Abstract
Background
Laparoscopic sleeve gastrectomy (LSG) is currently being widely accepted for its role in the treatment of morbid obesity. Staple-line leakage is one of the most reported complications found in 0.5–7 % of the population, in which the Over-the-Scope Clip (OTSC) (Ovesco Endoscopy, Tübingen, Germany), a novel device, is employed. We present our experience with this system in LSG leaks.
Methods
A retrospective analysis of prospectively collected data from patients with LSG leakage was performed, and these patients were treated with the OTSC system. Efficiency was defined as complete oral nutrition without any evidence of additional leakage.
Results
Overall, 26 patients underwent endoscopic OTSC treatment. The median age was 39 years (range 26–60), and 12 were male patients (46.15 %). The mean body mass index (BMI) was 42.89 kg/m2, and 10 patients (38.46 %) came from a revisional bariatric procedure (SRVG or LAGB). Twenty-two patients (84.61 %) had upper staple-line leaks (near the GEJ), and the remaining 4 (15.38 %) had lower antral leaks.
Number of endoscopy sessions ranged from 2 to 7 (median 3). There were five failures: 2 of them had an antral leak, and the remaining 3 had an upper staple-line leak. Twenty-one (80.76 %) leaks were successfully treated within 32 days’ median time till complete oral nutrition was attained (range 14–70).
Conclusions
The success rate was high with the OTSC system, and it is concluded to be a safe and effective treatment for LSG leaks.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Introduction
Sleeve gastrectomy is a widely accepted modality for the treatment of morbid obesity (with or without comorbidities) [1]. This popular procedure has its own complications. Among them, staple-line leakage is currently the most reported complication (0.5–7 %) [2–4]. This complication is due to the long staple line with its increased intragastric pressure [5]. Various attempts at treating this complication have been in practice, from medical observation to surgical and endoscopic management . If not treated promptly, this complication may lead to serious adverse events such as the appearance of intra-abdominal abscesses, sepsis, and even mortality [6, 7]. Currently, endoscopic procedures are one of the hallmarks of therapy. Recent advances in interventional endoscopy have brought forward a whole new area of bariatric endoscopy.
One of the novel devices used to treat this complication is the Over-the-Scope Clip (OTSC) (Ovesco Endoscopy, Tübingen, Germany) [8]. Only limited data have been published related to the clinical outcome of the application of the OTSC system for different leaks. We present our experience with this system in treating sleeve gastrectomy leaks.
Methods
We examined the medical records and imaging studies of all patients diagnosed with sleeve leakage and treated with the OTSC system who were referred by surgeons from various medical centers to the Bariatric Gastroenterology service. A retrospective chart review was performed encompassing the period from January 2010 to September 2014.
The data analyzed were age, sex, location of the leak, history of chronic diseases, previous bariatric surgery time between operation, fistula diagnosis, and endoscopic over-the-scope clip (OTSC) procedure. Additional treatment, complications, and efficiency as stated by full oral nutrition with no additional leakage symptoms were noted. Follow-ups were continued until the complication resolved.
All fistulas were visualized during the endoscopic procedure. All patients initially received parenteral nutrition. Patients with intra-abdominal collections were initially drained.
Leaks that were assessed as large (as compared with the scope diameter) were primarily debrided, and these patients were scheduled for a follow-up endoscopy a few weeks later. Each case was individually managed according to the clinical parameters, the amount of fluid in the drains, imaging, and after joint consultation with the surgeon.
This type of clip is loaded at the end of the scope and released by a technique using a thread and spool as band ligation. The leak site is centered and suctioned into a “cap” followed by a release of the clip.
Efficiency was defined as complete oral nutrition without any evidence of additional leakage.
Results
A total of 26 patients with post-LSG leaks received endoscopic OTSC treatment. The median age was 39 years (range 26–60), and 12 were male patients (46.15 %). The mean body mass index (BMI) was 42.89 kg/m2.
Overall, 16 (61.53 %) patients underwent primary sleeve gastrectomy, and 10 (38.46 %) came from a revisional bariatric procedure (SRVG or LAGB). Twenty-two (84.61 %) of the patients had upper staple-line leaks (near the GEJ), and the remaining 4 (15.38 %) had lower antral leaks.
The leak in 5 patients was diagnosed after performing a routine contrast study and before their release from the ward. In another 4 patients, the drain showed increased gastric secretions that led to the diagnosis of the leak. The remaining 16 patients presented with clinical symptoms: 3 with only tachycardia, 4 with only fever, 3 with fever and abdominal pain, 2 with fever and intra-abdominal collections, 3 with abdominal pain and intra-abdominal fluid collection, 1 with recurrent pneumonia and a subdiaphragmatic abscess, and 1 who presented to the emergency room with septic shock. Leaks were diagnosed at a median of 8 days (range, 2–240 days) postoperatively: 6 (23.07 %) early (in 0–4 days), 13 (50 %) intermediately (in 5–9 days), and 7 (20.83 %) late (after day 10) (Table 1).
At least half of the patients had hypertension and/or diabetes and/or disturbed lipid profile at the time of pre-operative screening. Obstructive sleep apnea (OSA) was present in 5 patients (19.23 %).
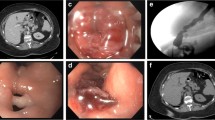
The number of endoscopy sessions ranged from 2 to 7 (median 3). Seven (26.92 %) patients underwent additional endoscopic treatment: stent insertion; biological glue at another center before referral to our center; and in another patient, a plastic biliary prosthesis was inserted before the OTSC procedure. Twenty-one of the patients underwent a single-clip placement, and the other 5 had two clips placed. Figure 1 shows an endoscopic view of the clip placement, and Fig. 2 shows the OVESCO clip with a stent.
All endoscopic procedures with clip placement were without complications. There were five failures: two of them were antral leaks, and the remaining 3 were upper staple-line leaks. Twenty-one leaks were successfully treated (80.76 %) within 30 days’ median time till complete oral nutrition was attained (range 14–70).
Discussion
Sleeve gastrectomy is one of the widely used options for the management of morbid obesity (with or without comorbidities). This approach does not come without its complications. Staple-line leakage is widely reported to be ranging from 0.57 to 24 % [4]. Although numerous therapeutic options have been described in the literature, many of them utilize the endoscopic approach, such as stent insertion (biliary or bariatric), clips, and biologic glue [9–12].
This study comprises our experience with 26 cases with the use of the OTSC system for leaks after sleeve gastrectomy, which is the largest series to date. This type of clip has dramatically increased the possibilities of endoscopic defect closure compared with Through-The-Scope Clips (TTSC). Not many reports have been published about the use of this type of clip. Post-LSG, 11 cases were reported by Surace et al., 18 cases by Mercky et al., and 2 additional successful case reports [13–15].
We reported a high success rate among 21 of the 26 patients (80.76 %). The others also reported high success rates, that is, 90.9 and 88.9 % [13, 14]. An additional report of 9 cases from an International multicenter series, with an over-the-scope clipping on different types of leaks, reported a 73.3 % success rate. [16] Since low-volume centers report an overall lower success rate, it is evident that the treatment efficiency is operator dependent. Patients from different centers around the country as well as 3 patients from neighboring countries were referred for treatment.
Nonsurgical management of gastrointestinal perforation and fistulas had also been attempted using various such as different clips and stents devices, with a success rate between 55 and 69 %, often necessitating additional surgical management [17, 18].
Leaks have been classified based on the period for which they appear: early, between first and fourth day post-op; intermediate, between the fifth and ninth day after surgery; and late, appearing after day 10. [19, 20]. Most of the leaks treated were early or intermediate, and among the late leaks, the clip efficiently closed in 6 out of the 7 cases, with the last, very prolonged case being fibrotic and resistant to treatment.
In our unit, endoscopy was initially performed to assess the size of the leakage. We aimed at all initial endoscopies being performed with a bariatric surgeon in the room. The leak orifice after sleeve gastrectomy may be diagnosed at the time of the procedure itself. As previously reported by Surace et al., we also found that clip placement was more successful when no evidence of infection behind the orifice of the leak was seen by normal CRP, ESR, and WBC levels, and no post-orifice fluid collections were seen by CT imaging [13]. Afterward, we often initially performed debridement of the orifice. There was no need to center the edges of the fistula, except for thrice with the OTSC anchor, and simple biopsy forceps were used for an additional 4 cases. Clip placement, at times, led to a gradual decrease in the amount of fluid in the drains, a trend that continued until complete cessation of fluids and initiation of complete oral nutrition, and with it there was cessation of parenteral feeding.
The Over-the-Scope Clip system (Ovesco, Tubingen, Germany) has shown efficacy in the management of severe bleeding and perforations of the gastrointestinal tract [21, 22]. This relatively new device provides more strength and better tissue capture. The clip is attached to the endoscope tip, and its release technique is similar to band ligation [23]. The leak site orifice can be suctioned inside the cap or gripped with a Twin Grasper or simple biopsy forceps [24].
The role of the OTSC in bariatric endoscopy has been increasing steadily; it has been used to treat fistulas, deep wall defects, and perforations after endoscopic procedures [25, 26]. One of its main advantages, shown in the colon, is providing a full-thickness closure and a comparable efficiency to manual surgical suture [27]. Recently, a case report was published on successful closure of a giant gastrogastric fistula after gastric bypass surgery, which took place after unsuccessful revisional surgery [28].
There were 4 patients with antral leakages. Although the number of antral leakages was small, the success rate was only 50 %. These leakages are difficult to treat and require recurrent multi-modality endoscopic treatments, with less success rates.
To our knowledge, this case study series is the largest presented to date with a final closure rate of 80.76 %. Repeated endoscopies are often necessary, and the bariatric team should not be discouraged by the initial findings.
There are a number of endoscopic treatment options, and effective treatment requires patience and teamwork between the bariatric surgeon and bariatric endoscopist, having the surgeon present at the time of endoscopy and together deciding in a case-by-case manner as to what is the best thing to do.
In conclusion, we present our experience with the OTSC system. The rate of success with fistula closure was high, and it proves, with appropriate indications, to be a safe and effective treatment for leaks after sleeve gastrectomy.
References
Silecchia G, Boru C, Pecchia A, et al. Effectiveness of laparoscopic sleeve gastrectomy (first stage of biliopancreatic diversion with duodenal switch) on co-morbidities in super-obese high-risk patients. Obes Surg. 2006;16(9):1138–44.
Baltasar A, Serra C, Perez N, et al. Laparoscopic sleeve gastrectomy: a multi-purpose bariatric operation. Obes Surg. 2005;15:1124–8.
Jurowich C, Thalheimer A, Seyfried F, et al. Gastric leakage after sleeve gastrectomy—clinical presentation and therapeutic options. Langenbecks Arch Surg. 2011;396(7):981–7.
Surgery, Clinical Issues Committee of the American Society for Metabolic and Bariatric Surgery. Updated position statement on sleeve gastrectomy as a bariatric procedure. Surg Obes Relat Dis. 2010;6(1):1–5.
Moszkowicz D, Arienzo R, Khettab I, et al. Sleeve gastrectomy severe complications: is it always a reasonable surgical option? Obes Surg. 2013;23(5):676–86.
Sakran N, Goitein D, Raziel A, et al. Gastric leaks after sleeve gastrectomy: a multicenter experience with 2,834 patients. Surg Endosc. 2013;27(1):240–5.
Burgos AM, Braghetto I, Csendes A, et al. Gastric leak after laparoscopic-sleeve gastrectomy for obesity. Obes Surg. 2009;19(12):1672–7.
Kirschniak A, Kratt T, Stüker D, et al. A new endoscopic over-the-scope clip system for treatment of lesions and bleeding in the GI tract: first clinical experiences. Gastrointest Endosc. 2007;66:162–7.
Huang CS, Hess DT, Lichtenstein DR. Successful endoscopic management of postoperative GI fistula with fibrin glue injection: report of two cases. Gastrointest Endosc. 2004;60(3):460–3.
Choi HJ, Lee BI, Kim JJ, et al. The temporary placement of covered self-expandable metal stents to seal various gastrointestinal leaks after surgery. Gut Liver. 2013;7(1):112–5.
Romagnuolo J. Endoscopic clips: past, present and future. Can J Gastroenterol. 2009;23(3):158–60.
Slim R, Smayra T, Chakhtoura G, et al. Endoscopic stenting of gastric staple line leak following sleeve gastrectomy. Obes Surg. 2013;23(11):1942–5.
Surace M, Mercky P, Demarquay JF, et al. Endoscopic management of GI fistulae with the over-the-scope clip system (with video). Gastrointest Endosc. 2011;74(6):1416–9.
Mercky P, Gonzalez JM, Aimore Bonin E, et al. Usefulness of over-the-scope clipping system for closing digestive fistulas. Dig Endosc, 2014.
Aly A, Lim HK. The use of over-the-scope clip (OTSC) device for sleeve gastrectomy leak. J Gastrointest Surg. 2013;17(3):606–8.
Haito-Chavez Y, Law JK, Kratt T, et al. International multicenter experience with an over-the-scope clipping device for endoscopic management of GI defects (with video). Gastrointest Endosc, 2014.
Trecca A, Gaj F, Gagliardi G. Our experience with endoscopic repair of large colonoscopic perforations and review of the literature. Technol Coloproctol. 2008;12:315–21.
Blackmon SH, Santora R, Schwarz P, et al. Utility of removable esophageal covered self-expanding metal stents for leak and for fistula management. Ann Thorac Surg. 2010;89(3):931–6.
Márquez MF, Ayza MF, Lozano RB, et al. Gastric leak after laparoscopic sleeve gastrectomy. Obes Surg. 2010;20(9):1306–11.
Csendes A, Braghetto I, León P, et al. Management of leaks after laparoscopic sleeve gastrectomy in patients with obesity. J Gastrointest Surg. 2010;14(9):1343–8.
Kirschniak A, Kratt T, Stüker D. A new endoscopic over-the-scope clip system for treatment of lesions and bleeding in the GI tract: first clinical experiences. Gastrointest Endosc. 2007;66:162–7.
Kratt T, Küper M, Traub F, et al. Feasibility study for secure closure of natural orificetransluminal endoscopic surgery gastrotransluminal endoscopic surgery gastrotomies by using over-the-scope clips. Gastrointest Endosc. 2008;68:993–6.
Parodi A, Repici A, Pedroni A, et al. Endoscopic management of GI perforations with a new over-the-scope clip device (with videos). Gastrointest Endosc. 2010;72:881–6.
Zhang XL, Qu JH, Sun G, et al. Feasibility study of secure closure of gastric fundus perforation using over-the-scope clips in a dog model. J Gastroenterol Hepatol. 2012;27:1200–4.
Repici A, Arezzo A, De Caro G, et al. Clinical experience with a new endoscopic over-the-scope clip system for use in the GI tract. Dig Liver Dis. 2009;41:406–10.
von Renteln D, Denzer UW, Schachschal G, et al. Endoscopic closure of GI fistulae by using an over-the-scope clip (with videos). Gastrointest Endosc. 2010;72:1289–96.
Díez-Redondo P, Blanco JI, Lorenzo-Pelayo S, et al. A novel system for endoscopic closure of iatrogenic colon perforations using the Ovesco® clip and omental patch. Rev Esp Enferm Dig. 2012;104(10):550–2.
Donatelli G, Vergeau BM, Dumont JL, et al. Late presentation of a giant gastrogastric fistula following gastric bypass, treated with a colic over-the-scope clip after unsuccessful surgical repair. Endoscopy. 2014;46(S 01):E128–9.
Conflict of Interest Disclosure Statement
Dr. Dean Keren has completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declares no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; and no other relationships or activities which could appear to have influenced the submitted work.
Dr. Ori Eyal has completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declares no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; and no other relationships or activities which could appear to have influenced the submitted work.
Dr. Gideon Sroka has completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declares no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; and no other relationships or activities which could appear to have influenced the submitted work.
Dr. Tova Rainis has completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declares no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; and no other relationships or activities which could appear to have influenced the submitted work.
Dr. Asnat Raziel has completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declares no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; and no other relationships or activities which could appear to have influenced the submitted work.
Dr. Nasser Sakran has completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declares no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; and no other relationships or activities which could appear to have influenced the submitted work.
Dr. David Goitein has completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declares no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; and no other relationships or activities which could appear to have influenced the submitted work.
Dr. Ibrahim Matter has completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declares no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; and no other relationships or activities which could appear to have influenced the submitted work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Keren, D., Eyal, O., Sroka, G. et al. Over-the-Scope Clip (OTSC) System for Sleeve Gastrectomy Leaks. OBES SURG 25, 1358–1363 (2015). https://doi.org/10.1007/s11695-014-1540-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-014-1540-3