Abstract
Background
We have investigated the differences between metabolically “healthy” morbidly obese patients and those with comorbidities.
Materials and Methods
Thirty-two morbidly obese patients were divided by the absence (“healthy”: DM−DL−) or presence of comorbidities (dyslipidemic: DM−DL+, or dyslipidemic and with type 2 diabetes: DM+DL+). We have studied various plasma parameters and gene expression adipose tissue, before and after gastric bypass.
Results
The group DM+DL+ tends to have lower values than the other two groups for anthropometric parameters. Regarding the satiety parameters, only leptin (p = 0.0024) showed a significant increase with comorbidities. Lipid parameters showed significant differences among groups, except for phospholipids and NEFA. For insulin resistance parameters, only glucose (p < 0.0001) was higher in DM+DL+ patients, but not insulin or homeostasis model assessment of insulin resistance (HOMA-IR). The gene expression of adiponectin, insulin receptor (INSR) and glucose receptor-4 (GLUT4), in the subcutaneous fat, decreased in all groups vs. a non-obese control. Interleukin-6 (IL6) and the inhibitor of plasminogen activator type 1 (PAI-1) genes decreased only in DM−DL+ and DM+DL+, but not in “healthy” patients. Leptin increased in all groups vs. the non-obese control. The visceral fat from DM+DL+ patients showed a sharp decrease in adiponectin, GLUT4, IL6 and PAI-1. All parameters mentioned above improved very significantly by surgery, independent of the occurrence of comorbidities.
Conclusions
The morbidly obese “healthy” individual is not really metabolically healthy, but morbidly obese individuals with diabetes and dyslipidemia are more metabolically imbalanced.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
For the last decade, scientists have been trying to find the mechanism that causes some obese people to develop insulin resistance and type 2 diabetes mellitus (DM), while others with the same BMI remain “healthy” and do not develop these comorbidities [1–3]. Generally, metabolically “healthy” obesity describes the absence of any cardio-metabolic disease—specifically, DM, dyslipidemia (DL) or hypertension (HTA)—in an individual with BMI ≥ 30 kg/m2. The discordance in the definition is a possible reason for the inconsistencies in the prevalence of metabolic normality reported in the literature [4]. It is interesting to note that the prevalence of metabolic normality, defined as the absence of an overt pathology such as DM, HTA or DL, declined from 85 % in normal-body-weight subjects to 46–48 % in obese individuals and 23 % in morbidly obese individuals, thus suggesting that an increased body mass index drastically reduces the chances of being metabolically normal [4].
Our hypothesis is that in the morbidly obese, it is difficult, or impossible, to consider “healthy” obese patients.
In the present study, we have investigated the differences among morbidly obese individuals, who were “healthy” or dyslipidemic, or dyslipidemic and diabetic, before and 1, 6 and 12 months after Roux-en-Y gastric bypass (RYGBP). First, we established the anthropometric parameters, satiety factors (leptin, ghrelin and adiponectin), the lipid and insulin profiles and inflammation parameters in all patients. Second, we examined the mRNA gene-expression profiles for some inflammatory factors, such as interleukin-6 (IL-6), TNF-α and plasminogen activator type 1 (PAI-1); some satiety factors, such as leptin and adiponectin; and some parameters related to DM, such as the insulin receptor and glucose receptor-4 (GLUT4). Third, we focused on how HTA and BMI affect these factors in each group of morbidly obese patients.
Materials and Methods
Patient Selection
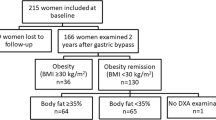
A group of 32 morbidly obese patients (23 women and 9 men) aged between 21 and 61 years who underwent RYGBP surgery were enrolled and followed up at the Hospital de la Vall d’Hebron in Barcelona, Catalonia, as described elsewhere [5, 6]. Subjects presented the necessary indications for bariatric surgery: BMI > 40 kg/m2 or greater than 35 kg/m2 with at least one comorbidity (including HTA, Type 2 diabetes mellitus (DM), dyslipidemia (DL), obstructive sleep apnoea or weight-induced rheumatologic disease). The diagnostic criteria used for DM, HTA or DL were according to the National Cholesterol Education Program [7] and the European Society of Cardiology [8].
Patients were considered to be “healthy” morbidly obese patients when we apply the most restrictive criteria of Wildman et al. [9]. Thus for DM, the threshold was for fasting plasma glucose ≥100 mg/dL or medically diagnosed DM; the criteria for HTA was systolic and diastolic blood pressure (SBP and DBP, respectively), SBP ≥130 mmHg and DBP ≥85 mmHg, and the criteria for DL was TG ≥150 mg/dL, cLDL ≥110 mg/dL and cHDL <40 and 50 mg/dL for men and women, respectively, or medically diagnosed DL.
According to those criteria, the patients were divided into three groups as follows: 10 patients were DM−DL− (the “healthy” obese group, without type 2 diabetes mellitus (DM−) or dyslipidemia (DL−), comprising 6 women and 4 men), 15 patients were DM−DL+ (the obese group with dyslipidemia, comprising 11 women and 4 men), and 7 patients were DM+DL+ (the obese group with dyslipidemia and diabetes, consisting of 6 women and 1 man). Regarding hypertension, 2 patients were hypertensive in the first group, 4 patients in the second and all in the third group.
Blood samples were taken under fasting conditions between 8:00 a.m. and 10:00 a.m., at the time of surgery (OB in Tables and Graphs) and 1, 6 and 12 months after gastric bypass surgery. Plasma was separated immediately by centrifugation, and aliquots were frozen at −80 °C for subsequent analysis. In obese subjects, subcutaneous abdominal adipose tissue (SAT) and visceral adipose tissue (VAT) biopsies were performed during RYGBP. Second and third SAT biopsies were obtained at 6 and 12 months after bariatric surgery, respectively. The anaesthetic procedure was standardised for elective surgery and for the biopsy procedures (1 % Scandicain was used). Epinephrine was not used. Tissue samples were quickly minced, frozen in liquid nitrogen and stored at −80 °C until further analysis.
For the control group (supplemental data Table S1), we used 23 euthyroid, normal-weighted, normotensive, and non-diabetic patients (12-h fasting) who underwent elective cholecystectomy at the same time the blood was drawn, and a subcutaneous abdominal and visceral adipose tissue biopsy was performed in only seven of the patients.
The study protocol was reviewed and accepted by the hospital ethics committee conforming to the Declaration of Helsinki, and all subjects gave their written informed consent to participate.
Anthropometric and Body Composition Measurements
Body weight and waist and hip circumferences were measured according to standardised procedures [10]. The body fat percentage, the amount of total, subcutaneous and visceral fat, was calculated as described previously [11].
Plasma Biochemistry Assays
Leptin, ghrelin, adiponectin, insulin, homeostasis model assessment of insulin resistance (HOMA-IR), C-reactive protein (CRP) and PAI-1 were measured as described previously [6, 11].
The levels of fasting plasma glucose, triacylglycerides (TAGs), non-esterified fatty acids (NEFAs), total cholesterol (TC), and high- and low-density lipoprotein cholesterol (cHDL and cLDL, respectively) were measured enzymatically in the routine chemistry laboratory at the hospital. The plasma concentrations of apoA1 and apoB were measured using a turbidimetric method based on that described by Marcovina and Alberts [12].
Total RNA, cDNA Preparation and PCR Analysis
The total RNA from 70 mg of human adipose tissue biopsies (subcutaneous and visceral) was extracted with Tripure Isolation Reagent (Roche, USA). First-strand complementary DNA (cDNA) was synthesised from 0.4 μg of total RNA using random primers and TaqMan high-capacity cDNA reverse transcription reagents (Applied Biosystems, USA). Relative mRNA levels were evaluated using the ΔΔCt method. Leptin, adiponectin, insulin receptor (INSR), glucose receptor 4 (GLUT4) IL-6, TNF-α and activator of inhibitor of plasminogen type 1 (PAI-1) genes were measured.
Statistical Analysis
The results are reported as the means ± SEM. Significant differences between mean values for obese (OB) and 1, 6, or 12 months after surgery (weight loss) were assessed using non-parametric Kruskal-Wallis test, and individual comparisons were made using Dunn’s post-test. Significant differences between healthy morbidly obese (DM−DL−), dyslipidemic (DM−DL+) and diabetic and dyslipidemic (DM+DL+) individuals at different times after surgery (weight loss effect) were assessed by a two-way ANOVA (comorbidities and surgery effect, respectively) and Bonferroni post-tests. The same test was used to establish significant differences between the DM−DL−, DM−DL+ and DM+DL+ groups with different BMIs or HTA (comorbidities and BMI or an HTA effect, respectively). The level of significance was adjusted for multiple comparisons (Bonferroni correction/adjustment procedure), and the results were considered significant at p < 0.01.
All statistical analyses were computed using GraphPad Prism version 5.0 software for Windows (GraphPad Software, San Diego CA, USA, www.graphpad.com).
Results
Anthropometric and Satiety Parameters
Strikingly, for almost all parameters studied, the group DM+DL+ tends to have lower values than the other two groups. As mentioned above, all patients were morbidly obese, and it is therefore logical that the BMI is not affected by comorbidities (Table 1), except the body weight (p = 0.0004) which decreased in DM+DL+. Surgery had a very significant effect on all the parameters measured (Table 1), both globally and in each different group.
The parameters related to satiety are shown in Table 1. Ghrelin (2.5 times in the DM−DL+ group) and adiponectin (two times in the “healthy” group) levels progressively increase after surgery if comorbidities are present, whereas leptin was significantly lower in all groups (5.5 times in the “healthy” group, 4.1 times in the DM−DL+ group, and 5.3 times in the DM+DL+ group).
Lipid Parameters
We observed highly significant changes for all lipid parameters due to both comorbidities and surgery (Table 2) except for PL and NEFAs. For TGs, the TC, cLDL, cHDL, apoA1 and apoB levels were significantly different not only within each group of patients as a result of surgery but also between groups with and without comorbidities. It should also be noted that lipid levels were similar in the DM−DL+ and DM+DL+ groups and always slightly higher than in the “healthy” group. As can be observed for all parameters within all groups, there was a decrease 1 month after surgery that was often significant (Table 2).
Insulin Resistance Parameters
Although the various groups were selected according to DM status, insulin levels were similar in all groups (Table 3), whereas glucose was significantly different in the DM+DL+ group compared to either the DM−DL− (p < 0.001) group, which is logical, or the DM−DL+ group (p < 0.01) (Table 3). The HOMA-IR [13] clearly indicates that DM+DL+ patients are insulin resistant because the value is almost twice that of patients in the group with only DM−DL+. However, the “healthy” obese group had some insulin resistance because their HOMA-IR values were even higher than for the patients in the DM−DL+ group. Only glucose was affected by comorbidities. However, all of the above parameters were affected by surgery (Table 3).
Inflammation Parameters
CRP, a marker of inflammation, indicated that there were differences both from comorbidities (p = 0.0041) and surgery (p < 0.0001). PAI-1 was affected by bariatric surgery (p < 0.0001), but not by comorbidities (Table 3).
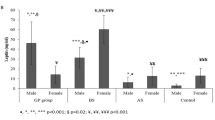
Gene Expression
The gene expression of adiponectin, insulin receptor (INSR) and glucose receptor-4 (GLUT4), in the subcutaneous fat (Table 4), decreased in all groups vs. control patients. Interleukin-6 (IL6) and the inhibitor of plasminogen activator type 1 (PAI-1) genes only decreased in DM−DL+ and DM+DL+, but not in “healthy” patients. Leptin increased in all groups vs. non-obese patients. The visceral fat (Table 5) from DM+DL+ patients showed a sharp decrease in adiponectin (50 % vs. control), GLUT4 (75 % vs. control), IL6 and PAI-1. All parameters mentioned above improved very significantly after surgery, independent of the absence or presence of comorbidities.
Hypertension Effects on Different Parameters
Although the number of patients without hypertension (Table 6) only includes two patients in the DM−DL− group, four in the DM−DL+ group and none from the DM+DL+ group, as mentioned in the “Materials and Methods” section, Table 6 shows the values of the various parameters in patients distributed by groups with/without hypertension (HTA). Obviously, the groups differ in blood pressure, as indicated by the ANOVA-2 (SBP, p = 0.0052 and DBP, p = ns). The difference in visceral fat is slightly lower in patients without hypertension. A notable difference is observed in the lipid parameters (TC, cLDL and apoB) and those related to diabetes (insulin, glucose and HOMA-IR), although none of the differences were significant. In all cases, the values were slightly lower in the groups with DL (DM−DL+) but without HTA. These changes were also observed for CRP and PAI-1.
BMI Effects on Different Parameters
The different parameters were separated according to BMI and comorbidities (supplemental data Tables S2, S3 and S4), and significant differences with respect to BMI are observed for all anthropometric parameters (except BW and VAT) in addition to cLDL. There is also a significant effect of comorbidity on apoB and glucose. The trend observed for many parameters is to increase with increasing comorbidity and BMI, with the exception of DM+DL+ individuals with a BMI >50, in which it seems that many of the studied parameters tend to slightly decrease.
Discussion
To conduct this study, we used the criteria mentioned in the “Materials and Methods” section to divide patients into three groups according to diagnoses of hyperlipidemia and/or diabetes, whereas patients were considered “healthy” if they did not present any of these comorbidities. Therefore, if we apply the criteria used to define metabolic health status proposed by Aguilar-Salinas [14], Karelis [15], Meigs [16] or Wildman (the most restrictive) [17] or in the work of Phillips and Perry [18], our “healthy” patients mentioned in the previous paragraph are really “healthy” morbidly obese patients.
Anthropometric and Satiety Parameters
Based on the anthropometric data observed in the three groups, it is possible that they have what Tchernof and Despres [19] call a “hypertriglyceridemic waist”, which is a simple clinical phenotype predictive of excess visceral fat and metabolic abnormalities associated with elevated insulin and glucose and an altered lipid profile. From that point of view, none of our groups are “healthy obese”. Brochu et al. [20] reported that reduced visceral fat accumulation, even in the presence of a large amount of total body fat, is a characteristic of “healthy obese” individuals and that this contributes to a protective effect against metabolic abnormalities. Our results do not agree with those reported by Shin et al. [21], most likely because the BMIs of the healthy and unhealthy patients in their study were lower (25 to 27 kg/m2) than those in our study (>40) and are therefore not comparable.
However, we found the greatest differences between the three groups in our study in the leptin, ghrelin and adiponectin levels. Our data for leptin contrasted with those observed by other authors although the data are conflicting; for instance, in some cases, leptin is lower in the unhealthy obese [14, 15], while in other cases, it is higher [16, 17]. In a previous study [6], we observed that the morbidly obese tend to have higher adiponectin levels after bariatric surgery, and a year after surgery, they reach the values of lean individuals without reaching the levels described by Phillips et al. [18]. The three groups of obese patients in our study had adiponectin values within the range reported by other authors for metabolically healthy patients but for patients with a BMI of 20 to 24.9 kg/m2 [14].
Lipid Parameters
We identified marked differences in the lipid parameters, and this could be precisely the key that differentiates the “healthy” and unhealthy obese. Obviously, unhealthy patients are all dyslipidemic, and all parameters are higher than in “healthy” individuals. Other authors have observed changes in TG and cHDL in healthy and unhealthy morbidly obese individuals [14].
Insulin Resistance Parameters
When we compared the HOMA-IR values, all three groups were insulin resistant; in the “healthy” obese, the value was 6.9, and the values were 5.7 (in DM−DL+) and 10.2 (in DM+DL+). The expression of the insulin receptor gene in SAT is clearly affected by comorbidity but not by surgery, being slightly higher for DL+DM+ patients. However, no changes were observed in VAT. Other authors have reported an increase in the expression of the insulin receptor gene in the VAT of morbidly obese individuals, which allows them not to be insulin resistant compared to insulin-resistant or thin individuals [22]. The expression of the GLUT4 gene in SAT does not change as a function of comorbidity but is affected by surgery; however, its expression in VAT tends to decrease with comorbidity. A noteworthy finding for insulin is that 1 year after bariatric surgery, its concentration decreased by 60–70 % compared to obese patients, independently of whether the patient was diabetic or “healthy”; whereas in the same period, adiponectin increased by 65 % compared to obese individuals with diabetes and by up to 100 % if the patient was “healthy”.
Low levels of adiponectin have been described in DM, cardiovascular disease, hypertension, metabolic syndrome [23] and obesity [24, 25], although the mechanism that regulates it is still unknown. Adiponectin has antidiabetic, antihypertensive and antiatherogenic properties, and recent studies revealed that this protein also has an anti-inflammatory and anti-oncogenic function [26].
Some authors have reported that a weight loss of approximately 10 % is enough for changes in plasma concentrations of adiponectin to occur [27]. Our patients achieved weight loss on the month of the intervention, but adiponectin levels were still low. In our case, changes in the concentration of adiponectin were not obvious until the weight loss was approximately 30 % (6 months post-surgery).
Data on adiponectin expression in relation to AT depot differences are conflicting [28, 29] even if increased adiponectin mRNA levels have been found in VAT vs. SAT in animal models [29, 30]. In the current study, the mRNA as well as the protein expression of adiponectin and its two receptors did not differ between VAT and SAT in severely obese patients [31].
Obesity causes an increase in fat mass but a paradoxical decrease in circulating adiponectin which can lead to insulin resistance, blood vessel dysfunction and hypertension [24].
Parameters of Inflammation
Despite the very slight differences observed between groups in plasma CRP, none stand out. In the case of PAI-1, we observed no differences in the plasma levels, but we observed higher gene expression in “healthy” patients, less in the DM−DL+ group and even less in the DM+DL+ group. Aguilar-Salinas et al. [14] also did not observe significant changes for the plasma CRP or for PAI-1 between “healthy” and unhealthy individuals, whereas others observed changes in the CRP but not in PAI-1 [16] and still others observed significant differences for both parameters [15, 17].
For the other parameters that trigger inflammation, such as IL-6 and TNF-α, we observed no significant differences between the “healthy” group and those with comorbidities; however, a slight tendency for IL-6 to be higher in the “healthy” individuals was observed. There is also controversy regarding IL-6, for which Karelis et al. [15] showed no differences between “healthy” and unhealthy individuals, whereas other authors did observe differences [17]. The same is true for TNF-α for which some authors observed differences [17] while others did not [14]. Another group observed no differences in the levels of TNF-α in patient with and without insulin resistance when corrected for BMI [32]. Our data contrast with those reported by other authors who observed a decrease in the values of CRP, IL-6 and TNF-α in obese healthy patients compared to unhealthy individuals [18]. Other authors observed no differences in either plasma CRP or in the expression of TNF-α or IL-6 in the morbidly obese with high insulin resistance [22].
Thus, according to our hypothesis, morbidly obese patients also have numerous healthy altered plasma parameters, although less so than in the other two groups. Gene expression in the SAT follows the same trend as the corresponding plasma protein. All obese patients, whether healthy or not, have altered leptin (increased), adiponectin, the INSR and GLUT4 (decreased). From the data obtained in our study, healthy obese patients have more altered gene expression than control patients of normal weight and the impairment increases with increasing comorbidity, up to the maximum observed in diabetic patients. Our results are consistent with the idea that the SAT is the major source of leptin [33] and adiponectin [34], while VAT releases more proinflammatory cytokines (TNF-α, CRP, IL6 or PAI-1) [35], which, in our case, was only true for PAI-1 in healthy patients or with dyslipidemia, but not for diabetics or for the other cytokines mentioned. Moreover, although the promotion of insulin sensitisation in adipose tissue while causing decreased expression of TNF-α has been described for adiponectin [36], we did not observe that relationship in either in the SAT or the VAT.
Thus, it is unclear which parameter can better differentiate “healthy” and unhealthy obese patients. At least for the morbidly obese, the difficulty lies in strictly defining what constitutes a “healthy obese” patient, as indicated by other authors [18]. From our point of view, the state of being obese is not “healthy”, especially in the case of morbid obesity. As discussed by Pataky et al. [37], although remaining within a normal range, metabolically normal obese subjects show an elevated lipid profile and insulin resistance compared with controls of normal body weight, and for the majority of the obese subjects, metabolic normality is ephemeral.
In conclusion, the morbidly obese “healthy” individual is not really metabolically healthy but morbidly obese individuals with diabetes and dyslipidemia are more metabolically imbalanced. However, a year after bariatric surgery, independent of comorbidities, recovery of many of the biochemical parameters that were previously altered was observed both in plasma and adipose tissue.
Abbreviations
- RYGBP:
-
Roux-en-Y gastric bypass
- HOMA-IR:
-
Homeostasis model assessment of insulin resistance
- NEFA:
-
Non-esterified fatty acid
- TG:
-
Triglyceride
- TC:
-
Total cholesterol
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- DM:
-
Diabetes mellitus
- DL:
-
Dyslipidemia
- HTA:
-
Arterial hypertension
- PAI-1:
-
Plasminogen activator inhibitor-1
- CRP:
-
C-Reactive Protein
- SAT:
-
Subcutaneous adipose tissue
- VAT:
-
Visceral adipose tissue
- CVD:
-
Cardiovascular disease
References
Pataky Z, Bobbioni-Harsch E, Golay A. Open questions about metabolically normal obesity. Int J Obes (Lond). 2010;34 Suppl 2:S18–23.
Pataky Z, Bobbioni-Harsch E, Makoundou V, et al. What is the evolution of metabolically normal obesity? Rev Med Suisse. 2011;7(288):692–4.
Barbarroja N, Lopez-Pedrera R, Mayas MD, et al. The obese healthy paradox: is inflammation the answer? Biochem J. 2010;430(1):141–9.
Pataky Z, Makoundou V, Nilsson P, et al. Metabolic normality in overweight and obese subjects. Which parameters? Which risks? Int J Obes (Lond). 2011;35:1208–15.
Pardina E, Baena-Fustegueras JA, Catalan R, et al. Increased expression and activity of hepatic lipase in the liver of morbidly obese adult patients in relation to lipid content. Obes Surg. 2009;19(7):894–904.
Pardina E, Ferrer R, Baena-Fustegueras JA, et al. The relationships between IGF-1 and CRP, NO, leptin, and adiponectin during weight loss in the morbidly obese. Obes Surg. 2010;20(5):623–32.
NCEP. Executive summary of the third report of The National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA. 2001;285:2486–97.
ESH and ESC. Task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2007;25:1105–87.
Wildman RP. Healthy obesity. Curr Opin Clin Nutr Metab Care. 2009;12:438–43.
Standardization of anthropometric measurements. In: Lohman T, Roche A, Martorel R, eds.Champaign, IL: Human Kinetics Publishers. 1988;39–80.
Pardina E, Ferrer R, Baena-Fustegueras JA, et al. Only C-reactive protein, but not TNF-α or IL6, reflects the improvement in inflammation after bariatric surgery. Obes Surg. 2012;22(1):131–9.
Marcovina SM, Albers JJ. Apolipoprotein assays: standardization and quality control. Scand J Clin Lab Invest. 1990;50(198):58–65.
Matthews DR, Hosker JP, Rudenski AS, et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–9.
Aguilar-Salinas CA, Garcia EG, Robles L, et al. High adiponectin concentrations are associated with the metabolically healthy obese phenotype. J Clin Endocrinol Metab. 2008;93(10):4075–9.
Karelis AD, Faraj M, Bastard JP, et al. The metabolically healthy but obese individual presents a favorable inflammation profile. J Clin Endocrinol Metab. 2005;90(7):4145–50.
Meigs JB, Wilson PW, Fox CS, et al. Body mass index, metabolic syndrome, and risk of type 2 diabetes or cardiovascular disease. J Clin Endocrinol Metab. 2006;91(8):2906–12.
Wildman RP, Kaplan R, Manson JE, et al. Body size phenotypes and inflammation in the women’s health initiative observational study. Obesity (Silver Spring). 2011;19(7):1482–91.
Phillips CM, Perry IJ. Does inflammation determine metabolic health status in obese and nonobese adults? J Clin Endocrinol Metab. 2013;98(10):E1610–9.
Tchernof A, Despres JP. Pathophysiology of human visceral obesity: an update. Physiol Rev. 2013;93(1):359–404.
Brochu M, Tchernof A, Dionne IJ, et al. What are the physical characteristics associated with a normal metabolic profile despite a high level of obesity in postmenopausal women? J Clin Endocrinol Metab. 2001;86(3):1020–5.
Shin MJ, Hyun YJ, Kim OY, et al. Weight loss effect on inflammation and LDL oxidation in metabolically healthy but obese (MHO) individuals: low inflammation and LDL oxidation in MHO women. Int J Obes (Lond). 2006;30(10):1529–34.
Barbarroja N, Lopez-Pedrera C, Garrido-Sanchez L, et al. Progression from high insulin resistance to type 2 diabetes does not entail additional visceral adipose tissue inflammation. PLoS One. 2012;7:e48155. doi:10.1371/journal.pone.0048155.
Elissondo N, Gómez Rosso L, Maidana P, et al. Adiponectina: una adipocitoquina con múltiples funciones protectoras. Acta Bioquim Clin Latinoam. 2008;42(1):17–33.
Kadowaki T, Yamauchi T, Kubota N, et al. Adiponectin and adiponectin receptors in insulin resistance, diabetes, and the metabolic syndrome. J Clin Invest. 2006;116(7):1784–92.
Degawa-Yamauchi M, Moss KA, Bovenkerk JE, et al. Regulation of adiponectin expression in human adipocytes: effects of adiposity, glucocorticoids, and tumor necrosis factor alpha. Obes Res. 2005;13(4):662–9.
Matsuzawa Y. Establishment of a concept of visceral fat syndrome and discovery of adiponectin. Proc Jpn Acad Ser B Phys Biol Sci. 2010;86(2):131–41.
Butner KL, Nickols-Richardson SM, Clark SF, et al. A review of weight loss following Roux-en-Y gastric bypass vs restrictive bariatric surgery: impact on adiponectin and insulin. Obes Surg. 2010;20(5):559–68.
Yang WS, Chen MH, Lee WJ, et al. Adiponectin mRNA levels in the abdominal adipose depots of nondiabetic women. Int J Obes Relat Metab Disord. 2003;27:896–900.
Altomonte J, Harbaran S, Richter A, et al. Fat depot-specific expression of adiponectin is impaired in Zucker fatty rats. Metab Clin Exp. 2003;52:958–63.
Daniele A, Cammarata R, Masullo M, et al. Analysis of adiponectin gene and comparison of its expression in two different pig breeds. Obesity. 2008;16:1869–74.
De Rosa A, Monaco ML, Capasso M, et al. Adiponectin oligomers as potential indicators of adipose tissue improvement in obese subjects. Eur J Endocrinol. 2013;169:37–43.
Recasens M, Ricart W, Fernandez-Real JM. Obesity and inflammation. Rev Med Univ Navarra. 2004;48(2):49–54.
Montague CT, Prins JB, Sanders L, et al. Depot- and sex-specific differences in human leptin mRNA expression: implications for the control of regional fat distribution. Diabetes. 1997;46(3):342–7.
Fisher FM, McTernan PG, Valsamakis G, et al. Differences in adiponectin protein expression: effect of fat depots and type 2 diabetic status. Horm Metab Res. 2002;34(11–12):650–4.
Rodríguez A, Catalán V, Gómez-Ambrosi J, et al. Visceral and subcutaneous adiposity: are both potential therapeutic targets for tackling the metabolic syndrome? Curr Pharm Des. 2007;13(21):2169–75.
Bastard JP, Maachi M, Lagathu C, et al. Recent advances in the relationship between obesity, inflammation, and insulin resistance. Eur Cytokine Netw. 2006;17(1):4–12.
Pataky Z, Bobbioni-Harsch E, Golay A. Response to ‘Metabolically normal obesity’ a misnomer? Int J Obes (Lond). 2011;36:165.
Acknowledgments
Study concept and design (JAB-F, JP-O), surgery and endocrinology studies of patients (JAB-F, JMF, JMB, EC, OG, RV, AL) performed experiments (RF, EP, JR), tissue analyses (RF, EP, JR), analysis and interpretation of data (JAB-F, JP-O, AL, RF, EP, JR), obtained funding (JP-O), drafting of manuscript (JP-O), critical revision of the manuscript for important intellectual content (JAB-F, JP-O, AL, RF). We thank Dr. Miñarro of the Biostatistics Dept. of Biology Fac. (UB) for their invaluable help. All authors were involved in writing the paper and approved the final version of the manuscript. English grammar and language were corrected by American Journal Experts (www.journalexperts.com).
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional and/or National research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare that no conflicts of interest exist. The authors who have taken part in this study do not have a relationship, past or present, with the manufacturers of the drugs involved and did not receive funding from the manufacturers to conduct their research.
Author information
Authors and Affiliations
Corresponding author
Additional information
Roser Ferrer and Eva Pardina have contributed equally to this study.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 48 kb)
Rights and permissions
About this article
Cite this article
Ferrer, R., Pardina, E., Rossell, J. et al. Morbidly “Healthy” Obese Are Not Metabolically Healthy but Less Metabolically Imbalanced Than Those with Type 2 Diabetes or Dyslipidemia. OBES SURG 25, 1380–1391 (2015). https://doi.org/10.1007/s11695-014-1528-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-014-1528-z