Abstract
Background
Data regarding albendazole monotherapy for cystic echinococcosis (CE) are scarce, especially in children. We report our experience treating CE in children with albendazole monotherapy.
Methods
A retrospective case series, 2005–2021, assessing factors leading to albendazole monotherapy, demographic, clinical, duration of treatment and follow-up, and outcome (changes in cyst size and side effects) characteristics.
Results
Overall, we identified 18 patients with 31 cysts; liver: 68% (n = 21), lungs: 29% (n = 9), and kidney: 3% (n = 1). Mean cyst size was 4.5 ± 2.6 cm. Reasons for administrating albendazole monotherapy were small (< 4 cm) cyst size (56%), difficulty to operate (33%) and comorbidity (22%). Duration of treatment (range 1–32 months) was 1, 2–3, 4–6 and > 6 months in 28% (n = 5), 39% (n = 7), 17% (n = 3) and 17% (n = 3) of children, respectively. Duration of follow up (range 1–87 months) was 1, 2–3, 4–6 and > 6 months in 11% (n = 2), 11% (n = 2), 17% (n = 3) and 61% (n = 11) of children, respectively. Overall, 83% (n = 15) of patients experienced lack of cyst growth, and 72% (n = 13) experienced reduction in cyst size, while 44% (n = 8) experienced reduction larger than 50%. Full resolution was noted in 22% (n = 4) of patients. In three cases (17%) treatment failure was recorded: one (6%) recurrence, and two cases (11%) of cyst growth. Neutropenia was recorded in two patients (11%), and liver enzymes elevation was recorded in six patients (33%).
Conclusions
Albendazole monotherapy may be an adequate treatment for selected cases of CE disease in children, especially in CE with small, hepatic cysts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cystic echinococcosis (CE) is a zoonotic disease caused by the larval cystic stage of the dog tapeworm Echinococcus granulosus [1]. Children, especially in endemic regions, such as Africa, Asia, and the Middle East, become infected by ingesting the parasite eggs from the stool of stray dogs, which did not receive prophylactic praziquantel, deworming treatment [2]. Several treatments are currently recommended for treating CE based on radiological criteria meant to determine the viability of the hydatid cyst [3]. Most of the treatment modalities are surgical, due to the nature of the cystic disease [4]. In most cases, albendazole regimen is included as a complement part of the surgical intervention.
Administration of benzimidazoles for inoperable cases of hydatid cysts is very effective against the parasite in humans [5]. After nearly 50 years of use, albendazole is the main medication in the management of cystic echinococcosis, combined with other anthelminthic drugs, like praziquantel, or administrated alone [6]. Albendazole is an effective drug for echinococcosis, if the liver can derive albendazole sulphoxide, the drug principal metabolite which cause the therapeutic effect of the medicine [3, 7]. Recent studies even suggest that continuous treatment achieves equivalent or improved efficacy compared to that of surgery, with no increased adverse effects [8]. Pharmacological treatment improved results in patients with CE when it was involved in combinations with surgical interventions and showed higher scolicidal activity [9, 10]. Nevertheless, medical treatment for children is not well established as part of the treatment guidelines for CE [3].
Considerations for choosing albendazole monotherapy are not well defined. There are data suggesting that this treatment is mostly chosen in cases with a higher risk of rupturing a cyst during surgery [11]. Others suggest that thinner walls of cysts in certain organs may make cysts more susceptible to albendazole monotherapy [12]. Additionally, this method is reserved for those with cysts in multiple organs, or small, uncomplicated cysts [13]. Small cysts were previously defined as cysts smaller than 4 cm [14]. It was also suggested to be an appropriate treatment for asymptomatic patients, or for patients who declined other medical treatment [13, 15].
Albendazole monotherapy effect on CE is not fully understood—Though reliably causing cystic degeneration, the effect on the clinical course of disease is less predictable [16]. Cases of spontaneous recovery in patients treated with albendazole monotherapy have been documented [15].
When assessing the complication profile for albendazole monotherapy, some research indicates that recurrence of CE can occur in as much as 25% of patients treated with chemotherapy only [8]. Importantly, in the event of a CE relapse after monotherapy, up to 90% are sensitive to re-treatment [17]. Other common notable side effects are increased liver enzymes, neutropenia (isolated or as part of pancytopenia), alopecia, and general gastrointestinal symptoms. The most common central nervous system (CNS) effect reported was headache [18].
In this case series, our main goal was to report our experience of treating pediatric CE with albendazole monotherapy. First, we aimed to create a better understanding of the suitable criteria for choosing albendazole monotherapy. Second, we tried to analyze the association between this treatment and the clinical outcome in our patients. Lastly, we tried to shed light upon the complication profile that the physician should consider when choosing this type of intervention.
Methods
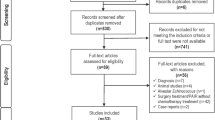
Study Design
This is a retrospective case series study, assessing all children with CE (hydatid disease) treated with albendazole monotherapy at the Soroka University Medical Center (SUMC) between the years 2005 through 2021.
The study was approved by the SUMC review board committee. Due to its retrospective nature, a waiver of informed consent was granted.
Setting and Study Population
The SUMC is the only hospital in the Negev district of southern Israel, providing primary and referral health services to the entire population of the region (~ 200,000 children < 18 years). Over 95% of the children living in the Negev region are served by the SUMC, enabling population-based studies.
The population in the SUMC catchment area is composed of two ethnic groups: the Jewish population, generally comparable with a Western population, and the Bedouin Arab population, generally comparable to a low-middle income country (LMIC) population. Contact between children of the two populations is rare, but both have access to the same medical services. Medical insurance for children is universal and free of charge. In southern Israel, CE was reported to be endemic in the Bedouin population, while in the Jewish population cases were almost exclusively reported among adults and imported from other countries [19].
The SUMC Ethical Committee approved this study with approval number SOR-0047-22.
Cystic Echinococcosis Definition
Cystic echinococcosis diagnosis was defined by a clinical decision made by the treating physician based upon typical imaging with or without positive echinococcosis serology, which led to anti-helminthic treatment.
Classification of Hepatic Cystic Echinococcosis Lesions Based on Ultrasound Examination
Cyst were classified by a well-accepted classification of hepatic cystic echinococcosis lesions based on ultrasound examination [3]. According to the WHO guidelines, the treatment of CE disease is defined by sonomorphological classification that facilitates the diagnosis [3].
Chemotherapy as Monotherapy Treatment
Treatment with albendazole was defined when administrated as typically; 1–6 monthly cycles separated by 10–14-day intervals [11]. Albendazole regimen was defined as 15 mg/kg/day, divided into two doses, to maximum 400 mg orally twice daily with food. Albendazole monotherapy was defined as treatment that did not include surgical intervention of any kind, such as drainage or excision procedures. New course of treatment was defined when it was given after period longer than 28 days in which the patient did not received albendazole. Compliance with treatment was evaluated by follow-up meetings at the SUMC pediatric infectious disease unit.
Side Effect of Albendazole Treatment
Elevation in Liver Enzymes
Elevation in liver enzymes was defined as rise in measured levels of GOT or GPT at the same date or up to a month of the date of estimation [18, 20]. According to the WHO guidelines, normal range of values for AST (SGOT) is between 8 and 45 units per liter of serum. The normal range of values for ALT (SGPT) is about 7–38 units per liter of serum.
Neutropenia
Long-term (28 days) treatment with albendazole has shown to possibly lead to neutropenia due to myelosuppression character of the treatment. In adults, a count of 1500 neutrophils per microliter of blood or less is neutropenia, with any count below 500 per microliter of blood regarded as a severe case [18].
Recurrence
Recurrence was defined as return of an echinococcal cyst typical imaging, at least 30 days after that location was defined clear by radiologist based on imaging [18].
Data Collection Method
Data were collected from the computerized files of children ≤ 18 years who were tested for CE via ELISA at the SUMC between 2005 and 2021 and were diagnosed with CE. These data were included in the current study.
The following data were collected: Demographics (age, gender, and ethnicity); clinical and laboratory data (fever, abdominal pain, jaundice, hepatomegaly, abdominal mass, respiratory symptoms, GOT, GPT, neutrophils and eosinophilia); number, location, and size of cysts, based on relevant imaging; treatment and follow-up (duration, changes in cyst size).
Results
Study Population
Overall, 18 patients with 31 cysts were identified. All patients were of Bedouin ethnicity, and 56% were males. Mean number of cysts was 1.8 ± 0.9 per patient; 50% (n = 9) of the patients had more than one cyst. In 89% of cases, cysts were in a single organ, while 11% (n = 2) had multi organ disease. When assessing distribution of cyst location, 68% (n = 21) were in the liver, 29% (n = 9) were in the lungs and 0.3% (n = 1) were in the kidney. Mean cyst size was 4.5 ± 2.6 cm, and 55% (n = 17) of the cysts were larger than 4 cm.
The reasons for administrating albendazole monotherapy were analyzed. In 56% (n = 10) of the cases, small cyst size was noted as a reason for choosing conservative treatment. For 33% (n = 6) of the patients, difficulty to operate was the reason reported, and for 22% (n = 4) of patients, comorbidity was noted as a reason to not risk an immunocompromised patient in surgical procedure. Notably, 22% (n = 4) of patients has a combination of the reasons noted (Table 1).
Albendazole Monotherapy Patient Characteristics and Treatment Outcomes
Treatment Characteristics
Albendazole was given for duration of 1–32 months, while duration of follow up was 1–87 months. Albendazole treatment was given for 1, 2–3, 4–6 and > 6 months in 28% (n = 5), 39% (n = 7), 17% (n = 3) and 17% (n = 3) of the children, respectively. Follow-up imaging studies were performed in 1, 2–3, 4–6 and > 6 months in 11% (n = 2), 11% (n = 2), 17% (n = 3) and 61% (n = 11) of the children, respectively (Table 2).
Clinical Outcomes
Eighty three percent of all patients (n = 15) experienced lack of cyst growth, and 72% (n = 13) experienced reduction in cyst size, while 44% (n = 8) experienced reduction larger than 50%. Full resolution of cysts was noted in 22% (n = 4) of patients. Overall, one case of recurrence was reported. In 11% (n = 2) of patients, growth of cysts was detected on follow-up assessments.
Treatment Outcomes by Length of Treatment and Follow-Up Period
Among patients who received albendazole treatment for 1 month, 70% (7/10) of cysts were reduced by at least 25% in size at the end of follow-up period. Notably, 50% (5/10) were reduced by more than 50%. For 70% (7/10) of treated cysts, change in cyst size was noted during first 10 months of follow-up. One case of recurrence was recorded after 10 months of follow-up (Fig. 1).
Among patients who received albendazole treatment for 2–3 months, 71% (5/7) of cysts were reduced by at least 25% in size at the end of follow-up period. Additionally, 43% (3/7) were reduced by more than 50% in size. For 43% (3/7) of treated cysts, reduction in cyst size was noted during first month of follow-up. For 29% (2/7) of treated cysts, reduction in cyst size was noted 12 months after starting treatment. Cases of recurrence or cyst growth were not recorded.
Among patients who received albendazole treatment for 4–6 months, 71% (5/7) of cysts were reduced by more than 50% in size at the end of the follow-up period. For 57% (4/7) of treated cysts, reduction in cyst size was noted 6 months after starting treatment. One case of cyst growth (14%) was recorded during the first 11 months of follow-up.
Among patients who received albendazole treatment for more than 6 months, 50% (2/4) of cysts were reduced by at least 25% in size at the end of follow-up period. All cases of reduction in cyst size were detected more than 22 months after starting treatment. One case of cyst growth (14%) was recorded during the first 9 months of follow-up (Table 3).
Adverse Events
Neutropenia
For 15 (83%) of 18 patients, neutrophil count was recorded at baseline (pre-treatment). Of those, none had neutropenia (< 1500/mm3). For two patients (11%), neutropenia was recorded following treatment (with trough values of 1440/mm3 and 1210/mm3). In both cases, treatment was continued.
Liver Enzymes
For 15 (83%) of 18 patients, liver enzymes levels (either GOT, GPT or both) was recorded at baseline (pre-treatment). Of those, one (5.5%) had elevated liver enzymes (GOT and GPT) at baseline. Following treatment, in 6 patients (33%) elevated liver enzymes were recorded. Four patients (22%) had elevation of both.
Other
No cases of alopecia, headache or gastrointestinal symptoms were recoded.
Discussion
In this retrospective case series study, we report our experience of treating CE in children with albendazole monotherapy. Eighteen cases were detected between the years 2005–2021, providing supportive evidence for the utility of albendazole monotherapy treatment of CE in children, especially in multiple, small hepatic cysts disease, as reported before, and surprisingly also in extra hepatic CE, mostly in the lungs. Additionally, we describe the complication profile of albendazole monotherapy in children.
Albendazole monotherapy might be considered a suitable choice for treatment of CE disease in selected pediatric cases. Of the 18 patients treated in our center, 83% experienced lack of cyst growth, and 72% experienced some reduction in cyst size. Furthermore, 44% of patients have experienced a reduction of more than 50% in cyst size. Studies have previously shown that albendazole monotherapy is effective in reducing cyst size, as a measurement of clinical outcome in adults [16]. Our work shed light upon the impressive results of albendazole monotherapy in children.
When assessing disease characteristics associated with choosing albendazole monotherapy in our center, we found that cysts located in the liver, multiple cysts, and small cyst size (smaller than 4 cm) were common among children selected. These findings are in accordance with previous studies, suggesting that patients with these features will benefit the most from choosing non-surgical intervention [11, 12, 14].
Other considerations for administrating albendazole monotherapy include difficulties in surgery, such as cysts located close to bile ducts and severe co-morbidities such as systemic infections or cancerous processes. These reasons for choice of treatment highlight the fact that conservative treatment is mostly chosen when the surgical procedure itself might endanger the patient [11].
Interestingly, Albendazole monotherapy can benefit CE patients with extra hepatic cyst locations, mostly in the lungs. The leading reasons reported for choosing albendazole monotherapy among these patients were small cyst size, and difficulty to operate cysts located closely to air bronchi or the pulmonary pleura. Clinical outcomes of albendazole monotherapy for extra hepatic disease, especially in children, were rarely reported [21]. In the current study, during follow-up period of 50 months, five cysts were resolved, and four were reduced by more than 50% in cyst size.
Evaluation of disease outcomes and side effects of albendazole monotherapy highlight the need for strict follow of these cases. For several patients, cyst growth was noted during follow-up imaging. One case of recurrence was documented 50 months after the beginning of treatment. Recurrence of CE can occur in as much as 25% of patients treated with chemotherapy alone [8]. Importantly, there are reports of cysts having initially responded, and then reverted to active status up to 2 years after treatment, emphasizing the need for prolonged observation period, even in cases with initial improvement. Current literature lacks more information about albendazole monotherapy success/failure rate, even though cases of recurrence in pulmonary disease were reported [21]. Other complications of albendazole monotherapy were relatively mild and uncommon. Neutropenia, a well-documented side effect [18, 21], was recorded in two patients following treatment. Yet, in both cases, treatment was continued. Similarly, elevation of liver enzymes [18, 22] was recorded in 6 patients (33%). Other and relatively rare adverse events such as alopecia or headache, that were reported previously [18, 23], were not reported during our study.
The main advantages of this study include our unique setting, in which we have a relatively high number of confirmed CE cases in children, with an extent follow-up period. We acknowledge several limitations. First, the relatively small number of patients. Second, for several patients some clinical data were missing, as well as possibly limited reporting of side effects in retrospective collection. In addition, evaluating treatment adherence could be rather difficult, especially among rural population, like the Bedouin in southern Israel, as was presented previously [24]. To ensure adherence, follow-up meetings were scheduled at SUMC pediatric infectious disease unit, and the administration of medications was checked in patients' files. Finally, differentiating recurrence of an old disease from re-infection is impossible in an endemic population, with continuous exposure to the parasite eggs. Nevertheless, we believe that this case series gives an important perspective about the reasons for administrating, the clinical outcomes, and the side effect profile of albendazole monotherapy.
In conclusion, in this retrospective case series, we reported a single center experience of treating CE in children with albendazole monotherapy. We found supportive evidence for the utility of albendazole monotherapy in multiple, small hepatic cyst disease, and even in certain cases of extra hepatic cyst disease. Finally, we achieved a better understanding of the complication profile for albendazole monotherapy in children.
References
Thompson RC (2017) Biology and systematics of echinococcus. Adv Parasitol 95:65–109. https://doi.org/10.1016/bs.apar.2016.07.001
Tamarozzi F, Silva R, Fittipaldo VA, Buonfrate D, Gottstein B, Siles-Lucas M (2021) Serology for the diagnosis of human hepatic cystic echinococcosis and its relation with cyst staging: a systematic review of the literature with meta-analysis. PLoS Negl Trop Dis 15(4):e0009370. https://doi.org/10.1371/journal.pntd.0009370
Brunetti E, Kern P, Vuitton DA, Writing Panel for the W-I (2010) Expert consensus for the diagnosis and treatment of cystic and alveolar echinococcosis in humans. Acta Trop 114(1):1–16. https://doi.org/10.1016/j.actatropica.2009.11.001
Haralabidis S, Diakou A, Frydas S et al (2008) Long-term evaluation of patients with hydatidosis treated with albendazole and praziquantel. Int J Immunopathol Pharmacol 21(2):429–435. https://doi.org/10.1177/039463200802100223
Yasawy MI, Mohamed AR, Al-Karawi MA (1992) Albendazole in hydatid disease: results in 22 patients. Ann Saudi Med 12(2):152–156. https://doi.org/10.5144/0256-4947.1992.152
El-On J (2003) Benzimidazole treatment of cystic echinococcosis. Acta Trop 85(2):243–252. https://doi.org/10.1016/s0001-706x(02)00217-6
Stojkovic M, Rosenberger K, Kauczor HU, Junghanss T, Hosch W (2012) Diagnosing and staging of cystic echinococcosis: how do CT and MRI perform in comparison to ultrasound? PLoS Negl Trop Dis 6(10):e1880. https://doi.org/10.1371/journal.pntd.0001880
Stojkovic M, Zwahlen M, Teggi A et al (2009) Treatment response of cystic echinococcosis to benzimidazoles: a systematic review. PLoS Negl Trop Dis 3(9):e524. https://doi.org/10.1371/journal.pntd.0000524
Aydin Y, Ulas AB, Ince I et al (2022) Evaluation of albendazole efficiency and complications in patients with pulmonary hydatid cyst. Interact Cardiovasc Thorac Surg 34(2):245–249. https://doi.org/10.1093/icvts/ivab259
Velasco-Tirado V, Alonso-Sardon M, Lopez-Bernus A et al (2018) Medical treatment of cystic echinococcosis: systematic review and meta-analysis. BMC Infect Dis 18(1):306. https://doi.org/10.1186/s12879-018-3201-y
Bhutani N, Kajal P (2018) Hepatic echinococcosis: a review. Ann Med Surg (Lond) 36:99–105. https://doi.org/10.1016/j.amsu.2018.10.032
Todorov T, Vutova K, Mechkov G, Petkov D, Nedelkov G, Tonchev Z (1990) Evaluation of response to chemotherapy of human cystic echinococcosis. Br J Radiol 63(751):523–531. https://doi.org/10.1259/0007-1285-63-751-523
Smego RA Jr, Sebanego P (2005) Treatment options for hepatic cystic echinococcosis. Int J Infect Dis 9(2):69–76. https://doi.org/10.1016/j.ijid.2004.08.001
Brunetti E, Tamarozzi F, Macpherson C et al (2018) Ultrasound and cystic echinococcosis. Ultrasound Int Open 4(3):E70–E78. https://doi.org/10.1055/a-0650-3807
Simon D, Koegelenberg CF, Sinha Roy S, Allwood BW, Irusen EM (2016) Can large hydatid cysts resolve with medical treatment alone? Respiration 92(6):428–431. https://doi.org/10.1159/000451032
Fattahi Masoom SH, Lari SM, Fattahi AS, Ahmadnia N, Rajabi M, NaderiKalat M (2018) Albendazole therapy in human lung and liver hydatid cysts: a 13-year experience. Clin Respir J 12(3):1076–1083. https://doi.org/10.1111/crj.12630
Teggi A, Lastilla MG, Grossi G, Franchi C, Rosa F (1995) Increase of serum glutamic-oxaloacetic and glutamic-pyruvic transaminases in patients with hydatid cysts treated with mebendazole and albendazole. Mediterranean J Infect Parasitic Diseases 10:85–90
Chai JY, Jung BK, Hong SJ (2021) Albendazole and mebendazole as anti-parasitic and anti-cancer agents: an update. Korean J Parasitol 59(3):189–225. https://doi.org/10.3347/kjp.2021.59.3.189
Ben-Shimol S, Sagi O, Houri O et al (2016) Cystic echinococcosis in Southern Israel. Acta Parasitol 61(1):178–186. https://doi.org/10.1515/ap-2016-0024
Piloiu C, Dumitrascu DL (2021) Albendazole-induced liver injury. Am J Ther 28(3):e335–e340. https://doi.org/10.1097/MJT.0000000000001341
Dogru D, Kiper N, Ozcelik U, Yalcin E, Gocmen A (2005) Medical treatment of pulmonary hydatid disease: for which child? Parasitol Int 54(2):135–138. https://doi.org/10.1016/j.parint.2005.02.003
Choi GY, Yang HW, Cho SH et al (2008) Acute drug-induced hepatitis caused by albendazole. J Korean Med Sci 23(5):903–905. https://doi.org/10.3346/jkms.2008.23.5.903
Hong ST (2018) Albendazole and praziquantel: review and safety monitoring in Korea. Infect Chemother 50(1):1–10. https://doi.org/10.3947/ic.2018.50.1.1
Yoel U, Abu-Hammad T, Cohen A, Aizenberg A, Vardy D, Shvartzman P (2013) Behind the scenes of adherence in a minority population. Isr Med Assoc J 15(1):17–22
Author information
Authors and Affiliations
Contributions
MS and SBS have made a substantial contribution to the concept or design of the article, or the acquisition, analysis, or interpretation of data for the article. MS, SE, OS, and SBS drafted the article or revised it critically for important intellectual content. MS, SE, OS, DG, ZA, and SBS approved the version to be published. All authors agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that there are no competing interests. No funding has been received for this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shmueli, M., Elamour, S., Sagi, O. et al. Albendazole Monotherapy for Pediatric Cystic Echinococcosis: A Case Series. Acta Parasit. 68, 651–658 (2023). https://doi.org/10.1007/s11686-023-00699-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11686-023-00699-6