Abstract
Background
Morbid obese patients have a high rate of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH). NASH is related to the progression and poor evolution of chronic hepatopathy in NAFLD, so that its detection makes it possible to identify the subjects who are most at risk in order to prioritize treatment. The ELF test (Enhanced Liver Fibrosis test; Siemens Diagnostics, NY, USA) has been assessed for its capacity to detect fibrosis in patients with NAFLD, but its capacity for diagnosing NASH has not been checked.
Aims
Our objective is to determine the utility of the ELF test for detecting NASH in morbid obese patients with suspected NAFLD.
Methods
ELF values were determined in a cohort of obese patients who underwent bariatric surgery with suspected NAFLD. Liver biopsy was used as the reference standard.
Results
The values of ELF were significantly higher in patients with NASH (p = 0.002) and in those who presented with metabolic syndrome (p = 0.047). An ELF cut-off point of 8.72 allows the detection of patients with NASH with a sensitivity of 71.4% and a specificity of 74.1% (AUC = 0.742, p = 0.002).
Conclusions
The ELF test is efficient for the identification of obese patients with NAFLD and early signs of steatohepatitis and fibrosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nonalcoholic fatty liver disease (NAFLD) is a chronic liver disease characterized by the presence of ectopic fat in the liver, steatosis, which cannot be explained by alcohol consumption [1].
The spectrum of NAFLD includes two major variants which differ substantially in natural history and prognosis. Simple steatosis is generally considered a benign and reversible process, but can progress to the more serious liver disease, nonalcoholic steatohepatitis (NASH), which can develop into progressive fibrosis and liver cirrhosis in the long term [2]. Identification of NASH patients is crucial, as they are at a high risk from cirrhosis and liver-related death [1].
Epidemiological studies indicate that obesity, insulin resistance, diabetes mellitus, and metabolic syndrome (MS) are established risk factors of NAFLD [2, 3]. In overweight subjects, the prevalence of steatosis is at least two times greater than in lean subjects, and in morbid obesity the prevalence of NAFLD and NASH is nearly 90 and 37%, respectively.
At present, liver biopsy is required for the diagnosis of NAFLD, but is invasive, subject to sampling variability and occasionally associated with serious complications. Therefore, there is an urgent unmet need to develop noninvasive methods that facilitate diagnosis, identification of populations at risk, and assessment of disease progression [4].
Blood serum markers are a noninvasive alternative that allows for a more widespread use. Traditionally, these biomarkers have been proposed to identify advanced fibrosis in NAFLD patients, but the early detection of NASH would make it possible to anticipate the natural course of the disease, allowing therapeutic action to be proposed before the appearance of fibrosis.
The ELF test measures three markers of liver matrix metabolism in serum: hyaluronic acid (HA), tissue inhibitor of metalloproteinase-1 (TIMP-1), and amino-terminal propeptide of type III procollagen (PIIINP), which are combined to calculate the ELF score. This algorithm was designed in a mixed cohort of patients with chronic liver disease [5] and has been subsequently validated in a population of patients with NAFLD, with good results for identifying hepatic fibrosis [6]. Also, the ELF score is a valuable tool for risk stratification in patients with chronic liver disease [7]. However, it has not been evaluated for the identification of NASH in patients with suspected NAFLD.
The aim of this study is to evaluate the clinical utility of the ELF algorithm, in the identification of NASH in obese patients with suspected NAFLD using liver biopsy as a reference standard.
Patients and Methods
Patients
The study population consisted of 57 obese patients who underwent bariatric surgery at the “Virgen de la Arrixaca” University Hospital in Murcia (Spain) and had suspected NAFLD.
The patients were prospectively included if they fulfilled the criteria for bariatric surgery [8] and they had suspected NAFLD criteria that indicated the need to perform a liver biopsy to confirm the diagnosis and for grading the liver disease:
-
BMI above 40 kg/m2 or above 35 kg/m2 with significant obesity-related comorbidities.
-
Acceptable operative risk.
-
Documented failure of nonsurgical weight loss programs.
-
Clinical, analytic or radiological criteria for suspicion of NAFLD: abnormal liver tests and/either ultrasound results suggestive of liver steatosis or liver dysmorphy and/or a macroscopically abnormal liver, as observed by the surgeon.
The exclusion criteria were alcohol intake higher than 20 g/day and other causes of liver disease (hepatitis C or B, autoimmune liver disease, hemochromatosis, or treatment with steatosis-inducing drugs).
All the patients received a laparoscopic Roux-en-Y gastric bypass and during surgery a liver biopsy was obtained.
Laboratory and Clinical Parameters
Clinical data were recorded the week prior to the liver biopsy and included age, sex, BMI, hypertension, diabetes, dyslipidemia, and MS. MS was diagnosed according to the criteria of the Adult Treatment Panel III [9].
The day prior to the liver biopsy blood samples were collected. The laboratory tests included complete blood count, coagulation panel, glucose, urea, creatinine, total protein, total bilirubin, albumin, total cholesterol, triglycerides, aspartate aminotransferase (AST), alanine aminotransferase (ALT), γ-glutamyltransferase (GGT), alkaline phosphatase (ALP), haptoglobin, ApoA-1 and α2-macroglobulin. Furthermore, serum samples were analyzed for HA, TIMP-1, and PIIINP. Levels of TIMP-1, HA, and PIIINP were measured using an ADVIA Centaur XP automated immunoanalyzer (Siemens Healthcare Diagnostics Inc). Both TIMP-1 and PIIINP assays use two monoclonal antibodies that bind to different binding sites on their respective antigens. The HA assay utilizes HA binding protein instead of monoclonal antibodies. Results were entered into the manufacturer’s published algorithm to derive an ELF score [ELF = 2.278 + 0.851 ln(HA) + 0.751 ln(PIIINP) + 0.394 ln(TIMP-1)]; ln = natural logarithm.
Assessment of Hepatic Histology
Liver biopsies were performed on the right lobe (segment VI) by bariatric surgeons in conditions of direct visualization. All the tissue wedges were studied by the same pathologist, who was blinded to the other results.
The classification by Matteoni et al. [10], that divides the histological findings into four studies as shown in Table 1, was used to grade liver biopsies for the severity of NAFLD. The patients were classed into two groups according to histological findings: group A, healthy liver and simple steatosis and group B, NASH and/or fibrosis.
Statistical Analysis
The quantitative variables were compared using Studentʼs t test or the Mann-Whitney U test and the qualitative variables were compared using the Chi-squared test with Fisherʼs exact test, if it was relevant. The correlation between continuous variables was calculated using Pearsonʼs or Spearmanʼs coefficient correlation.
The ROC curve of the ELF algorithm was analyzed to evaluate its capacity to identify patients with steatohepatitis. The optimal cut-off point was calculated according to Youdenʼs index [11] together with values of sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV).
Results
Clinical Parameters
The study population consisted of 57 patients. 75.4% of subjects were female and their mean age was 43.95 years. The mean BMI was 49.09 kg/m2 and 24.6% of subjects had evidence of diabetes, 64.9% dyslipidemia, 47.4% hypertension, and 45.6% MS.
Histopathological Findings
Four of the patients presented with a normal liver in the histopathological study but in most of the patients, multiple alterations were observed. The distribution of histological findings is shown in Table 1.
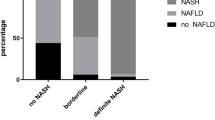
Group A consisted of 28 patients (49.12%) with a healthy liver or simple steatosis and group B included 29 patients (50.8%) with NASH and/or fibrosis. Table 2 shows clinical and demographic characteristics of the patients in both groups. Only the variables of hypertension and MS showed significant differences between groups.
Laboratory Parameters
All the hematological and biochemical variables were compared between both groups of patients, without any significant differences being found between any of them (Table 3).
The ELF values for each stage of the Matteoniʼs classification are shown in Table 1. Significant differences were found after analyzing the findings of the ELF test in both groups of patients with higher values in the patients in group B (Table 4).
We analyzed the ELF values according to the clinical and demographic characteristics of the patients. In no cases were differences found according to sex, and in the case of BMI, the values tended to be higher as this index increased, although the differences were not statistically significant. Significantly higher levels of ELF were found in the patients who presented with MS (p = 0.047); see Fig. 1. However, by studying each of the variables of the MS on an individual basis (hypertension, dyslipidemia, and diabetes), we found that ELF was higher in all cases in affected patients, although significant differences were only found in the case of hypertense patients (p = 0.030).
A significant correlation was found between the ELF test result and age (r = 0.470; p = 0.001).
To assess the utility of the ELF algorithm, a ROC curve was calculated, taking the identification of the patients with steatohepatitis as the state variable, namely those included in group B, and the area below the curve (AUC) was 0.742 (95% CI 0.607–0.874), p = 0.002. In Table 5, the cut-off point and the values associated for sensitivity, specificity, PPV, and NPV are shown. Figure 2 reflects the AUC.
Discussion
NAFLD is considered to be a complex condition with a phenotype reflecting an interaction between different factors related to lifestyle, the environment and genetics. It has been calculated that there is an approximate disease incidence of 30% in the general population [12]. A recent study showed that cirrhosis associated with NASH is the third most common indication for liver transplantation in the USA, and it is expected that for the year 2020, it will become the first indication [2].
Obesity is associated with MS, heart disease, insulin resistance, and diabetes, leading to a higher risk of developing NAFLD. The NAFLD prevalence has been found to be between 75 and 100% in morbid obese patients [13].
The demographic characteristics of our population are comparable to those reported in similar recent studies [14–17] confirming that our population is representative of the type of patient who undergoes this type of surgery.
Regarding the comorbidities affecting the patients, our results confirm that NAFLD is associated with the components of MS [2, 18]. When we compare both groups, it can be seen that there are significant differences between the percentage of hypertense patients and the percentage affected by MS, with a higher rate in patients in group B. This reflects the association between these variables and an increased risk of developing an advanced stage of the disease [2, 14, 19].
If we consider the hematological and biochemical parameters in the global population, there were no values outside the normal ranges, and in no cases were there significant differences on comparing both groups, although the AST variable was very near to reaching significance. These results reflect the fact that many of the patients with NAFLD remain asymptomatic showing few or no changes in the laboratory parameters, meaning that it is difficult to identify them using basic blood tests.
The mean ELF value obtained in our population was 8.67, higher than in other studies that assessed this test in healthy patients with a normal BMI and without any signs of MS, such as Lichtinghagen et al. [20] and Yoo et al. [21], who showed mean values of 8.06 and 7.75, respectively. This brings to light the relationship that exists between ELF and the hepatic alterations involved in NAFLD. On comparing the ELF values between both groups of patients, significant differences were found. What is more, when these values were studied according to only the clinical and demographic characteristics of the patients, significant differences were found according to arterial hypertension and MS.
The analysis of correlations revealed the existence of significant relationships between ELF and age. These results coincide with those provided by other studies [5, 20, 22] suggesting that age needs to be considered when interpreting the ELF result. The relationship between ELF and age is predictable, due to the fact that an advanced age is associated with the progression of fibrosis, perhaps owing to the greater vulnerability towards environmental factors, particularly oxidative stress. However, these results contradict with those reported in the study by Yoo et al. [21] that suggested an absence of differences in ELF values according to age, and also with those reported in the studies by Guha et al. [6] and Parkes et al. [23], which simplified the original ELF algorithm eliminating age without affecting diagnostic accuracy. Taking into account all these data, it is clear that the values of ELF should be interpreted with caution taking into account patient age, although the age of our population was very homogenous, and no significant differences were found between both groups of patients, so that our results will not have been affected by this factor.
The analysis of ELF ROC curves provided significant results. In the original study that designed the ELF algorithm, an AUC of 0.870 was obtained for the detection of moderate-severe fibrosis with a sensitivity of 89% and a specificity of 96% in NAFLD patients [5]. Subsequently, the study by Guha et al. [6] simplified the algorithm and validated it in an independent cohort of patients with NAFLD obtaining equally good results. There have been other studies that have assessed the ELF algorithm in patients with NAFLD. This is the case of Nobili et al. [24] and Alkhouri et al. [25], who assessed the algorithm in pediatric patients obtaining good results for the detection of fibrosis. Similarly Dvorak et al. [26] reported a good diagnostic performance for the identification of significant fibrosis. Szybowska et al. [27] also found that the ELF test value was significantly higher in obese children with ultrasound-proven steatosis, although they should take into account the limitations of ultrasound for identifying steatosis [12]. On the other hand, the recent study by Irvine et al. [28] shows a new model in which diagnostic accuracy was superior compared to the ELF test, although it should be noted that they use a mixed-etiology cohort of patients and their objective was to identify advanced fibrosis, making it substantially different from the present study.
Using a compilation of the results of all these studies, we can deduce that the ELF test has been assessed in cohorts of patients with different characteristics but always with the aim of detecting fibrosis, providing different cut-off points depending on the types of patients and the stage of fibrosis that was fixed as the objective, and obtaining good results.
The cut-off point proposed in our study is associated with optimal sensitivity and specificity values. These are good results if we take into account that the objective is not only restricted to the detection of patients with fibrosis, but actually includes pathological stages belonging to NAFLD which can occur in conjunction with or prior to the fibrosis. It is important to detect the disease at these stages because then the therapeutic effort is more beneficial as the natural course of the disease can be anticipated.
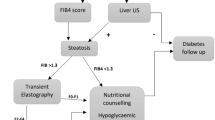
To conclude, the evidence presented in this study shows that the ELF test represents a valid and efficient option for the identification of obese patients with NAFLD and early stages of steatohepatitis and fibrosis, so that its use would be very convenient for the evaluation and stratification of a growing number of patients with suspicion of this disease. In the case of patients who are going to be subjected to bariatric surgery, the use of ELF would make it possible to presurgically identify those patients with more severe hepatopathy, thus establishing a population at risk in which surgery could be prioritized, and to propose prior therapeutic actions to reduce postsurgical morbidity and mortality related to hepatopathy.
References
Lassailly G, Caiazzo R, Buob D, et al. Bariatric surgery reduces features of nonalcoholic steatohepatitis in morbidly obese patients. Gastroenterology. 2015;149:379–88.
Machado MV, Cortez-Pinto H. Non-alcoholic fatty liver disease: what the clinician needs to know. World J Gastroenterol. 2014;20:12956–80.
Petrick A, Benotti P, Wood GC, Still CD, Strodel WE, Gabrielsen J, Rolston D, Chu X, Argyropoulos G, Ibele A, Gerhard GS: Utility of ultrasound, transaminases, and visual inspection to assess nonalcoholic fatty liver disease in bariatric surgery patients. Obes Surg. 2015.
Sanyal AJ, Friedman SL, McCullough AJ, et al. Challenges and opportunities in drug and biomarker development for nonalcoholic steatohepatitis: findings and recommendations from an American Association for the Study of Liver Diseases-U.S. Food and Drug Administration Joint Workshop. Hepatology. 2015;61:1392–405.
Rosenberg WM, Voelker M, Thiel R, et al. Serum markers detect the presence of liver fibrosis: a cohort study. Gastroenterology. 2004;127:1704–13.
Guha IN, Parkes J, Roderick P, et al. Noninvasive markers of fibrosis in nonalcoholic fatty liver disease: validating the European liver fibrosis panel and exploring simple markers. Hepatology. 2008;47:455–60.
Irvine KM, Wockner LF, Shanker M, et al. The enhanced liver fibrosis score is associated with clinical outcomes and disease progression in patients with chronic liver disease. Liver Int. 2016;36:370–7.
Salas-Salvado J, Rubio MA, Barbany M, et al. SEEDO 2007 consensus for the evaluation of overweight and obesity and the establishment of therapeutic intervention criteria. Med Clin (Barc). 2007;128:184–96.
Third Report of the National Cholesterol Education Program (NCEP) Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–421.
Matteoni CA, Younossi ZM, Gramlich T, et al. Nonalcoholic fatty liver disease: a spectrum of clinical and pathological severity. Gastroenterology. 1999;116:1413–9.
Youden WJ. Index for rating diagnostic tests. Cancer. 1950;3:32–5.
Lee SS, Park SH. Radiologic evaluation of nonalcoholic fatty liver disease. World J Gastroenterol. 2014;20:7392–402.
Schwenger KJ, Allard JP. Clinical approaches to non-alcoholic fatty liver disease. World J Gastroenterol. 2014;20:1712–23.
Naveau S, Lamouri K, Pourcher G, et al. The diagnostic accuracy of transient elastography for the diagnosis of liver fibrosis in bariatric surgery candidates with suspected NAFLD. Obes Surg. 2014;24:1693–701.
Diez-Rodriguez R, Ballesteros-Pomar MD, Calleja-Fernandez A, et al. Insulin resistance and metabolic syndrome are related to non-alcoholic fatty liver disease, but not visceral adiposity index, in severely obese patients. Rev Esp Enferm Dig. 2014;106:522–8.
Feijo SG, Lima JM, Oliveira MA, et al. The spectrum of non alcoholic fatty liver disease in morbidly obese patients: prevalence and associate risk factors. Acta Cir Bras. 2013;28:788–93.
Pulzi FB, Cisternas R, Melo MR, et al. New clinical score to diagnose nonalcoholic steatohepatitis in obese patients. Diabetol Metab Syndr. 2011;3:3.
Dyson JK, Anstee QM, McPherson S. Non-alcoholic fatty liver disease: a practical approach to treatment. Frontline Gastroenterol. 2014;5:277–86.
Vernon G, Baranova A, Younossi ZM. Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment Pharmacol Ther. 2011;34:274–85.
Lichtinghagen R, Pietsch D, Bantel H, et al. The enhanced liver fibrosis (ELF) score: normal values, influence factors and proposed cut-off values. J Hepatol. 2013;59:236–42.
Yoo EJ, Kim BK, Kim SU, et al. Normal enhanced liver fibrosis (ELF) values in apparently healthy subjects undergoing a health check-up and in living liver donors in South Korea. Liver Int. 2013;33:706–13.
Fagan KJ, Pretorius CJ, Horsfall LU, et al. ELF score >/=9.8 indicates advanced hepatic fibrosis and is influenced by age, steatosis and histological activity. Liver Int. 2015;35:1673–81.
Parkes J, Guha IN, Roderick P, et al. Enhanced liver fibrosis (ELF) test accurately identifies liver fibrosis in patients with chronic hepatitis C. J Viral Hepat. 2011;18:23–31.
Nobili V, Parkes J, Bottazzo G, et al. Performance of ELF serum markers in predicting fibrosis stage in pediatric non-alcoholic fatty liver disease. Gastroenterology. 2009;136:160–7.
Alkhouri N, Carter-Kent C, Lopez R, et al. A combination of the pediatric NAFLD fibrosis index and enhanced liver fibrosis test identifies children with fibrosis. Clin Gastroenterol Hepatol. 2011;9:150–5.
Dvorak K, Stritesky J, Petrtyl J, et al. Use of non-invasive parameters of non-alcoholic steatohepatitis and liver fibrosis in daily practice—an exploratory case-control study. PLoS One. 2014;9:e111551.
Szybowska P, Wojcik M, Starzyk JB, et al. Enhanced liver fibrosis (ELF) test in obese children with ultrasound-proven liver steatosis. Neuro Endocrinol Lett. 2015;36:700–5.
Irvine KM, Wockner LF, Hoffmann I, et al. Multiplex serum protein analysis identifies novel biomarkers of advanced fibrosis in patients with chronic liver disease with the potential to improve diagnostic accuracy of established biomarkers. PLoS One. 2016;11:e0167001.
Acknowledgments
We would like to thank the patients for their voluntary and disinterested participation in the study. Our thanks to Siemens® for the free use of the material for the evaluation of the ELF test.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest. Iria Cebreiros reports grants from Spanish Association of Pharmaceutical Analysts (AEFA), and nonfinancial support from Siemens Healthcare Diagnostics Inc.
Statement of Informed Consent
Informed consent was obtained from all the participants.
Statement of Human Rights
The study was approved by our hospital’s Ethics and Clinical Research Committee.
Additional information
Iria Cebreiros holds a research grant from the Spanish Association of Pharmaceutical Analysts (AEFA).
Rights and permissions
About this article
Cite this article
López, I.C., Aroca, F.G., Bernal, M.D.F. et al. Utility of the ELF Test for Detecting Steatohepatitis in Morbid Obese Patients with Suspicion of Nonalcoholic Fatty Liver Disease. OBES SURG 27, 2347–2353 (2017). https://doi.org/10.1007/s11695-017-2606-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-2606-9