and alleviating obesity-related comorbidities. Yet, it is not being used equitably. This study seeks to identify if there is a disparity in payer status of patients undergoing bariatric surgery and what factors are associated with this disparity.
Methods
We performed a case-control analysis of National Inpatient Sample. We identified adults with body mass index (BMI) greater than or equal to 25 kg/m2 who underwent bariatric surgery and matched them with overweight inpatient adult controls not undergoing surgery. The sample was analyzed using multivariate logistic regression.
Results
We identified 132,342 cases, in which the majority had private insurance (72.8%). Bariatric patients were significantly more likely to be privately insured than any other payer status; Medicare- and Medicaid-covered patients accounted for a low percentage of cases (Medicare 5.1%, OR 0.33, 95% CI 0.29–0.37, p < 0.001; Medicaid 8.7%, OR 0.21, 95% CI 0.18–0.25, p < 0.001). Medicare (OR 1.54, 95% CI 1.33–1.78, p < 0.001) and Medicaid (OR 1.31, 95% CI 1.08–1.60, p = 0.007) patients undergoing bariatric surgery had an increased risk of complications compared to privately insured patients.
Conclusions
Publicly insured patients are significantly less likely to undergo bariatric surgery. As a group, these patients experience higher rates of obesity and related complications and thus are most in need of bariatric surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity in the USA has become one of the greatest public health epidemics, impacting and affecting all economic levels of society and leading to approximately 400,000 deaths per year, second only to smoking [1]. Since the 1960s, adult obesity rates have nearly tripled with approximately 35% of American adults considered obese and these rates are predicted to keep significantly increasing over the next 15 years [2, 3]. Studies have shown that the prevalence of morbid obesity, defined as a body mass index (BMI) ≥40 kg/m2, is, in fact, increasing even faster than other obesity classes and it is additionally predicted that the percentage of adults with a BMI >45 will double from 2.1% in 2004 to 4.4% by 2020 [4, 5]. This is a terrifying prospect for healthcare professionals and, more importantly, for patients as obesity and its associated comorbidities create medical challenges, complicated cases, and financial burdens. Obesity leads to cardiovascular disease, diabetes, dyslipidemia, osteoarthritis, obstructive sleep apnea, depression, malignancy, and gastroesophageal reflux disease, and the prevalence of these obesity-related comorbidities is found to be highest among those with morbid obesity [6]. Having a BMI >40 is furthermore shown to correlate with a significant reduction in the life span of 10 years, and a meta-analysis of 97 studies demonstrated that a BMI >35 is associated with significantly higher all-cause mortality [7, 8].
Obesity not only negatively impacts health but also is an economic phenomenon, creating direct and indirect costs that are more considerable than those for any other primary disease within today’s generation. The economic burden of obesity is well documented with substantial disparities in healthcare costs between moderate and severe obesity [9, 10]. And even though the obesity phenomenon is widespread and rather non-discerning, studies do show that a negative relationship exists between socioeconomic status and income with BMI, particularly among women [11,12,13,14].
With such widespread detrimental effects of obesity invading various aspects of society, it is intuitive to understand why bariatric surgery has exploded as an excellent surgical solution to this complicated epidemic. In the late 1990s, there were only 12,000 bariatric cases performed per year and now it is estimated there are over 100,000 cases performed per year [15]. Bariatric surgery has become the treatment of choice for patients with a BMI >40 or a BMI >35 with comorbidities [16]. It not only leads to significant decreases in risk factors and long-term, sustainable weight loss but also confers a survival advantage in surgical patients [17]. Additionally, with a return to lower BMI, a meta-analysis demonstrated that bariatric surgery is effective in financial models and leads to reductions in healthcare costs by improving quality of life and decreasing comorbidities [18].
Unfortunately, bariatric surgery is not an accessible or viable option for all patients even if deemed medically suitable and optimized for surgery. Many candidates are either delayed or denied undergoing this effective procedure secondary to a lack of insurance coverage. Studies show that these delays and insurance rejections lead to an astonishing statistically significant threefold increase in mortality [19]. Therefore, lower-socioeconomic patients not only are more inclined to be obese but also often have inadequate insurance coverage secondary to income that does not cover bariatric surgery. Thus, the patient with obesity continues to have increased healthcare costs associated with obesity, creating a self-sustaining cycle that negatively impacts not only the individual but also the country’s economy.
This study seeks to further illuminate whether a disparity in payer status exists in patients undergoing bariatric surgery and what factors are associated with such disparity such that we can ultimately improve upon healthcare reform to eliminate such inequities.
Methods
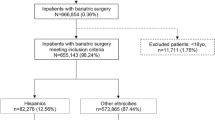
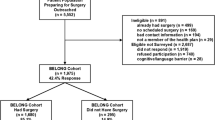
This study is a retrospective case-control study. The principle outcomes were to evaluate whether certain factors (i.e., payer status, demographics, and hospital attributes) are associated with bariatric surgery and/or outcomes of bariatric surgery. Data was derived from the Nationwide Inpatient Sample (NIS) database for the years 2003–2010. The Nationwide Inpatient Sample is part of the Healthcare Cost and Utilization Project (HCUP), sponsored by the Agency for Healthcare Research and Quality. This is the largest all-payer inpatient care database that is publicly available in the USA. It contains data from approximately eight million hospital stays from about 1000 hospitals sampled to approximate a 20% stratified sample of US community hospitals. The NIS database is a publicly available de-identified database that is exempt from the approval of the institutional review board [20]. The International Classification of Disease, 9th Revision (ICD-9) was used in defining the parameters of the study.
Cases included adult (≥18 years) inpatients with a BMI of more than or equal to 25 kg/m2 and those who underwent bariatric surgery. Controls were randomly selected with a ratio of 5 (controls):1 (case) from a patient with a BMI ≥25 kg/m2 and who did not undergo bariatric surgery.
Objectives
The primary objective was to examine if certain demographics, economic characteristics, and hospital attributes are associated with bariatric surgery. Factors of interest included (i) age (<35, 35–<65, and ≥65 years old), (ii) gender, (iii) race (White, Black, Hispanic, Asian/Pacific Islander, Native American, other), (iv) service payer (private, Medicare, Medicaid, self-pay), (v) modified Charlson Comorbidity Index Score (CCIS) (0, 1, and ≥24), (vi) hospital region (northeast, Midwest, west, south), (vii) hospital location (rural, urban), and (viii) hospital teaching status (non-teaching, teaching).
The secondary objective of the study was to assess factors associated with outcomes of bariatric surgeries. Those outcomes included (i) postoperative complications (none vs. one or more of cardiovascular, pulmonary, urinary, bleeding, infectious, and wound complications) and (ii) length of stay (LOS), categorized based on quartile classification into short stay (≤75th percentile, ≤3 days) vs. long stay (>75th percentile, >3 days).
Other independent factors considered for confounding effect included (i) surgeon volume, calculated based on the annual frequency of bariatric surgeries performed by each surgeons and then categorized based on quartile classification into low volume (≤25th percentile, ≤45 surgeries/year), intermediate volume (>25th–75th percentile, 46–174 surgeries/year), and high volume (>75th percentile, ≥175 surgeries/year), and (ii) hospital volume, calculated based on the annual frequency of bariatric surgeries performed in each hospital and then categorized based on quartile classification into low volume (≤25th percentile, ≤109 surgeries/year), intermediate volume (>25th–75th percentile, 110–374 surgeries/year), and high volume (>75th percentile, ≥375 surgeries/year).
Statistical Analysis
In our analysis, we used weighted data reflecting a national estimate. The records’ weights are available in the NIS data and calculated based on the stratification variables that were used in sampling methodology. These variables include hospital geographic region, urban/rural location, teaching status, bed size, and ownership. Cross-tabulation and chi-square tests were used to examine the association between each of the independent factors and the outcome of interest. Factors with significant association were considered possible confounders and were included in multivariate logistic regression models. Multivariate logistic regression models were used to calculate the odds ratio (OR) and 95% CI. A linear regression model was applied to determine incidence growth rate for 8 years beyond the study period. Significance level was set at an alpha of 0.05. All data analyses were performed using SAS 9.3 for Windows (SAS Institute, Inc., Cary, NC, USA).
Results
Study Population
We identified 132,342 patients in the NIS database who underwent bariatric surgery between 2003 and 2010 (Table 1). The average age of the study population was 53.6 years, and the majority was female (66.5%) and White (70.0%). Forty-two percent of the study population had private insurance, and the average LOS of bariatric surgery per case was 2.5 (±0.04) days.
Unadjusted Analysis
Bariatric patients were significantly more likely to be between 35 and 65, female, white, and privately insured than controls. They were also more likely to have no comorbidities. Cases were more likely to be in the northeast at an urban, teaching hospital. Private insurance accounted for 72.8% of payer status of bariatric patients, whereas Medicare and Medicaid only accounted for 10.6 and 6.7%, respectively. Self-pay covered only 4.9% of controls, while self-pay accounted for 6.5% of bariatric patients (Table 1).
Adjusted Analysis
After adjusting for age, race, Charlson Comorbidity Index Score, hospital region, location, and teaching status, bariatric patients were significantly more likely to be privately insured than any other payer status; Medicare- and Medicaid-covered patients accounted for a low percentage of cases (Medicare 5.1%, OR 0.33, 95% CI 0.29–0.37, p < 0.001; Medicaid 8.7%, OR 0.21, 95% CI 0.18–0.25, p < 0.001). Table 2 shows the multivariate model of characteristics of the bariatric surgery population compared to controls who did not undergo bariatric surgery. For post-bariatric surgical complications, using private insurance as the reference group, the odds ratio for a risk of complications is 1.54 in the Medicare group (95% CI 1.33–1.78, p < 0.001) and 1.31 in the Medicaid group (95% CI 1.08–1.60, p = 0.007). Self-pay status carries a decreased risk, with an odds ratio of 0.81 (95% CI 0.66–0.997, p = 0.047) compared to the privately insured reference group (Table 3).
There was not a significant association between payer status and in-hospital mortality, so payer status was not included in the multivariate model for the risk of in-hospital mortality. Similarly, there was no significant association of payer status with a risk of health services costing greater than the 75th percentile ($16,153.06).
When examining a multivariate model for the risk of extended hospital length of stay (>75th percentile, >3 days), Medicare and Medicaid again appear to be risk factors with odds ratios of 1.73 (95% CI 1.51–1.98, p < 0.001) and 2.29 (95% CI 1.92–2.73, p < 0.001), while self-pay patients have a decreased risk of extended hospital stay, with an odds ratio of 0.58 (95% CI 0.48–0.70, p < 0.001) (Table 4).
Discussion
In this case-control analysis of approximately 130,000 inpatients with obesity, we discovered that patients with Medicare or Medicaid were significantly less likely to undergo bariatric surgery than privately insured patients, suggesting that cost and access to care may be barriers to a lifesaving operation. Payer status affects surgical care; this is consistent with other current literature. Santry et al. showed similar results with the majority of bariatric patients being middle aged, white, female, and having private insurance [21]. Another study looked at the characteristics of the bariatric patient at both a private practice and an academic institution; 0% of patients at the private practice were federally funded whereas 28% were at the academic institution, which was statistically significant [22]. This disparity found in bariatric patients may be attributed to multiple mechanisms. First, the low payment generosity from public insurance has been found to be a significant component in physicians’ decisions to deny services to these patients [23,24,25,26]. Public insurance results in decreased payment to physicians and to hospitals, resulting in decreased reimbursements for both in comparison with private insurance [27]. Furthermore, publicly insured patients have on average longer lengths of stay and accrue significantly higher total hospital charges [28]. This could be secondary to the fact that public insurance covers the elderly and the disabled who have more comorbidities resulting in more complicated hospital stays. This study, however, did not find a significant difference between payer status and total hospital charges although the disparity in length of stay was replicated. Additionally, surgeons may take a patient’s socioeconomic status into consideration when evaluating for surgery to the detriment of the patient. Low socioeconomic status can become a barrier to a significant recovery secondary to a potential lack of transportation or inability to cover indirect costs necessary for care, resulting in a negative outcome. However, studies have shown this is not the case. Publicly funded patients did as well as the privately funded group in bariatric surgery, having on average the same amount of weight loss and similar reductions in medications for comorbidities and a similar percentage of patients in both groups were able to procure new employment postoperatively [29].
Our study also revealed that having Medicare or Medicaid insurance increased the risk of complications after bariatric surgery whereas self-pay insurance status decreased the risk of postoperative complications. Other retrospective analyses showed similar findings with publicly insured patients having more postoperative complications and increased morbidity and mortality in comparison to privately insured and self-pay patients [28]. This finding is not just demonstrated in bariatric surgery. LaPar et al. reviewed nearly 900,000 major surgical operatives including gastrointestinal cases, orthopedic cases, and cardiac cases using the NIS database and found that Medicaid and uninsured payer status bestows a significantly increased risk-adjusted mortality [30]. Other data has demonstrated that Medicaid patients receiving vascular surgery have more severe disease than matched privately insured patients and a higher adjusted mortality rate after trauma surgery [31, 32]. Medicare and Medicaid patients as a population are at an inherently higher risk of poor outcomes than the regular population as these patients are either older than 65 or severely disabled. However, even with an increase in complication rates after surgery, Martin et al. found that the publicly funded population ultimately did as well as the privately funded group in bariatric surgery in terms of weight loss and decreasing comorbidities, indicating that even if risks are considerable to publicly employed patients, they still receive significant advantage from bariatric surgery [29].
Ultimately, this study brings up several important questions that facilitate the need for future studies. These disparities in payer status seem to stem from a wide combination of factors related to both the system and current medical culture. Additional concerns include potential motivating factors for surgeons to operate on privately insured patients and surgeon experience contributing to increased complication rates. However, these are all assumptions and thus are questions that need to be assessed by future studies. Public coverage of bariatric surgery could lead to cost savings. Furthermore, there is an economic benefit to increasing access to bariatric surgery. Insurance companies currently contend that individuals will have to pay more annually if surgical options for treatment are made available to all optimal candidates. While this is true, short-term and long-term estimates, 5 to 20 years after initiating the coverage, predict healthcare costs to substantially decrease [33]. Other studies have found similar results, also concluding that bariatric surgery over a lifetime can lead to substantial cost savings to healthcare systems [34,35,36,37,38,39]. Thus, we can assume that an increase in the utilization of bariatric surgery may lead to a decrease in cost due to remission of obesity-related comorbidities.
Strengths of this study include large sample size and completeness of the NIS dataset used. Our results are generalizable to most of the population as the NIS represents 97% of inpatient discharges. There are also several limitations present in this study. First, even though the NIS database provides a large database, it is based on administrative coding and thus has inherent limitations from potential insufficient coding or coding errors. Second, as this is a case-control study, there is possibility for selection and information bias that cannot be disregarded. The study design also relies on others for accurate record keeping, and thus, it is not possible to definitively trust the reliability of the dataset. Furthermore, we considered the hospital charges equivalent to cost which cannot be considered an accurate measure. Finally, we cannot determine causality of any of the associations.
Conclusion
Publicly insured patients are less likely than privately insured and self-paying patients to undergo bariatric surgery and have significantly higher postoperative complications. This could be due to a myriad of factors including prohibitive direct and indirect costs to patients, insurance criteria, and motivations of surgeons. These factors need to be further explored and investigated in order to implement a necessary fundamental change in our health system in order to end the coverage gap between private and publicly insured patients.
References
Mokdad AH, Marks JS, Stroup DF, et al. Actual causes of death in the United States. JAMA. 2000;291:1238–45.
Ogden CL, Carroll MD, Kit BK, et al. Prevalence of obesity in the United States, 2009–2010. NCHS Data Brief. 2012;82:1–8.
Kelly T, Yang W, Chen CS, et al. Global burden of obesity in 2005 and projections to 2030. Int J Obes. 2008;32:1431–7.
Sturm R. Increases in clinically severe obesity in the United States, 1986–2000. Arch Intern Med. 2003;163:2146–8.
Ruhm CJ. Current and future prevalence of obesity and severe obesity in the United States. Forum Health Econ Policy. 2007;10:1086.
Boido A, Ceriani V, Cetta F, et al. Bariatric surgery and prevention of cardiovascular events and mortality in morbid obesity: mechanisms of action and choice of surgery. Nutr Metab Cardiovasc Dis. 2015;25(5):437–43.
Prospective Studies Collaboration. Body-mass index and cause- specific mortality in 900,000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083–96.
Flegal KM, Kit BK, Orpana H, et al. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309(1):71–82.
Andreyeva T, Sturm R, Ringel JS. Moderate and severe obesity have large differences in health care costs. Obes Res. 2004;12:1936–43.
Grieve E, Fenwick E, Yang HC, et al. The disproportionate economic burden associated with severe and complicated obesity: a systematic review. Obes Rev. 2013;14(11):883–94.
Sobal J, Stunkard AJ. Socioeconomic status and obesity: a review of the literature. Psychol Bull. 1989;105:260–75.
McLaren L. Socioeconomic status and obesity. Epidemiol Rev. 2007;29(1):29–48.
Gortmaker SL, Must A, Perrin JM, et al. Social and economic consequences of overweight in adolescence and young adulthood. N Engl J Med. 1993;329(14):1008–12.
Averett S, Korenman S. Black-white differences in social and economic consequences of obesity. Int J Obes. 1999;23:166–73.
Nguyen N, Vu S, Kim E, et al. Trends in utilization of bariatric surgery, 2009-2012. Sure Endosc. 2016;30:2723–7.
NIH conference. Gastrointestinal surgery for severe obesity. consensus development conference panel. Ann Intern Med 1991;115(12):956–961.
Sundbom M. Laparoscopic revolution in bariatric surgery. World J Gastroenterol. 2014;20(41):15135–43.
Li J, Lai D, Wu D. Laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy to treat morbid obesity-related comorbidities: a systematic review and meta-analysis. Obes Surg. 2016;26(2):429–42.
Flanagan E, Ghaderi I, Overby DW, et al. Reduced survival in bariatric surgery candidates delayed or denied by lack of insurance approval. Am Surg. 2016;82(2):166–70.
Healthcare cost and utilization project. Overview of national inpatient sample. http://www.hcup-us.ahrq.gov/nisoverview.jsp. Updated 2013. Access 9, 2013.
Santry HP, Lauderdale DS, Cagney KA, et al. Predictors of patient selection in bariatric surgery. Ann Surg. 2007;245:59–67.
Dallal RM, Bailey L, Guenther L, et al. Comparative analysis of short-term outcomes after bariatric surgery between two disparate populations. Surg Obes Relat Dis. 2008;4:110–4.
Cunningham PJ, Nichols LM. The effects of Medicaid reimbursement on the access to care of Medicaid enrollees: a community perspective. Med Care Res Rev. 2005;62(6):676–96.
Decker SL. In 2011 nearly one-third of physicians said they would not accept new Medicaid patients, but rising fees may help. Health Aff. 2012;31(8):1673–9.
Long SH, Settle RF, Stuart BC. Reimbursement and access to physicians’ services under Medicaid. J Health Econ. 1986;5(3):235–51.
Showalter MH. Physicians’ cost shifting behavior: Medicaid versus other patients. Contemp Econ Policy. 1997;15(2):74–84.
Angus LD, Cottam DR, Gorecki PJ, et al. DRG, costs and reimbursement following Roux-en-Y gastric bypass: an economic appraisal. Obes Surg. 2003;13(4):591–5.
Carbonell AM, Lincourt AE, Matthews BD, et al. National study of the effect of patient and hospital characteristics on bariatric surgery outcomes. Am Surg. 2005;71:308–14.
Martin LF, Tan T-L, Holmes PA, et al. Preoperative insurance status influences postoperative complication rates for gastric bypass. Am J Surg. 1991;161:625–34.
LaPar DJ, Bhamidipati CM, Mery CM, et al. Primary payer status affects mortality for major surgical operations. Ann Surg. 2010;252(3):544–50.
Giacovelli JK, Egorova N, Nowygrod R, et al. Insurance status predicts access to care and outcomes of vascular disease. J Vasc Surg. 2008;48(4):905–11.
Rosen H, Saleh F, Lipsitz S, et al. Downwardly mobile: the accidental cost of being uninsured. Arch Surg. 2009;144(11):1006–11.
Martin LF, Robinson A, Moore BJ. Socioeconomic issues affecting the treatment of obesity in the new millennium. PharmacoEconomics. 2000;18(4):335–53.
Borisenko O, Adam D, Funch-Jensen P, et al. Bariatric surgery can lead to net cost savings to health care systems: results from a comprehensive European decision analytic model. Obes Surg. 2015;25(9):1559–68.
Warren JA, Ewing JA, Hale AL, et al. Cost-effectiveness of bariatric surgery: increasing the economic viability of the most effective treatement for type II diabetes mellitus. Am Surg. 2015;81(8):807–11.
Sanchez-Santos R, Sabench Pereferrer F, Estévez Fernandez S, et al. Is the morbid obesity surgery profitable in times of crisis? A cost-benefit analysis of bariatric surgery. Cir Esp. 2013;91(8):476–84.
Ackroyd R, Mouiel J, Chevallier JM, et al. Cost-effectiveness and budget impact of obesity surgery in patients with type-2 diabetes in three European countries. Obes Surg. 2006;16:1488–503.
Salem L, Devlin A, Sullivan SD, et al. A cost-effectiveness analysis of laparoscopic gastric bypass, adjustable gastric banding and non-surgical weight loss. Surg Obes Relat Dis. 2008;4:26–32.
Ikramuddin S, Klingman D, Swan T, et al. Cost-effectiveness of Roux-en-Y gastric bypass in type diabetes patients. Am J Manag Care. 2009;15:607–15.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Additional information
Study Importance
What Is Known:
• The economic burden of obesity is well documented with substantial disparities in healthcare costs between moderate and severe obesity.
• A negative relationship exists between socioeconomic status and income with BMI.
• Bariatric surgery is not an accessible or viable option for all patients even if deemed medically suitable and optimized for surgery.
Study Adds:
• Publicly insured patients are significantly less likely to undergo bariatric surgery.
• Publicly insured patients experience higher rates of obesity and related complications and thus are most in need of bariatric surgery.
• Self-pay insurance status decreased the risk of postoperative complications after bariatric surgery.
Rights and permissions
About this article
Cite this article
Hennings, D.L., Baimas-George, M., Al-Quarayshi, Z. et al. The Inequity of Bariatric Surgery: Publicly Insured Patients Undergo Lower Rates of Bariatric Surgery with Worse Outcomes. OBES SURG 28, 44–51 (2018). https://doi.org/10.1007/s11695-017-2784-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-2784-5