Abstract
Background
Roux-en-Y gastric bypass (RYGB) effectively treats obesity and gastroesophageal reflux disease (GERD). As more surgeons recommend RYGB to treat GERD in patients with obesity, there are concerns about this approach in patients with previous non-bariatric foregut surgery. This study aims to evaluate the effect of previous non-bariatric foregut surgery on subsequent RYGB.
Methods
Retrospective review of 2089 patients undergoing RYGB between January 1985 and June 2015 was conducted to identify all patients with previous non-bariatric foregut surgery. Perioperative and postoperative data was collected by retrospective chart review.
Results
A total of 11 patients with prior non-bariatric foregut surgery underwent RYGB with median time between operations of 95.6 months. Of note, 7/11 (63.6%) had previous Nissen fundoplication. Conversion to open operation was required in 3/7 (42.9%) with previous Nissen compared to 1/4 (25%) in those without previous Nissen. The average length of stay (LOS) was 3.9 ± 0.9 days, significantly longer than our institutional average for RYGB of 3.2 ± 3.2 days (p = 0.02). Mean percentage of excess body mass index loss (%EBMIL) was 64.7 ± 23.5 at 4-year median follow-up, comparable to our institution’s previously reported data. No mortalities were attributed to RYGB and the overall complication rate was 18.2%, compared to our institutional complication rate for RYGB of 8.5% (p = 0.253).
Conclusion
Despite increased technical difficulty and increase perioperative morbidity, patients undergoing RYGB with previous non-bariatric foregut surgery had long-term symptom resolution and robust weight loss. This indicates that in the right hands, RYGB after non-bariatric foregut surgery may be performed safely and effectively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, there has been an epidemic of obesity throughout the USA and the rest of the world [1]. This epidemic has been associated with a rise in obesity-related comorbidities including gastroesophageal reflux disease (GERD), type 2 diabetes mellitus (DM), hyperlipidemia, hypertension (HTN), obstructive sleep apnea (OSA), heart disease, stroke, asthma, and degenerative joint disease (DJD) [2, 3]. The prevalence of obesity in the USA and worldwide has continued to rise and it is estimated that by 2030, 20% of the world population will be obese [4]. For patients that are unable to lose weight through lifestyle modification or medical therapies, surgical options have been utilized since the 1950s to reduce the burden of obesity-related comorbidities. However, in recent years, Roux-en-Y gastric bypass (RYGB) has emerged as the standard of care in weight loss surgery because it results in both robust weight loss and comorbidity resolution [2].
The incidence of GERD is up to three times greater in patients with obesity compared to that of patients without obesity and patients with obesity have more severe and frequent symptoms [5]. GERD causes a reduction in patient quality of life, as well as increase the incidence of Barrett’s esophagus and esophageal cancers. For many years, Nissen fundoplication has been the standard surgical treatment for patients that have failed maximal medical therapy. However, in more recent years, RYGB has been established as a highly effective treatment for patients with severe gastroesophageal reflux disease [5, 6]. RYGB is not only used to treat obese patients with GERD but also has been used as a primary acid-reducing surgery in patients with obesity who have failed anti-reflux surgery [7]. Studies have shown that after RYGB, patients have reduced symptoms of GERD, improvement in 24-h pH measurements or manometric studies, and reduced esophagitis on endoscopy [7, 8]. Several factors have been implicated in the mechanism behind these findings, including reduced burden of acid-producing cells in the stomach pouch, rapid pouch emptying, promoting weight loss, diverting bile from the Roux limb, and decreased pressure over the lower esophageal sphincter [9, 10]. It is clear that RYGB is an effective treatment option for both obesity and GERD.
There are several studies that have investigated the outcomes of RYGB used for revision of Nissen fundoplication or for weight loss after Nissen fundoplication. A review of the literature conducted in 2015 by Grover et al. highlighted five studies of RYGB for revision of failed anti-reflux operations [11]. Makris et al., Stefanidis et al., and Zainabadi et al. specifically evaluated patients undergoing RYGB as a revision operation after previous anti-reflux operations and included 72, 25, and 7 patients, respectively [12–14]. Furthermore, Houghton et al. and Kellogg et al. evaluated the safety and efficacy of RYGB for weight loss or operative revision after previous anti-reflux operation in 19 and 11 patients, respectively [15, 16]. In these studies, 30-day complication rates ranged from 21 to 46%, rates of conversion to an open operation ranged between 0 and 33%, and patient satisfaction in three of the studies ranged between 88 and 96% (Kellogg et al. and Zainabadi et al. did not report a patient satisfaction). These are studies of RYGB for operative revision of failed Nissen fundoplication and none of these studies have evaluated RYGB solely for the indication of obesity in patients with prior non-bariatric foregut surgery. Our aim in this study is to evaluate the effect of previous non-bariatric foregut surgery on a cohort of patients undergoing RYGB for both weight loss and comorbidity resolution rather than for revision of previous foregut operation. We hypothesized that patients with previous non-bariatric foregut surgery undergoing RYGB will be at higher risk for operative complications with no difference in long-term outcomes.
Materials and Methods
Patients
A prospectively collected database approved by the Institutional Review Board (IRB# 17132) at our institution of all patients undergoing weight loss surgery was queried. This database included patients between 1/1/1985 and 1/1/2014 and all patients with previous non-bariatric foregut surgery undergoing RYGB for morbid obesity were identified. Inclusion criteria include (1) previous non-bariatric surgery on the esophagus, diaphragm, or stomach with an abdominal approach, (2) previous foregut surgery completed at least 1 month before RYGB, and (3) indication for RYGB was weight loss. Exclusion criteria include (1) RYGB performed for failed anti-reflux procedure and (2) additional foregut surgery performed in the same operation as RYGB.
This database included the demographic data (age, sex, race), preoperative weight, preoperative comorbidities (DM, GERD, OSA, HTN, DJD, pulmonary disease, and cardiac disease), postoperative complications/comorbidities (GERD, cardiac disease, DJD, DM, OSA, HTN, pulmonary disease, myocardial infarction, stroke, cancer prevalence, major vitamin deficiency, and incisional hernia), and weights from yearly follow-up appointments. Patient specific data was collected, including details of the initial foregut surgery as well as time between foregut surgery and RYGB. The RYGB operative reports for all 11 patients were reviewed and perioperative data were collected including operative time, laparoscopic versus open approach, need to convert to an open procedure, resection of the fundus, and takedown of the Nissen wrap, and need for extensive enterolysis. All patients in this study were operated on by one of two attending bariatric surgeons at our institution. Postoperative outcomes were collected such as length of stay (LOS), percentage of excess body mass index loss (%EBMIL), evidence of anastomotic leak, significant postoperative bleeding, postoperative malnutrition, episodic postoperative hypoglycemia, and recurrence of GERD symptoms as noted in the electronic medical record.
Definitions
Comorbidity information was collected using a prospectively collected database for preoperative data. Long-term data were collected through a prospective database and retrospective chart review. Weight loss is reported as change in BMI, percentage of total weight lost, and %EBMIL, with 25 kg/m2 used as the ideal body mass index (BMI) to calculate %EBMIL. Readmission is defined as any documented hospital admissions within 30 days of RYGB.
Statistical Analysis
The primary outcome was incidence of postoperative complication in prior foregut surgery patients versus that of our standard population. Secondary outcomes included percent reduction in excess BMI and long-term comorbidity resolution. Statistical analysis was performed using Student’s T test and χ 2 test to calculate significance. A p value of <0.05 was used for statistical significance.
Results
We identified a total of 11 patients (8 female, 3 male) that underwent RYGB after previous non-bariatric foregut surgery, with median time between interventions of 95.6 months (range 2.9–260.4). All RYGB operations were conducted between 1997 and 2013 at our institution. In total, 7/11 (63.6%) patients had a prior Nissen fundoplication before RYGB. Three were completed without hiatal hernia repair, three were done with concomitant hiatal hernia repair, and one patient had a paraesophageal hernia repair with Goretex Dualmesh (Flagstaff, AZ, USA) mesh after failed Nissen fundoplication. There were 4 patients that had prior foregut operation without creation of a Nissen wrap. One patient had a primary laparoscopic hiatal hernia repair without mesh placement. One patient was scheduled for laparoscopic gastric band placement but intraoperatively was found to have leiomyomas of the distal esophagus and proximal stomach that required resection. An additional patient underwent resection of a leiomyoma of the distal esophagus. The fourth patient had a gunshot wound to the upper abdomen requiring extensive diaphragmatic repair along with laparotomy, thoracotomy, and pericardial window.
The median age at the time of RYGB was 50 years (range 32–65) and median preoperative BMI was 43 (range 38–56). Table 1 details preoperative comorbidities for the entire cohort, as well as for the subsets of patients with and without prior Nissen fundoplication. Of note, the prevalence of GERD in the entire cohort is 81.8% and it is similar in patients with previous Nissen fundoplication (85.7%). The median operative time was 238 min with a range of 170–335. There was no statistically significant difference shown between operative times of our cohort compared to previously reported data from our institution (p = 0.84) [17]. In patients with a previous Nissen fundoplication, 3 (42.9%) required conversion to an open procedure, compared to 1 (25%) conversion in patients without previous Nissen fundoplication. All RYGB surgeries converted to open in this study were done after 2003, when laparoscopic RYGB was well established and commonly performed at our institution. Extensive enterolysis, as noted by the surgeon in the operative note, was required in 4 (57.1%) patients with previous Nissen fundoplication while in patients without previous Nissen fundoplication, only 1 (25%) patient requiring extensive enterolysis. The Nissen wrap was taken down in 5 (71.4%) patients and the fundus was resected in 1 (14.3%) patient. One patient did not have the wrap taken down because there were too many dense adhesions to adequately take it down. The other patient without wrap takedown was found intraoperatively to have a slightly attenuated wrap and the surgeon elected to create the gastric pouch below the wrap.
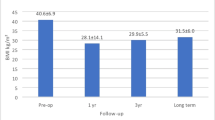
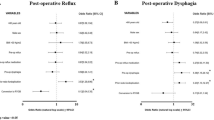
Postoperative and long-term outcomes for our cohort are shown in Table 2. The mean LOS was 3.9 ± 0.9 days, which is significantly longer than the average LOS at our institution for RYGB of 3.2 ± 3.2 days (p = 0.02). The median change in BMI was 11.9 (range 5.7–20.1) and the median percent total weight lost was 27.0% (range 14.4–44.7%). The median follow-up time was 3.1 years with a range of 0.5–10.9 years and 10/11 (90.9%) patients had over 1 year of follow-up. The mean %EBMIL was 64.7% ± 23.5 at a median follow-up time of 3.1 years, which is comparable to our institution’s previously reported %EBMIL 74.7 ± 22.7 at 2 years, and 52.5 ± 33.8 at 10 years (p = 0.62) [17]. In our cohort, one patient was readmitted for conservative management of bowel obstruction and another was readmitted for resuscitation due to nausea, vomiting, and inability to tolerate food by mouth. Therefore, our readmission rate of 2/11 (18.2%) is higher than our institution’s previously published rate of 6.5%, however, this is not a statistically significant difference (p = 0.117) [18]. The overall complication rate was 2/11 (18.2%), which is higher than our institutions previously published rate of 8.5%, however, this was not a statistically significant difference (p = 0.253) [18]. There were no cases of anastomotic leak or significant postoperative bleeding requiring transfusion or reoperation but there was 1/11 (9.1%) patients with postoperative malnutrition considered to be related to RYGB and 1/11 (9.1%) patients with persistent daily symptoms of GERD. One patient in the cohort died as a result of urosepsis 6 years after RYGB; however, this was not considered to be related to the patient’s RYGB.
Discussion
This study suggests that previous non-bariatric foregut surgeries make subsequent RYGB a more technically difficult procedure. In this study, there was a higher rate of conversion to an open operation, with 36.3% of our entire cohort requiring a conversion to open. This effect was further amplified in our patients with previous Nissen fundoplication, as 42.9% of this subset of patients required an open procedure while only 25% of our patients without a previous Nissen required conversion to open. The rate of conversion to open in this study is higher than that of other series of patients with RYGB after non-bariatric foregut surgery, with rates ranging between 0 and 33% [12–16]. In our population, this is likely related to the presence of intraabdominal adhesions, as a higher proportion of patients with previous Nissen fundoplication required extensive enterolysis, compared to patients with non-Nissen foregut surgery. Additionally, 5/7 (71.4%) patients with previous Nissen fundoplication underwent takedown of the Nissen wrap or fundus resection. The two attending surgeons at our institution have different approaches to takedown of the Nissen wrap, with one attempting to preserve the wrap if possible and the other preferring to take the wrap down. For the surgeon that attempts to preserve the wrap, 4/5 (80%) patients with a previous Nissen required the wrap to be taken down. Despite differing approaches to wrap takedown, it is clear that for our patients, the presence of previous Nissen fundoplication further complicated RYGB. Furthermore, the high rate of conversion to open surgery in our cohort is likely related to post-surgical changes from the initial non-bariatric foregut surgery, the presence of intraabdominal adhesions, and the necessity of Nissen wrap takedown in patients with previous Nissen fundoplication.
Gastric bypass after a Nissen fundoplication is a difficult and complex procedure. There are frequently adhesions to take down, and separating the fundic wrap from the body of the stomach is often difficult. Whether the wrap should be taken down is also controversial. Care must be taken to preserve the cardia of the stomach where the pouch will be created. It is not unusual to damage the fundus while dissecting and resection of the fundus may be required. We recommend intraoperative endoscopy to assess the pouch and gastrojejunostomy anastomosis. In a patient population requiring special considerations during laparoscopic procedures, these additional factors make RYGB a more technically difficult procedure. The increased technical difficulty translated to increased perioperative morbidity in this study, as patients with prior foregut surgery in this study had longer LOS than average patients undergoing RYGB at our institution. There was a higher rate of readmission within 30 days; however, this was not a statistically significant difference. Our cohort includes 11 patients, while the reference data includes over 2000 patients; the lack of statistical significance is likely related to the comparatively small sample size in the present study. While there is no statistical significance shown between readmission rates, this could represent a clinically significant finding and further study is required in this area.
In our study, 2/11 (18.2%) patients had long-term complications and there was no statistically significant difference when comparing to previously published data from our institution. However, the complication rate in our study is slightly lower than rates reported in other studies (21–46%) [12–16]. One patient had persistent gastroparesis, dysphagia, and GERD; however, postoperative endoscopic evaluation did not reveal any targets for intervention. This raises the question of whether this represents a failed surgical operation or disease not amenable to surgical intervention. One patient was diagnosed with malnutrition by the surgeon because of poorly controlled, excessive weight loss at follow-up visits. There were no cases of anastomotic leak or significant bleeding requiring transfusion or reoperation. While there was no statistically significant difference demonstrated for long-term complications in this study, considering our small cohort of 11 patients, additional studies are required to determine the clinical significance of this finding. However, considering 9/11 (81.8%) patients presented with preoperative GERD and only 1/11 (9.1%) had persistent GERD indicates that patients in this study had considerable resolution of GERD symptoms. Patients also maintained a mean %EBMIL of 64.7% at median follow-up time of 3.1 years, which is comparable to previously published data of patients undergoing RYGB at our institution. Therefore, despite increased technical difficulty and perioperative morbidity, patients in our study had considerable resolution of GERD symptoms and maintained a robust %EBMIL.
These data demonstrate RYGB for patients with prior non-bariatric foregut surgery is a more technically demanding procedure, as patients had a higher rate of conversion to an open operation and a longer LOS. Additionally, for patients in this study with a previous Nissen fundoplication, the presence of intraabdominal adhesions, the potential need for Nissen wrap takedown, and possible resection of the fundus further increased the technical difficulty. However, these patients had considerable reduction in symptoms of GERD as well as robust weight loss. Previous non-bariatric foregut surgery made the operation more technically difficult, but in experienced hands, it was still feasible to perform safe and effective RYGB for our patients. While this study has a small sample size, for a relatively small population of patients requiring special considerations, the surgeon must weigh the possible risks of increased complications and readmission rates with the potential benefit of long-term symptom resolution and robust weight loss. Surgeons evaluating patients for RYGB with previous non-bariatric foregut surgery have to rely primarily on personal experience, as there are few studies of these patients. This study therefore can be useful to inform both surgeons and patients on the expectations for weight loss and complications expected postoperatively in this special population.
The limitations of this paper include the small single-center experience with two primary bariatric surgeons and the retrospective nature of the study. There is also heterogeneity between the types of previous foregut surgery for patients in the cohort and this heterogeneity limits the generalizability of this study. The database we used to track all patients undergoing surgery has been prospectively collected for the past 30 years. The data is regularly updated when patients are seen in clinic for routine follow-up. Out of over 2000 patients in our database, only 11 were identified with RYGB after previous non-bariatric foregut surgery. This low proportion represents the low incidence of RYGB in patients with prior foregut surgery, however, given the perceived increased risk, this study represents an important addition to the literature. Our cohort of 11 patients is very small, which limits the power of statistical analyses within the cohort and when comparing to the cohort of all patients operated on at our institution. Additionally, while our cohort of 11 patients is a small sample size, it is comparable in size to previous studies evaluating patients undergoing RYGB for weight loss surgery after non-bariatric foregut surgery. Additionally, this study specifically evaluated patients with previous non-bariatric foregut surgery undergoing RYGB for weight loss, rather than as a revision of failed anti-reflux operation.
Conclusion
This study demonstrates that based on our experience of 11 patients with previous non-bariatric foregut surgery undergoing subsequent RYGB, patients had a higher rate of readmission and long-term complications but with considerable symptom resolution and robust weight loss. While other work has been focused on outcomes of RYGB for failed anti-reflux operation, this is one of the only studies of RYGB specifically for weight loss after previous non-bariatric foregut surgery. With a small cohort of patients, there was no statistical significance demonstrated for readmission rates or long-term complication rates, yet further study is required to elucidate the clinical significance of this finding. However, we have demonstrated that our patients had considerable resolution of GERD symptoms from 81.8 to 9.1% and robust weight loss. Therefore, while previous non-bariatric foregut surgery makes the performance of RYGB more technically difficult, in experienced hands, it is still feasible to perform safely and effectively. Considering the symptom resolution and robust weight loss for patients in our cohort, this raises the question of whether the presence of GERD symptoms in a patient with obesity should lower the BMI threshold for surgery as in patients with obesity and diabetes. Future study may be directed at the appropriateness of a lower threshold BMI to perform RYGB for patients with obesity and GERD.
References
Sturm R. Increases in clinically severe obesity in the United States, 1986-2000. Arch Intern Med. 2003;163(18):2146–8.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004 Oct 13;292(14):1724–37.
World Health Organization. World Health Report 2002. Available at: http://www.who.int/whr/2002/en/. Accessed November 1, 2016
Smith KB; Smith MS. Obesity statistics. Prim Care. 43(1):121–135, 2016 Mar.
Nelson LG, Gonzalez R, Haines K, et al. Amelioration of gastroesophageal reflux symptoms following Roux-en-Y gastric bypass for clinically significant obesity. Am Surg. 2005;71(11):950–3. discussion 3-4
Kindel TL, Oleynikov D. The improvement of gastroesophageal reflux disease and Barrett’s after bariatric surgery. Obes Surg. 2016;26(4):718–20.
Kim M, Navarro F, Eruchalu CN, et al. Minimally invasive Roux-en-Y gastric bypass for fundoplication failure offers excellent gastroesophageal reflux control. Am Surg. 2014;80(7):696–703.
Pallati PK, Shaligram A, Shostrom VK, et al. Improvement in gastroesophageal reflux disease symptoms after various bariatric procedures: review of the bariatric outcomes longitudinal database. Surg Obes Relat Dis. 2014;10(3):502–7.
Houghton SG, Romero Y, Sarr MG. Effect of Roux-en-Y gastric bypass in obese patients with Barrett’s esophagus: attempts to eliminate duodenogastric reflux. Surg Obes Relat Dis. 2008;4(1):1–4. discussion 1-5
Naik RD, Choksi YA, Vaezi MF. Impact of weight loss surgery on esophageal physiology. Gastroenterol Hepatol (N Y). 2015;11(12):801–9.
Grover BT, Kothari SN. Reoperative antireflux surgery. Surg Clin North Am. 2015;95(3):629–40.
Makris KI, Panwar A, Willer BL, et al. The role of short-limb Roux-en-Y reconstruction for failed antireflux surgery: a single-center 5-year experience. Surg Endosc. 2012;26(5):1279–86.
Stefanidis D, Navarro F, Augenstein VA, et al. Laparoscopic fundoplication takedown with conversion to Roux-en-Y gastric bypass leads to excellent reflux control and quality of life after fundoplication failure. Surg Endosc. 2012;26(12):3521–7.
Zainabadi K, Courcoulas AP, Awais O, et al. Laparoscopic revision of Nissen fundoplication to Roux-en-Y gastric bypass in morbidly obese patients. Surg Endosc. 2008;22(12):2737–40.
Houghton SG, Nelson LG, Swain JM, et al. Is Roux-en-Y gastric bypass safe after previous antireflux surgery? Technical feasibility and postoperative symptom assessment. Surg Obes Relat Dis. 2005;1(5):475–80.
Kellogg TA, Andrade R, Maddaus M, et al. Anatomic findings and outcomes after antireflux procedures in morbidly obese patients undergoing laparoscopic conversion to Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2007;3(1):52–7.
Mehaffey JH, DJ LP, Clement KC, et al. 10-year outcomes after Roux-en-Y gastric bypass. Ann Surg. 2015a;264(1):121–6.
Mehaffey JH, LaPar DJ, Turrentine FE, et al. Outcomes of laparoscopic Roux-en-Y gastric bypass in super-super-obese patients. Surg Obes Relat Dis. 2015b;11(4):814–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
The authors declare that they have no conflict of interest.
Source of Funding
The National Heart, Lung, and Blood Institute of the National Institutes of Health under Award Number T32HL007849 supported research reported in this publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study. This study was approved by our institution’s Institutional Review Board (IRB# 17132). A prospectively collected database approved by the Institutional Review Board (IRB# 17132) at our institution of all patients undergoing weight loss surgery was queried.
Statement of Human Rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Watson, M.D., Hunter Mehaffey, J., Schirmer, B.D. et al. Roux-en-Y Gastric Bypass Following Nissen Fundoplication: Higher Risk Same Reward. OBES SURG 27, 2398–2403 (2017). https://doi.org/10.1007/s11695-017-2643-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-2643-4