Abstract
Background
Bariatric surgery (BS) is known to favorably impact fasting lipid profile. Fasting and postprandial lipids were evaluated before and 2 years after BS in obese type 2 diabetic (T2DM) patients.
Methods
A prospective study was conducted in 19 obese T2DM patients: ten undergoing sleeve gastrectomy (SG) and nine undergoing Roux-en-Y gastric bypass (RYGB). Before and 2 years after BS, clinical parameters and the response of lipid and incretin hormones to a mixed meal (MM) were assessed.
Results
The two groups had similar characteristics at baseline. After BS, weight loss was similar in the two groups (p ≤ 0.01). Fasting glucose, insulin, and triglycerides decreased while HDL cholesterol increased in a similar way (p < 0.05); in contrast, fasting LDL cholesterol decreased only after RYGB (p < 0.05). Post-meal glucose concentrations decreased while early insulin response significantly improved after both procedures (p < 0.001 for both). Postprandial triglycerides decreased after both procedures (p < 0.05) while postprandial LDL cholesterol decreased only after RYGB (p < 0.05). Meal-GLP-1 increased postoperatively in both groups although to a greater extent after RYGB (p < 0.001 vs. SG). GIP decreased after both procedures, especially after RYGB (p = 0.003). At multivariate analysis, GLP-1 peak was the best predictor of LDL reduction (β = −0.552, p = 0.039) while the improvement of HOMA-IR (β = 0.574, p = 0.014) and weight loss (β = 0.418, p = 0.036) predicted triglycerides reduction.
Conclusions
Both surgical procedures markedly reduce fasting and postprandial triglycerides and increase HDL cholesterol levels. LDL cholesterol decreases only after RYGB through a mechanism likely mediated by the restoration of GLP-1.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bariatric surgery (BS) represents an effective means to induce sustained weight loss and to improve metabolic homeostasis in patients with severe obesity and type 2 diabetes (T2DM) [1]. BS is able to induce a marked reduction of fasting triglycerides, with malabsorptive procedures (e.g., biliopancreatic diversion) exerting a more pronounced effect than restrictive procedures (e.g., gastric banding) [2, 3]. With regard to cholesterol, there is evidence that malabsorptive and mixed procedures (e.g., Roux-en-Y gastric bypass) decrease total and LDL cholesterol through a reduction of both synthesis and absorption, whereas restrictive procedures do not affect cholesterol levels [4, 5]. Limited information is available on the impact of BS on postprandial lipid response, which is an important cardiovascular risk factor especially in diabetic patients [6]. We previously demonstrated a 70 % reduction of postprandial triglycerides in obese T2DM patients 2 weeks after either sleeve gastrectomy (SG) or Roux-en-Y gastric bypass (RYGB) [7]. A similar improvement in postprandial TG-rich lipoproteins was observed in diabetic and non-diabetic patients 3 months after SG or RYGB, independently of weight loss [8, 9]. However, little information is available on postprandial lipid changes in the long term, when a stable metabolic and hormonal equilibrium is reached.
There is clinical evidence that pharmacologic activation of the glucagon-like peptide-1 (GLP-1) receptor improves lipid profile in T2DM patients, indicating that GLP-1 has the potential to favorably affect lipid metabolism [10]. Also GIP could contribute to reduce fasting lipid levels through modification of insulin resistance [11]. Whether the changes in GLP-1 and GIP levels consequent to BS directly affect lipid metabolism is still unclear, also because most studies have assessed lipid concentrations only in the fasting state. Therefore, we evaluated the 2-year effects of SG and RYGB on fasting and postprandial lipid profile in obese T2DM subjects and the relation of lipid changes with modifications of incretin levels.
Subjects and Methods
Participants
Nineteen obese T2DM patients were studied. The inclusion criteria were as follows: age 30–65 years, body mass index (BMI) ≥ 40 or ≥ 35 kg/m2 with poor glycemic control under medical treatment, no use of statins or other lipid-lowering agents and eligibility for SG or RYGB. Antidiabetic treatment was oral hypoglycemic agents in 15 patients (9 in SG and 6 in RYGB); 1 patient was treated with insulin; 3 patients (1 in SG and 2 patients in RYGB) were on diet alone; 13 patients (9 in SG and 4 in RYGB) were on antihypertensive drugs (ACE-inhibitors/sartans) (Table 1). No patient was treated with SGLT2 inhibitors and/or thiazide diuretics or other drugs potentially influencing lipid levels. Clinical and metabolic evaluation of participants was conducted at the Department of Clinical Medicine and Surgery of University Federico II while bariatric operations were performed at the Department of Surgery, S. Giovanni Bosco Hospital of Naples. All patients were informed of the risks and benefits of each procedure and provided written informed consent before undergoing surgery. The study was approved by the local Ethics Committee.
Study Design
All operative procedures were performed laparoscopically by the same surgery team [7]. Before and 2 years after surgery, all participants were given a liquid mixed meal (304 kcal, Resource Energy Nestle Nutrition) containing 41 g carbohydrates (55 %), 13 g proteins (18 %), and 9 g fat (27 %). Blood samples, taken fasting and at 30-min intervals for 3 h, were collected in chilled EDTA/Aprotinin tubes, immediately centrifuged, and plasma was stored at −80 ° C for determination of substrates and hormones. At the 2-year follow-up, all patients filled in a 7-day food record to estimate their nutrient intake.
Laboratory Measurements
Cholesterol and triglycerides concentrations were determined by enzymatic-colorimetric methods (ABX Diagnostics, Montpellier, France, Roche Diagnostics, Milan, Italy) on a Cobas Mira autoanalyzer (ABX Diagnostics, Montpellier, France). HDL lipoproteins were separated from plasma by the method of precipitation with phosphotungstic acid/magnesium chloride. LDL cholesterol was calculated by Friedewald formula (no patient had plasma triglycerides > 300 mg/dl). Plasma glucose, insulin, active GLP-1 and GIP concentrations were measured by standard methods, as previously described [7].
Calculations
Homeostasis model assessment of insulin resistance (HOMA-IR) was calculated using the following formula: fasting glucose (mg/dl) × fasting insulin (μU/l)/405. Glucose, insulin, lipid, GLP-1, and GIP responses to the mixed meal were evaluated as the area under the curve above the baseline value (IAUC) for 3 h, calculated with the trapezoidal rule.
Statistical Analysis
Data are expressed as means ± SD unless otherwise stated. Variables not normally distributed were analyzed after logarithmic transformation. Differences were evaluated by t test for paired data within each surgical procedure and by t test for unpaired data between the two surgical procedures. Bivariate associations were assessed by Pearson’s correlation. A multivariate regression analysis was performed to identify which variables best predicted the changes in lipid levels. A p value <0.05 was considered statistically significant. The statistical analysis was performed according to standard methods using the Statistical Package for Social Sciences software (SPSS/PC; SPSS, Chicago, IL). Based on previous reports [4], we estimated that 9 patients in each group were needed to detect a 30 % difference in LDL cholesterol level between the two procedures with a 80 % power at 5 % significance level.
Results
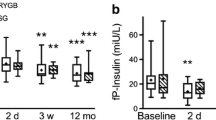
The anthropometric and metabolic parameters of participants before and 2 years after surgery are presented in Table 1. Subjects had similar characteristics at baseline. The diet followed by the patients after intervention was similar in the two groups (Kcal 1390 ± 503 vs 1386 ± 572; Fat% 31 ± 3 vs 35 ± 7; CHO% 53 ± 7 vs 49 ± 9; Protein% 17 ± 5 vs 19 ± 5). After surgery, BMI decreased to the same extent in the two groups. Blood glucose control significantly improved after both procedures with HbA1c reduction of 1.9 % in the SG and 2.3 % in the RYGB group. All patients, except one, discontinued hypoglycemic treatment. Fasting insulin and HOMA-IR were reduced by 2–4-fold with both procedures. Fasting triglycerides markedly decreased while HDL cholesterol increased after either SG or RYGB. In contrast, total and LDL cholesterol decreased significantly by ~25 % after RYGB while they remained unchanged after SG, with a significant difference between the two procedures (p < 0.05). Glucose response to the meal significantly decreased after both procedures (p < 0.05, p < 0.001). A more rapid and sharp increase in insulin concentration was observed after surgery in both groups (p < 0.05) followed by a steeper fall thereafter. However, no difference was found in the insulin IAUC between SG and RYGB (Fig. 1).
Plasma concentration and IAUC of glucose and insulin after a mixed meal before (continuous line and white bar) and 2 years (dotted line and gray bar) after sleeve gastrectomy (SG) or gastric bypass (RYGB). Data are expressed as means (±SEM). *p < 0.05, § p < 0.01 and # p < 0.001, pre- vs post-surgery
Postprandial triglycerides markedly decreased whereas HDL cholesterol increased after both interventions (Fig. 2). Conversely, postprandial LDL cholesterol levels were significantly lower after RYGB compared to SG (p < 0.05). No significant difference was found in the IAUC of triglycerides, HDL, and LDL cholesterol between the two interventions (Fig. 2). GLP-1 meal response, very flat preoperatively, increased after surgery, with a higher increment after RYGB (IAUC 1753 ± 271 vs 256 ± 78 pmol/l × 180 min, p < 0.001). GLP-1 peak was 10 ± 2 pmol/l after SG and 49 ± 6 pmol/l after RYGB (p = 0.001) (Fig. 3). GIP response to the mixed meal markedly decreased after SG (320,951 ± 12,448 vs 21,947 ± 5990 pg/ml, p = 0.007) as well as RYGB (27,177 ± 1460 vs 12,867 ± 5290 pg/ml, p = 0.024), with a greater reduction after RYGB (p = 0. 003) (Fig. 3).
Plasma concentration and IAUC of triglycerides, HDL cholesterol and LDL cholesterol after a mixed meal before (continuous line and white bar) and 2 years (dotted line and gray bar) after sleeve gastrectomy (SG) or gastric bypass (RYGB). Data are expressed as means (±SEM). *p < 0.05, pre- vs post-surgery
The decrease of fasting triglycerides was positively correlated with weight loss (R = 0.470, p = 0.049), reduction of HOMA-IR (R = 0.679, p = 0.001) and reduction of GIP IAUC (R = 0.871, p = 0.005). In the RYGB group, LDL cholesterol was inversely related with GLP-1 peak (R = −0.733, p = 0.007) adjusted for pre-surgery values.
The multivariate model, adjusted for age, gender, duration of T2DM and HbA1c, showed that GLP-1 peak was the best predictor of LDL reduction (β = −0.552, p = 0.039) while reduction of HOMA-IR (β = 0.574, p = 0.014) and weight loss (β = 0.418, p = 0.036) predicted triglycerides improvement.
Discussion
Our study shows that SG and RYGB exert similar effects on body weight, glucose control, fasting, and postprandial triglycerides and HDL cholesterol, whereas total and LDL cholesterol levels were ~30 % lower after RYGB than SG. This difference is likely due to the type of surgery since both quantitative and qualitative dietary intake was similar in the two groups.
This finding is in line with previous studies showing a decrease in total and LDL cholesterol after malabsorptive or mixed surgery, but no change after restrictive procedures [4, 5]. A recent study demonstrated that malabsorptive, but not restrictive, procedures reduce sterol absorption and increase both cholesterol synthesis and catabolism with a net reduction in total and LDL cholesterol levels [4]. Noteworthy, this effect was independent of weight loss and the improvement of glucose metabolism and insulin sensitivity [4, 5], raising the possibility that factors activated by intestinal rearrangement may contribute to cholesterol reduction. The significant inverse correlation between LDL cholesterol and GLP-1 meal response found in our RYGB patients supports the hypothesis that the restoration of GLP-1 may contribute to the reduction of plasma cholesterol level. In experimental animals, GLP-1 is able to suppress hepatic lipogenesis through activation of AMPK pathway [12] and the genes involved in fatty acid β-oxidation [13]. It could be hypothesized that the inverse relation between GLP-1 peak and LDL cholesterol in RYGB group may be due to a common factor, i.e., an increase in circulating bile acids, which is known to occur after RYGB but not after restrictive procedures [14–16]. Bile acids are able to stimulate GLP-1 secretion through the interaction with the TGR5 receptor and, in the meanwhile, affect cholesterol metabolism through an interaction with transcriptional factors (LXR, FXR, and PPARs), as recently reviewed by Moschetta [17].
At odds with a differential effect on cholesterol, RYGB and SG cause a similar reduction of fasting as well as postprandial triglycerides, confirming in the long term the results obtained early after surgery [7]. The reduction of fasting triglycerides is attributable to weight loss and improvement of insulin resistance, whereas the reduction of postprandial triglyceride is likely a consequence of reduced absorption of triglycerides and/or synthesis of chylomicrons. This hypothesis is supported by a recent kinetic study showing a reduced production of VLDL and chylomicron in RYGB and SG patients [18].
The association between changes in GIP levels and triglycerides reduction found in our patients after surgery suggests that the suppression of GIP may play a role in improving triglyceride metabolism [19]. This possibility is supported by previous studies in rodents showing that GIP is able to promote post-meal triglyceride clearance and to increase fat storage by adipocytes [20]. In addition, there is evidence that the disruption of GIP signaling reduces fat accumulation in adipocytes [20] and that GIP receptor knockout mice exhibit an increased insulin sensitivity [21]. Our finding that, in the multivariate model, GIP is no longer associated with triglycerides reduction strongly indicates that its effect is mediated by weight loss and improvement of insulin resistance.
In the long term, both procedures induce a significant increase in HDL cholesterol, confirming previous clinical studies [22].
A limitation of our study is that it was performed in a nonrandomized setting; however, the two groups of patients had similar pre-surgery clinical and metabolic characteristics, making very unlikely the possibility that the differences observed between the two procedures may be attributed to patients’ selection bias. Noteworthy, we elected diabetic subjects who did not take lipid-lowering agents to better appreciate the changes in lipid levels induced by BS without the confounding effect of drug usage.
In conclusion, either RYGB and SG persistently improve glucose metabolism, reduce both fasting and postprandial triglycerides, and increase HDL cholesterol. LDL cholesterol decreases only after RYGB; this effect—likely mediated by surgery-induced GLP-1 restoration—underlines the crucial role of gut in the regulation of lipid metabolism. A longer follow-up period is required to highlight possible differences and changes in the clinical outcome of each procedure.
Abbreviations
- T2DM:
-
Type 2 diabetes
- BS:
-
Bariatric surgery
- GLP-1:
-
Glucagon-like peptide-1
- SG:
-
Sleeve gastrectomy
- RYGB:
-
Roux-en-Y gastric bypass
- HDL:
-
High-density lipoprotein
- LDL:
-
Low-density lipoprotein
- IAUC:
-
Incremental area under curve
- BMI:
-
Body mass index
- HOMA-IR:
-
Homeostasis model assessment-estimated insulin resistance
- GIP:
-
Glucose dependent insulinotropic peptide
References
Yu J, Zhou X, Li L, et al. The long-term effects of bariatric surgery for type 2 diabetes: systematic review and meta-analysis of randomized and non-randomized evidence. Obes Surg. 2015;25(1):143–58.
Moustarah F, Gilbert A, Després JP, et al. Impact of gastrointestinal surgery on cardiometabolic risk. Curr Atheroscler Rep. 2012;4(6):588–96.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;13(14):1724–37.
Benetti A, Del Puppo M, Crosignani A, et al. Cholesterol metabolism after bariatric surgery in grade 3 obesity: differences between malabsorptive and restrictive procedures. Diabetes Care. 2013;36(6):1443–7.
Pihlajamäki J, Grönlund S, Simonen M, et al. Cholesterol absorption decreases after Roux-en-Y gastric bypass but not after gastric banding. Metabolism. 2010;59(6):866–72.
Pirillo A, Norata GD, Catapano AL. Postprandial lipemia as a cardiometabolic risk factor. Curr Med Res Opin. 2014;30(8):1489–503.
Griffo E, Nosso G, Lupoli R, et al. Early improvement of postprandial lipemia after bariatric surgery in obese type 2 diabetic patients. Obes Surg. 2014;24(5):765–70.
Waldmann E, Hüttl TP, Göke B, et al. Effect of sleeve gastrectomy on postprandial lipoprotein metabolism in morbidly obese patients. Lipids Health Dis. 2013;12:82.
Umeda LM, Pereira AZ, Carneiro G, et al. Postprandial adiponectin levels are associated with improvements in postprandial triglycerides after Roux-en-Y gastric bypass in type 2 diabetic patients. Metab Syndr Relat Disord. 2013;11(5):343.
Patel VJ, Joharapurkar AA, Shah GB, et al. Effect of GLP-1 based therapies on diabetic dyslipidemia. Curr Diabetes Rev. 2014;10(4):238–50.
Mells JE, Anania FA. The role of gastrointestinal hormones in hepatic lipid metabolism. Semin Liver Dis. 2013;33(4):343–57.
Ben-Shlomo S, Zvibel I, Shnell M, et al. Glucagon-like peptide-1 reduces hepatic lipogenesis via activation of AMP-activated protein kinase. J Hepatol. 2011;54(6):1214–23.
Svegliati-Baroni G, Saccomanno S, Rychlicki C, et al. Glucagon-like peptide-1 receptor activation stimulates hepatic lipid oxidation and restores hepatic signalling alteration induced by a high-fat diet in nonalcoholic steatohepatitis. Liver Int. 2011;31(9):1285–97.
Nakatani H, Kasama K, Oshiro T, et al. Serum bile acid along with plasma incretins and serum high-molecular weight adiponectin levels are increased after bariatric surgery. Metabolism. 2009;58(10):1400–7.
Kohli R, Bradley D, Setchell KD, et al. Weight loss induced by Roux-en-Y gastric bypass but not laparoscopic adjustable gastric banding increases circulating bile acids. J Clin Endocrinol Metab. 2013;98(4):E708–12.
Patti ME, Houten SM, Bianco AC, et al. Serum bile acids are higher in humans with prior gastric bypass: potential contribution to improved glucose and lipid metabolism. Obesity (Silver Spring). 2009;17(9):1671–7.
Moschetta A. Nuclear receptors and cholesterol metabolism in the intestine. Atheroscler Suppl. 2015;17:9–11.
Padilla N, Maraninchi M, Béliard S, et al. Effects of bariatric surgery on hepatic and intestinal lipoprotein particle metabolism in obese, nondiabetic humans. Arterioscler Thromb Vasc Biol. 2014;34(10):2330–7.
Rao RS, Kini S. GIP and bariatric surgery. Obes Surg. 2011;21(2):244–52.
Miyawaki K, Yamada Y, Ban N, et al. Inhibition of gastric inhibitory polypeptide signaling prevents obesity. Nat Med. 2002;8(7):738–42.
Miyawaki K, Yamada Y, Yano H, et al. Glucose intolerance caused by a defect in the enteroinsular axis: a study in gastric inhibitory polypeptide receptor knockout mice. Proc Natl Acad Sci U S A. 1999;96(26):14843–7.
Brethauer SA, Aminian A, Romero-Talamás H, et al. Can diabetes be surgically cured?: Long-term metabolic effects of bariatric surgery in obese patients with type 2 diabetes mellitus. Ann Surg. 2013;258(4):628–37.
Acknowledgments
The authors thank Giuliana Vitolo for the dietary counseling.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of Interest
The authors declare that they have no competing interests.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Griffo, E., Cotugno, M., Nosso, G. et al. Effects of Sleeve Gastrectomy and Gastric Bypass on Postprandial Lipid Profile in Obese Type 2 Diabetic Patients: a 2-Year Follow-up. OBES SURG 26, 1247–1253 (2016). https://doi.org/10.1007/s11695-015-1891-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-015-1891-4