Abstract
Mild traumatic brain injury (mTBI) is highly prevalent in military populations, with many service members suffering from long-term symptoms. Posttraumatic stress disorder (PTSD) often co-occurs with mTBI and predicts worse clinical outcomes. Functional neuroimaging research suggests there are both overlapping and distinct patterns of resting-state functional connectivity (rsFC) in mTBI versus PTSD. However, few studies have directly compared rsFC of cortical networks in military service members with these two conditions. In the present study, U.S. service members (n = 137; ages 19–59; 120 male) underwent resting-state fMRI scans. Participants were divided into three study groups: mTBI only, PTSD only, and orthopedically injured (OI) controls. Analyses investigated group differences in rsFC for cortical networks: default mode (DMN), frontoparietal (FPN), salience, somatosensory, motor, auditory, and visual. Analyses were family-wise error (FWE) cluster-corrected and Bonferroni-corrected for number of network seeds regions at the whole brain level (pFWE < 0.002). Both mTBI and PTSD groups had reduced rsFC for DMN and FPN regions compared with OI controls. These group differences were largely driven by diminished connectivity in the PTSD group. rsFC with the middle frontal gyrus of the FPN was increased in mTBI, but decreased in PTSD. Overall, these results suggest that PTSD symptoms may have a more consistent signal than mTBI. Our novel findings of opposite patterns of connectivity with lateral prefrontal cortex highlight a potential biomarker that could be used to differentiate between these conditions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Mild traumatic brain injury (mTBI) is highly prevalent in both civilian and military populations and is often associated with a variety of persistent somatic, cognitive, and emotional symptoms (Levin & Diaz-Arrastia, 2015). Recent research indicates that the occurrence of mTBI in military service members is increasing, with over 300,000 service members diagnosed with mTBI since 2000 and many suffer from long-term symptoms (DVBIC, 2018; Reid & Velez, 2015; Snell & Halter, 2010). Therefore, it is particularly important to understand the clinical and neurobiological correlates of mTBI in military service members. Establishing reliable and distinct markers of mTBI may help in developing more accurate diagnostic tools and treatments aimed at reducing the persistent and debilitating long-term impacts of mTBI in service members.
Compared with clinical structural imaging, research indicates that functional magnetic resonance imaging (fMRI) can be used to detect neurobiological changes associated with mTBI. Using resting-state fMRI (rs-fMRI), which measures low-frequency fluctuations in brain activity at rest, researchers have identified alterations in resting-state functional connectivity (rsFC) within and between several cortical networks in mTBI (Mayer et al., 2011; Slobounov et al., 2011; Sours et al., 2013; Stevens et al., 2012; Vakhtin et al., 2013; Zhou et al., 2012). Studies have consistently reported reduced rsFC within the default mode network (DMN) in mTBI in civilians, in particular for posterior portions of the DMN such as the posterior cingulate/precuneus (Mayer et al., 2011; Sours et al., 2013; Stevens et al., 2012; Zhou et al., 2012). On the other hand, rsFC is often increased within the prefrontal cortex in mTBI, including for medial prefrontal regions of the DMN (Sours et al., 2013; Zhou et al., 2012) and lateral prefrontal areas in the frontoparietal network (FPN; Mayer et al., 2011;Stevens et al., 2012 ; Vakhtin et al., 2013). Besides the DMN and FPN, studies have also found altered rsFC within and between other cognitive, affective, and sensorimotor networks in mTBI (Stevens et al., 2012; Vakhtin et al., 2013). For instance, Stevens et al. (2012) reported abnormalities in rsFC within the salience, limbic, visual, and motor networks in civilians with mTBI.
Posttraumatic stress disorder (PTSD) often co-occurs with mTBI in military service members, with comorbidity rates between 33 and 43% (Carlson et al., 2011; Hoge et al., 2008; Polusny et al., 2011; Schneiderman et al., 2008). Regardless of mTBI status, longitudinal and cross-sectional research suggests that PTSD is consistently associated with worse clinical and cognitive outcomes (Hayes et al., 2015; Mac Donald et al., 2015; Shandera-Ochsner et al., 2013; Vasterling et al., 2012; Verfaellie et al., 2014), and abnormal white matter integrity (Bolzenius et al., 2018; Levin et al., 2010; Schuff et al., 2011). However, more limited research has examined the impact of PTSD versus mTBI on brain activity (Raji et al., 2015; Rowland et al., 2016; Santhanam et al., 2019). Therefore, an important question is whether functional neuroimaging, in particular rsFC, can be used to distinguish between mTBI and PTSD.
Functional neuroimaging studies suggest that abnormalities in rsFC of cortical networks in PTSD may partially overlap with network dysfunction in mTBI. Similar to mTBI, diminished rsFC within the DMN has been frequently reported in individuals with PTSD as compared to those without PTSD (Bluhm et al., 2009; Koch et al., 2016; D. R. Miller et al., 2017; Shang et al., 2014; Sripada et al., 2012; Wang et al., 2016). Recent meta-analyses of resting-state studies in PTSD have further revealed reduced rsFC of FPN regions including the middle frontal gyrus as well as enhanced rsFC of salience network regions, such as the insula, as compared with control groups (Koch et al., 2016; Wang et al., 2016). While these findings provide support for similarities in cortical resting-state networks affected by PTSD and mTBI, they also highlight some potential differences. For example, there appears to be diminished rsFC of the middle frontal gyrus within the FPN in PTSD (Koch et al., 2016; Olson et al., 2018), but elevated rsFC of overlapping lateral prefrontal regions in mTBI (Mayer et al., 2011; Zhou et al., 2012). Yet, to our knowledge only one study has directly compared rsFC of cortical networks in Service Members with mTBI to those with mTBI+PTSD (Santhanam et al., 2019). Santhanam et al. (2019) identified greater rsFC of the DMN in participants with mTBI only as compared with mTBI+PTSD, in particular for the mPFC. These findings provide preliminary support for differential rsFC of the DMN in mTBI versus PTSD. However, no study has yet investigated rsFC of other cortical networks, including the FPN and salience network, in service members with mTBI versus PTSD only.
The purpose of this study was to examine cross-sectional data from the study of cognitive rehabilitation effectiveness (SCORE) clinical trial to determine whether there are differences in rsFC of several cortical networks between U.S. service members with mTBI without PTSD, PTSD without mTBI, and orthopedically injured controls (OI). We used a seed-based voxelwise rsFC approach to examine group differences in rsFC within seven major cognitive, affective, sensory, and motor networks. In follow-up analyses, we also investigated relationships between significant rsFC findings and clinical symptom measures across the sample. Based on previous research, we hypothesized that: (1) there would be reductions in rsFC of posterior DMN regions in the mTBI and PTSD groups, and (2) there would be differences in rsFC between mTBI and PTSD groups, in particular for prefrontal regions within the DMN and FPN.
Method
Participants and procedure
Participants included 137 (120 Male, and 17 Female) active duty U.S. Service Members between the ages of 19 and 59 who were selected out of 162 originally recruited from a TBI clinic at a large military treatment facility. Seven participants were excluded due to data acquisition/quality issues (n = 5: mTBI[4], OI[1]) or excessive motion (n = 2: mTBI[1], PTSD[1], see “Motion Analysis” below). Remaining participants (n = 130) comprised three groups including mTBI (n = 48), PTSD (n = 24), and OI control (n = 58) participants (Table 1; see Supplemental Materials for a detailed description of inclusion/exclusion criteria). All subjects provided written informed consent in accordance with an approved institutional review board protocol at the Brooke Army Medical Center.
Clinical symptom measures
Each participant underwent an assessment of clinical symptoms collected concurrently (same week, mode = 1 day) with MRI acquisition. We collected self-report questionnaires to measure TBI symptoms (Neurobehavioral Symptom Inventory; Cicerone & Kalmar, 1995; King et al., 2012), PTSD symptoms (PTSD Checklist for DSM-IV-Military version; Bliese et al., 2008), and depression symptoms (Center for Epidemiological Studies-Depression Scale; Radloff, 1977).
MRI methods
Multimodal MRI were acquired on a 3 Tesla Siemens Verio scanner. Sequences administered included: T1 MPRAGE, T2, fluid attenuated inversion recovery, susceptibility weighted imaging, diffusion tensor imaging, and rs-fMRI. Total scan time for the whole set of sequences was approximately 75 min including preparation time. For this study, we used only the volumetric T1 and the rs-fMRI sequences (See Supplemental Materials for details regarding parameters for these scan sequences).
Preprocessing and motion analysis
All fMRI data analysis was performed using AFNI (Cox, 1996) and FSL (http://www.fmirb.ox.ac.uk/fsl/). We preprocessed the resting-state data using steps similar to those performed in previous studies (Philippi et al., 2015). See Supplemental Materials for a full description of the preprocessing steps.
We examined motion for each subject as individual differences in subject motion can contribute to resting-state correlations (Power et al., 2015). Only two subjects were excluded due to excessive motion (see Supplemental Materials for additional details). Average root-mean-squared (RMS) displacement was used as a summary measure of subject motion (as in Ciric et al., 2017). We found no significant relationships between average RMS displacement and participant group (F2,127 = 1.43, p > .2) or clinical variables (ps = .308–.853).
Functional connectivity analysis
We performed seed-based voxelwise rsFC analyses for 23 seed regions of interest (ROIs) for the following cortical networks previously implicated in mTBI (e.g., Bonnelle et al., 2012; Mayer et al., 2011; Stevens et al., 2012; Vakhtin et al., 2013; Zhou et al., 2012): DMN, FPN, salience, somatosensory, motor, auditory, and visual (Andrews-Hanna et al., 2007; Boveroux et al., 2010; Dosenbach et al., 2007). All network seed ROIs were 6-mm radius spherical seeds centered on the coordinates for each ROI in MNI space (3dcalc). The transformation matrix from the registration procedure described above was used to transform each seed from MNI space to original space (3dfractionize), with the accuracy of seed locations for each participant verified (C.L.P).
For each participant, the mean resting-state BOLD time series from each seed ROI was included in a GLM along with 14 regressors of no interest (as in Philippi et al., 2015; see Supplemental Materials for additional detail). The resulting z-score maps were then entered into the second level statistical analyses.
Statistical analyses
To examine group differences in rsFC, we performed multivariate modeling (3dMVM in AFNI) with separate models for rsFC z-score maps for each cortical network seed. All models included group as the between-subjects factor, with age and education as covariates. Age and education were included as covariates as there were significant group differences in these demographic variables (Table 1). Posthoc unpaired two-sample t tests were performed using SPSS (version 25; SPSS/IBM, Chicago, IL) to examine pairwise group differences for all significant results.
To correct for multiple comparisons, we implemented a family-wise error (FWE) correction approach at the cluster level using a whole-brain mask (3dClustSim in AFNI version updated May 2018) and applied cluster-extent thresholding (Carp, 2012; Forman et al., 1995). To address the non-Gaussian nature of fMRI data the autocorrelation function (−acf) was used to calculate the FWHM for each participant (3dFWHMx in AFNI; Eklund et al., 2016). Our results were FWE cluster-corrected at the whole brain level, with a predefined voxelwise threshold of p < 0.001 (uncorrected) and pFWE < 0.002 (Bonferroni-corrected for seed ROIs), with a cluster-corrected voxel size of ≥ 21 voxels.
We also conducted multiple linear regression analyses to examine the relationship between clinical symptoms and significant rsFC findings from the group analysis, while controlling for age and education. These analyses were Bonferroni-corrected (p = .05/[7 rsFC findings × 3 clinical symptoms] = .002).
Results
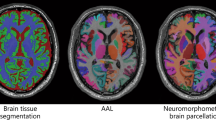
There were significant group differences in rsFC of DMN and FPN seeds (Table 2, Fig. 1). For the DMN, we found group differences in rsFC between the left inferior parietal lobule (IPL) and posterior cingulate/retrosplenial cortex (pCRsp) and regions in occipital cortex, including the lingual gyrus and cuneus. Posthoc tests revealed that these group differences were largely driven by diminished rsFC in the PTSD group as compared with mTBI and OI groups (Table 3). Reduced rsFC of DMN was also present for the mTBI group when compared with the OI group, with only pCRsp-left lingual gyrus connectivity significantly different at p < .05 (Table 3).
Altered rsFC in DMN and FPN seeds in mTBI and PTSD. Significant group differences in rsFC were found for the following DMN and FPN seeds: (a) L LatPar seed of DMN and left lingual gyrus; (b) pCRsp seed of DMN and bilateral visual cortex regions (i.e., lingual gyrus and cuneus); (c) L dlPFC seed of FPN and inferior parietal cortex and right middle frontal gyrus. The seed ROIs (red) and all results are displayed on an MNI template. The color bar depicts the F-statistic from the overall ANCOVA model, controlling for age and education. Bar graphs plot average rsFC (z-score) for OI (white), mTBI (blue), and PTSD (grey) groups and error bars correspond to ±1 standard error. All results survived whole-brain cluster correction, including Bonferroni-correction for number of cortical network seeds (pFWE < 0.002, p < 0.001 uncorrected, cluster-corrected voxel size of ≥21 voxels). Abbreviations: L LatPar = left lateral parietal, pCRsp = posterior cingulate /retrosplenial cortex, L dlPFC = left dorsolateral prefrontal cortex
For the FPN, there were group differences in rsFC between the left dorsolateral prefrontal cortex (dlPFC) and right IPL and right middle frontal gyrus. Posthoc tests showed that rsFC of the left dlPFC was significantly decreased in the PTSD group as compared with mTBI and OI groups (Table 3). By contrast, rsFC between the left dlPFC and right middle frontal gyrus was significantly increased in the mTBI group relative to the PTSD and OI groups (Table 3).
Follow-up analyses revealed relationships between rsFC of the pCRsp of the DMN and clinical symptom measures. TBI and PTSD symptoms were significantly associated with decreased rsFC between pCRsp and left lingual gyrus (Table 4). There were no significant relationships between depression symptoms and rsFC of DMN or FPN seeds (Supplemental Materials, Table S1).
Discussion
The present study provided evidence for both overlapping and distinct rsFC in cortical networks in U.S. Service Members with mTBI versus PTSD. Both mTBI and PTSD groups had reduced rsFC of DMN and FPN regions in comparison to OI controls. On the other hand, there were divergent patterns of rsFC between the dlPFC of the FPN and middle frontal gyrus in participants with mTBI versus PTSD. Follow-up analyses indicated that mTBI and PTSD symptom measures were associated with group differences in rsFC of the pCRsp of the DMN with the occipital cortex. We will discuss each of these findings in further detail.
Consistent with our hypothesis, we found reduced rsFC of IPL and pCRsp of the DMN in both mTBI and PTSD groups. Specifically, there was diminished rsFC was between posterior DMN regions and areas within the visual network, including the lingual gyrus and cuneus. Our results align with prior functional and structural neuroimaging research documenting abnormalities in visual cortical regions in both mTBI (Gilmore et al., 2016; Palacios et al., 2017; Slobounov et al., 2011; Stevens et al., 2012) and PTSD (Disner et al., 2018; Lanius et al., 2006; Mueller-Pfeiffer et al., 2013; Rauch et al., 1996; Wang et al., 2016; Zhang et al., 2011; Zhu et al., 2014). Researchers have proposed that disrupted functioning in visual cortex in both mTBI and PTSD could reflect abnormal integration of visual information with higher-order processes, such as visual attention (Gilmore et al., 2016; Lanius et al., 2006). However, additional research is warranted to determine whether reduced rsFC with visual cortex in mTBI and PTSD is associated with impaired higher-order visual processing.
We also identified diminished rsFC between the left dlPFC of the FPN and right IPL as well as the right middle frontal gyrus in individuals with PTSD as compared with those with mTBI and OI. Similar to our findings, previous studies have reported reduced connectivity of FPN structures in PTSD (Koch et al., 2016; Misaki et al., 2018; Olson et al., 2018). For instance, PTSD patients exhibited more negative rsFC between dlPFC and precuneus of the FPN than trauma-exposed and non-trauma exposed control participants (Olson et al., 2018). Together, these results suggest that PTSD is associated with aberrant FPN connectivity.
Overall, the group differences we identified were primarily driven by diminished rsFC in the PTSD group. One potential interpretation of these findings is that PTSD may be associated with more homogeneous neurobiological changes than mTBI (Bolzenius et al., 2018). In line with this hypothesis, prior studies have reported more robust relationships between PTSD and structural abnormalities than those with mTBI (Bazarian et al., 2013; Bolzenius et al., 2018). PTSD symptoms have also been consistently associated with dysfunction in cortical and subcortical circuits involved in threat, avoidance, reward, and arousal (Fenster et al., 2018). By comparison, clinical symptoms in mTBI are often heterogeneous and brain imaging abnormalities are often diffuse and variable (McDonald et al., 2012; Morey et al., 2013; Rosenbaum & Lipton, 2012). Nevertheless, given paucity of studies directly comparing rsFC in mTBI versus PTSD, these results will require replication to determine whether PTSD has more consistent neural signatures than mTBI.
In contrast to reduced rsFC in PTSD, Service Members with mTBI displayed significantly greater rsFC between the left dlPFC of the FPN and right middle frontal gyrus. These findings support our hypothesis and parallel neuroimaging studies in civilian and military cohorts consistently reporting increased rsFC with lateral prefrontal regions in individuals with mTBI (Mayer et al., 2011; Stevens et al., 2012; Vakhtin et al., 2013), but decreased rsFC with lateral prefrontal cortex in PTSD (Koch et al., 2016; Misaki et al., 2018; Olson et al., 2018). To our knowledge, our study is the first to report divergent rsFC of prefrontal cortex in mTBI versus PTSD participants in the same study. In mTBI, heightened lateral prefrontal cortex activity and connectivity may contribute to common cognitive complaints, including greater distractibility and fatigue (McAllister et al., 2006). For instance, a rehabilitation study in participants with moderately severe TBI showed that activity of the lateral prefrontal cortex decreased after cognitive training focused on attention (Kim et al., 2008). Additional research will be necessary to investigate whether successful treatment of cognitive deficits in mTBI is associated with normalization of rsFC with the lateral prefrontal cortex.
Our findings of both overlapping and divergent rsFC in mTBI versus PTSD could have important clinical implications for diagnosis and treatment. For instance, we found similar reductions in rsFC of DMN and FPN regions in mTBI and PTSD. This overlap in the neural circuitry affected in both conditions may help explain why mTBI has been associated with an increased risk for developing PTSD (Bryant, 2008; Hoge et al., 2008; Yurgil et al., 2014). Consequently, it is possible that early interventions designed to target these networks, such as with cognitive rehabilitation or non-invasive brain stimulation, may help decrease the incidence of co-morbid PTSD in mTBI. Separately, we also identified opposite patterns of rsFC between the dlPFC of the FPN and right middle frontal gyrus in mTBI versus PTSD. Given the role of the lateral prefrontal cortex in executive functioning and emotion regulation (E. K. Miller, 2000; Ochsner et al., 2012; Seeley et al., 2007), either hypo- or hyper-connectivity with the middle frontal gyrus could contribute to cognitive and emotional impairments in both PTSD and mTBI.
Another important clinical consideration is whether rsFC analyses could be used in the future to differentiate between individuals with PTSD versus mTBI in a clinical setting. Recent research applying machine learning approaches to predict the diagnosis of individuals with different neurological and psychiatric disorders, including mTBI and PTSD, suggests this may be possible (Drysdale et al., 2016; Khazaee et al., 2016; Nicholson et al., 2019; Saccà et al., 2019; Vergara et al., 2016). For instance, using a linear support vector machine, Vergara et al. (2016) were able to classify mTBI participants using rsFC between cortical networks with an accuracy of 84.1%. Altogether this work indicates that rsFC may be a promising diagnostic tool to distinguish between mTBI and PTSD in military populations. However, a necessary step toward establishing the feasibility of this approach will be to determine whether machine learning algorithms using rsFC data can accurately classify individuals with mTBI versus PTSD in larger civilian and military cohorts.
There are limitations to the present study that should be mentioned. First, we reported differences in rsFC between individuals with mTBI versus PTSD only. Therefore, we could not address the combined effect of co-morbid mTBI+PTSD on rsFC. Second, our sample was comprised of more male than female participants, which could limit the generalizability of our results. Third, we recruited mTBI participants with persistent cognitive symptoms. It is possible that specific types of persistent postconcussive symptoms (e.g., cognitive versus affective) may be associated with alterations in different resting-state networks.
Conclusions
Consistent with previous research, Service Members with mTBI and PTSD exhibited diminished rsFC of DMN and FPN regions. Results of more diminished rsFC in DMN and FPN in PTSD suggest that severe PTSD symptoms may have a more consistent signal than mTBI. Our novel findings of opposite patterns of rsFC with lateral prefrontal cortex highlight a potential biomarker that could be used to differentiate between these conditions.
References
Andrews-Hanna, J. R., Snyder, A. Z., Vincent, J. L., Lustig, C., Head, D., Raichle, M. E., & Buckner, R. L. (2007). Disruption of large-scale brain Systems in Advanced Aging. Neuron, 56(5), 924–935. https://doi.org/10.1016/j.neuron.2007.10.038.
Bazarian, J. J., Donnelly, K., Peterson, D. R., Warner, G. C., Zhu, T., & Zhong, J. (2013). The relation between posttraumatic stress disorder and mild traumatic brain injury acquired during operations enduring freedom and Iraqi freedom. The Journal of Head Trauma Rehabilitation, 28(1), 1–12. https://doi.org/10.1097/HTR.0b013e318256d3d3.
Bliese, P. D., Wright, K. M., Adler, A. B., Cabrera, O., Castro, C. A., & Hoge, C. W. (2008). Validating the primary care posttraumatic stress disorder screen and the posttraumatic stress disorder checklist with soldiers returning from combat. Journal of Consulting and Clinical Psychology, 76(2), 272–281. https://doi.org/10.1037/0022-006X.76.2.272.
Bluhm, R. L., Williamson, P. C., Osuch, E. A., Frewen, P. A., Stevens, T. K., Boksman, K., Neufeld, R. W., Théberge, J., & Lanius, R. A. (2009). Alterations in default network connectivity in posttraumatic stress disorder related to early-life trauma. Journal of Psychiatry & Neuroscience : JPN, 34(3), 187–194 PMC.
Bolzenius, J. D., Velez, C. S., Lewis, J. D., Bigler, E. D., Wade, B. S., Cooper, D. B., Kennedy, J. E., Reid, M. W., Ritter, J. L., & York, G. E. (2018). Diffusion imaging findings in US service members with mild traumatic brain injury and posttraumatic stress disorder. The Journal of Head Trauma Rehabilitation, 33(6), 393–402.
Bonnelle, V., Ham, T. E., Leech, R., Kinnunen, K. M., Mehta, M. A., Greenwood, R. J., & Sharp, D. J. (2012). Salience network integrity predicts default mode network function after traumatic brain injury. Proceedings of the National Academy of Sciences, 109(12), 4690–4695. https://doi.org/10.1073/pnas.1113455109.
Boveroux, P., Vanhaudenhuyse, B. A., Bruno, B. M.-A., Noirhomme, Q., Lauwick, S., Luxen, A., Degueldre, C., Plenevaux, A., Schnakers, C., Phillips, C., Brichant, J.-F., Bonhomme, V., Maquet, P., Greicius, M. D., Laureys, S., & Boly, M. (2010). Breakdown of within- and between-network resting state functional magnetic resonance imaging connectivity during Propofol-induced loss of consciousness. Anesthesiology, 113(5), 1038–1053. https://doi.org/10.1097/ALN.0b013e3181f697f5.
Bryant, R. A. (2008). Disentangling mild traumatic brain injury and stress reactions. New England Journal of Medicine, 358(5), 525–527. https://doi.org/10.1056/NEJMe078235.
Carlson, K. F., Kehle, S. M., Meis, L. A., Greer, N., MacDonald, R., Rutks, I., Sayer, N. A., Dobscha, S. K., & Wilt, T. J. (2011). Prevalence, assessment, and treatment of mild traumatic brain injury and posttraumatic stress disorder: A systematic review of the evidence. The Journal of Head Trauma Rehabilitation, 26(2) https://journals.lww.com/headtraumarehab/Fulltext/2011/03000/Prevalence,_Assessment,_and_Treatment_of_Mild.1.aspx, 103–115.
Carp, J. (2012). The secret lives of experiments: Methods reporting in the fMRI literature. NeuroImage, 63(1), 289–300. https://doi.org/10.1016/j.neuroimage.2012.07.004.
Cicerone, K. D., & Kalmar, K. (1995). Persistent postconcussion syndrome: The structure of subjective complaints after mild traumatic brain injury. The Journal of Head Trauma Rehabilitation, 10(3), 1–17. https://doi.org/10.1097/00001199-199510030-00002.
Ciric, R., Wolf, D. H., Power, J. D., Roalf, D. R., Baum, G. L., Ruparel, K., Shinohara, R. T., Elliott, M. A., Eickhoff, S. B., Davatzikos, C., Gur, R. C., Gur, R. E., Bassett, D. S., & Satterthwaite, T. D. (2017). Benchmarking of participant-level confound regression strategies for the control of motion artifact in studies of functional connectivity. Cleaning up the FMRI Time Series: Mitigating Noise with Advanced Acquisition and Correction Strategies, 154(supplement C), 174–187. https://doi.org/10.1016/j.neuroimage.2017.03.020.
Cox, R. W. (1996). AFNI: Software for analysis and visualization of functional magnetic resonance Neuroimages. Computers and Biomedical Research, 29(3), 162–173. https://doi.org/10.1006/cbmr.1996.0014.
Disner, S. G., Marquardt, C. A., Mueller, B. A., Burton, P. C., & Sponheim, S. R. (2018). Spontaneous neural activity differences in posttraumatic stress disorder: A quantitative resting-state meta-analysis and fMRI validation. Human Brain Mapping, 39(2), 837–850. https://doi.org/10.1002/hbm.23886.
Dosenbach, N. U. F., Fair, D. A., Miezin, F. M., Cohen, A. L., Wenger, K. K., Dosenbach, R. A. T., Fox, M. D., Snyder, A. Z., Vincent, J. L., Raichle, M. E., Schlaggar, B. L., & Petersen, S. E. (2007). Distinct brain networks for adaptive and stable task control in humans. Proceedings of the National Academy of Sciences, 104(26), 11073–11078. https://doi.org/10.1073/pnas.0704320104.
Drysdale, A. T., Grosenick, L., Downar, J., Dunlop, K., Mansouri, F., Meng, Y., Fetcho, R. N., Zebley, B., Oathes, D. J., Etkin, A., Schatzberg, A. F., Sudheimer, K., Keller, J., Mayberg, H. S., Gunning, F. M., Alexopoulos, G. S., Fox, M. D., Pascual-Leone, A., Voss, H. U., et al. (2016). Resting-state connectivity biomarkers define neurophysiological subtypes of depression. Nature Medicine, 23, 28.
DVBIC (2018). DoD worldwide TBI numbers. https://health.mil/About-MHS/OASDHA/Defense-Health-Agency/Research-and-Development/Traumatic-Brain-Injury-Center-of-Excellence/DoD-TBI-Worldwide-Numbers.
Eklund, A., Nichols, T. E., & Knutsson, H. (2016). Cluster failure: Why fMRI inferences for spatial extent have inflated false-positive rates. Proceedings of the National Academy of Sciences, 113(28), 7900–7905. https://doi.org/10.1073/pnas.1602413113.
Fenster, R. J., Lebois, L. A. M., Ressler, K. J., & Suh, J. (2018). Brain circuit dysfunction in post-traumatic stress disorder: From mouse to man. Nature Reviews Neuroscience, 19(9), 535–551. https://doi.org/10.1038/s41583-018-0039-7.
Forman, S. D., Cohen, J. D., Fitzgerald, M., Eddy, W. F., Mintun, M. A., & Noll, D. C. (1995). Improved assessment of significant activation in functional magnetic resonance imaging (fMRI): Use of a cluster-size threshold. Magnetic Resonance in Medicine, 33(5), 636–647. https://doi.org/10.1002/mrm.1910330508.
Gilmore, C. S., Camchong, J., Davenport, N. D., Nelson, N. W., Kardon, R. H., Lim, K. O., & Sponheim, S. R. (2016). Deficits in visual system functional connectivity after blast-related mild TBI are associated with injury severity and executive dysfunction. Brain and Behavior, 6(5), e00454. https://doi.org/10.1002/brb3.454.
Hayes, J. P., Miller, D. R., Lafleche, G., Salat, D. H., & Verfaellie, M. (2015). The nature of white matter abnormalities in blast-related mild traumatic brain injury. NeuroImage: Clinical, 8, 148–156. https://doi.org/10.1016/j.nicl.2015.04.001.
Hoge, C. W., McGurk, D., Thomas, J. L., Cox, A. L., Engel, C. C., & Castro, C. A. (2008). Mild traumatic brain injury in U.S. soldiers returning from Iraq. New England Journal of Medicine, 358(5), 453–463. https://doi.org/10.1056/NEJMoa072972.
Khazaee, A., Ebrahimzadeh, A., & Babajani-Feremi, A. (2016). Application of advanced machine learning methods on resting-state fMRI network for identification of mild cognitive impairment and Alzheimer’s disease. Brain Imaging and Behavior, 10(3), 799–817. https://doi.org/10.1007/s11682-015-9448-7.
Kim, Y.-H., Yoo, W.-K., Ko, M.-H., Park, C., Kim, S. T., & Na, D. L. (2008). Plasticity of the Attentional network after brain injury and cognitive rehabilitation. Neurorehabilitation and Neural Repair, 23(5), 468–477. https://doi.org/10.1177/1545968308328728.
King, P. R., Donnelly, K. T., Donnelly, J. P., Dunnam, M., Warner, G., Kittleson, C. J., Bradshaw, C. B., Alt, M., & Meier, S. T. (2012). Psychometric study of the neurobehavioral symptom inventory. Journal of Rehabilitation Research and Development, 49(6), 879–888.
Koch, S. B. J., van Zuiden, M., Nawijn, L., Frijling, J. L., Veltman, D. J., & Olff, M. (2016). Aberrant resting-state brain activity in PTSD: A meta-analysis and systematic review. Depression and Anxiety, 33(7), 592–605. https://doi.org/10.1002/da.22478.
Lanius, R. A., Bluhm, R., Lanius, U., & Pain, C. (2006). A review of neuroimaging studies in PTSD: Heterogeneity of response to symptom provocation. Journal of Psychiatric Research, 40(8), 709–729. https://doi.org/10.1016/j.jpsychires.2005.07.007.
Levin, H. S., & Diaz-Arrastia, R. R. (2015). Diagnosis, prognosis, and clinical management of mild traumatic brain injury. The Lancet Neurology, 14(5), 506–517. https://doi.org/10.1016/S1474-4422(15)00002-2.
Levin, H. S., Wilde, E., Troyanskaya, M., Petersen, N. J., Scheibel, R., Newsome, M., Radaideh, M., Wu, T., Yallampalli, R., Chu, Z., & Li, X. (2010). Diffusion tensor imaging of mild to moderate blast-related traumatic brain injury and its Sequelae. Journal of Neurotrauma, 27(4), 683–694. https://doi.org/10.1089/neu.2009.1073.
Mac Donald, C. L., Adam, O. R., Johnson, A. M., Nelson, E. C., Werner, N. J., Rivet, D. J., & Brody, D. L. (2015). Acute post-traumatic stress symptoms and age predict outcome in military blast concussion. Brain, 138(5), 1314–1326. https://doi.org/10.1093/brain/awv038.
Mayer, A. R., Mannell, M. V., Ling, J., Gasparovic, C., & Yeo, R. A. (2011). Functional connectivity in mild traumatic brain injury. Human Brain Mapping, 32(11), 1825–1835. https://doi.org/10.1002/hbm.21151.
McAllister, T. W., Flashman, L. A., McDonald, B. C., & Saykin, A. J. (2006). Mechanisms of working memory dysfunction after mild and moderate TBI: Evidence from functional MRI and Neurogenetics. Journal of Neurotrauma, 23(10), 1450–1467. https://doi.org/10.1089/neu.2006.23.1450.
McDonald, B. C., Saykin, A. J., & McAllister, T. W. (2012). Functional MRI of mild traumatic brain injury (mTBI): Progress and perspectives from the first decade of studies. Brain Imaging and Behavior, 6(2), 193–207. https://doi.org/10.1007/s11682-012-9173-4.
Miller, E. K. (2000). The prefontral cortex and cognitive control. Nature Reviews Neuroscience, 1(1), 59–65. https://doi.org/10.1038/35036228.
Miller, D. R., Hayes, S. M., Hayes, J. P., Spielberg, J. M., Lafleche, G., & Verfaellie, M. (2017). Default mode network subsystems are differentially disrupted in posttraumatic stress disorder. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, 2(4), 363–371. https://doi.org/10.1016/j.bpsc.2016.12.006.
Misaki, M., Phillips, R., Zotev, V., Wong, C.-K., Wurfel, B. E., Krueger, F., Feldner, M., & Bodurka, J. (2018). Connectome-wide investigation of altered resting-state functional connectivity in war veterans with and without posttraumatic stress disorder. NeuroImage: Clinical, 17, 285–296. https://doi.org/10.1016/j.nicl.2017.10.032.
Morey, R. A., Haswell, C. C., Selgrade, E. S., Massoglia, D., Liu, C., Weiner, J., Marx, C. E., MIRECC Work Group, Cernak, I., & McCarthy, G. (2013). Effects of chronic mild traumatic brain injury on white matter integrity in Iraq and Afghanistan war veterans. Human Brain Mapping, 34(11), 2986–2999. https://doi.org/10.1002/hbm.22117.
Mueller-Pfeiffer, C., Schick, M., Schulte-Vels, T., O’Gorman, R., Michels, L., Martin-Soelch, C., Blair, J. R., Rufer, M., Schnyder, U., Zeffiro, T., & Hasler, G. (2013). Atypical visual processing in posttraumatic stress disorder. NeuroImage: Clinical, 3, 531–538. https://doi.org/10.1016/j.nicl.2013.08.009.
Nicholson, A. A., Densmore, M., McKinnon, M. C., Neufeld, R. W. J., Frewen, P. A., Théberge, J., Jetly, R., Richardson, J. D., & Lanius, R. A. (2019). Machine learning multivariate pattern analysis predicts classification of posttraumatic stress disorder and its dissociative subtype: A multimodal neuroimaging approach. In Psychological medicine, 49(12), 2049–2059 (Vol. 49, pp. 2049–2059). Cambridge: Core. https://doi.org/10.1017/S0033291718002866.
Ochsner, K. N., Silvers, J. A., & Buhle, J. T. (2012). Functional imaging studies of emotion regulation: A synthetic review and evolving model of the cognitive control of emotion. Annals of the New York Academy of Sciences, 1251(1), E1–E24. https://doi.org/10.1111/j.1749-6632.2012.06751.x.
Olson, E, A., Kaiser, R, H., Pizzagalli, D, A., Rauch, S, L., & Rosso, I, M. (2018). Regional prefrontal resting-state functional connectivity in posttraumatic stress disorder. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging. https://doi.org/10.1016/j.bpsc.2018.09.012.
Palacios, E. M., Yuh, E. L., Chang, Y.-S., Yue, J. K., Schnyer, D. M., Okonkwo, D. O., Valadka, A. B., Gordon, W. A., Maas, A. I. R., Vassar, M., Manley, G. T., & Mukherjee, P. (2017). Resting-state functional connectivity alterations associated with six-month outcomes in mild traumatic brain injury. Journal of Neurotrauma, 34(8), 1546–1557. https://doi.org/10.1089/neu.2016.4752.
Philippi, C. L., Pujara, M. S., Motzkin, J. C., Newman, J., Kiehl, K. A., & Koenigs, M. (2015). Altered resting-state functional connectivity in cortical networks in psychopathy. The Journal of Neuroscience, 35(15), 6068–6078. https://doi.org/10.1523/JNEUROSCI.5010-14.2015.
Polusny, M. A., Kehle, S. M., Nelson, N. W., Erbes, C. R., Arbisi, P. A., & Thuras, P. (2011). Longitudinal effects of mild traumatic brain injury and posttraumatic stress disorder comorbidity on Postdeployment outcomes in National Guard Soldiers Deployed to IraqLongitudinal effects of traumatic brain injury. Archives of General Psychiatry, 68(1), 79–89. https://doi.org/10.1001/archgenpsychiatry.2010.172.
Power, J. D., Schlaggar, B. L., & Petersen, S. E. (2015). Recent progress and outstanding issues in motion correction in resting state fMRI. NeuroImage, 105(supplement C), 536–551. https://doi.org/10.1016/j.neuroimage.2014.10.044.
Radloff, L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. https://doi.org/10.1177/014662167700100306.
Raji, C. A., Willeumier, K., Taylor, D., Tarzwell, R., Newberg, A., Henderson, T. A., & Amen, D. G. (2015). Functional neuroimaging with default mode network regions distinguishes PTSD from TBI in a military veteran population. Brain Imaging and Behavior, 9(3), 527–534. https://doi.org/10.1007/s11682-015-9385-5.
Rauch, S. L., van der Kolk, B. A., Fisler, R. E., Alpert, N. M., Orr, S. P., Savage, C. R., Fischman, A. J., Jenike, M. A., & Pitman, R. K. (1996). A symptom provocation study of posttraumatic stress disorder using positron emission tomography and script-driven imagery. JAMA Psychiatry, 53(5), 380–387. https://doi.org/10.1001/archpsyc.1996.01830050014003.
Reid, M. W., & Velez, C. S. (2015). Discriminating military and civilian traumatic brain injuries. Traumatic Brain Injury, 66, 123–128. https://doi.org/10.1016/j.mcn.2015.03.014.
Rosenbaum, S. B., & Lipton, M. L. (2012). Embracing chaos: The scope and importance of clinical and pathological heterogeneity in mTBI. Brain Imaging and Behavior, 6(2), 255–282. https://doi.org/10.1007/s11682-012-9162-7.
Rowland, J. A., Stapleton-Kotloski, J. R., Alberto, G. E., Rawley, J. A., Kotloski, R. J., Taber, K. H., & Godwin, D. W. (2016). Contrasting effects of posttraumatic stress disorder and mild traumatic brain injury on the whole-brain resting-state network: A Magnetoencephalography study. Brain Connectivity, 7(1), 45–57. https://doi.org/10.1089/brain.2015.0406.
Saccà, V., Sarica, A., Novellino, F., Barone, S., Tallarico, T., Filippelli, E., Granata, A., Chiriaco, C., Bruno Bossio, R., Valentino, P., & Quattrone, A. (2019). Evaluation of machine learning algorithms performance for the prediction of early multiple sclerosis from resting-state FMRI connectivity data. Brain Imaging and Behavior, 13(4), 1103–1114. https://doi.org/10.1007/s11682-018-9926-9.
Santhanam, P., Wilson, S. H., Oakes, T. R., & Weaver, L. K. (2019). Effects of mild traumatic brain injury and post-traumatic stress disorder on resting-state default mode network connectivity. Brain Research, 1711, 77–82. https://doi.org/10.1016/j.brainres.2019.01.015.
Schneiderman, A. I., Braver, E. R., & Kang, H. K. (2008). Understanding Sequelae of injury mechanisms and mild traumatic brain injury incurred during the conflicts in Iraq and Afghanistan: Persistent Postconcussive symptoms and posttraumatic stress disorder. American Journal of Epidemiology, 167(12), 1446–1452. https://doi.org/10.1093/aje/kwn068.
Schuff, N., Zhang, Y., Zhan, W., Lenoci, M., Ching, C., Boreta, L., Mueller, S. G., Wang, Z., Marmar, C. R., Weiner, M. W., & Neylan, T. C. (2011). Patterns of altered cortical perfusion and diminished subcortical integrity in posttraumatic stress disorder: An MRI study. International Brain Mapping & Intraoperative Surgical Planning Society (IBMISPS)2009 Supplement, 54, S62–S68. https://doi.org/10.1016/j.neuroimage.2010.05.024.
Seeley, W. W., Menon, V., Schatzberg, A. F., Keller, J., Glover, G. H., Kenna, H., Reiss, A. L., & Greicius, M. D. (2007). Dissociable intrinsic connectivity networks for salience processing and executive control. The Journal of Neuroscience, 27(9), 2349–2356. https://doi.org/10.1523/JNEUROSCI.5587-06.2007.
Shandera-Ochsner, A. L., Berry, D. T. R., Harp, J. P., Edmundson, M., Graue, L. O., Roach, A., & High, W. M. (2013). Neuropsychological effects of self-reported deployment-related mild TBI and current PTSD in OIF/OEF veterans. The Clinical Neuropsychologist, 27(6), 881–907. https://doi.org/10.1080/13854046.2013.802017.
Shang, J., Lui, S., Meng, Y., Zhu, H., Qiu, C., Gong, Q., Liao, W., & Zhang, W. (2014). Alterations in low-level perceptual networks related to clinical severity in PTSD after an earthquake: A resting-state fMRI study. PLoS One, 9(5), e96834. https://doi.org/10.1371/journal.pone.0096834.
Slobounov, S. M., Gay, M., Zhang, K., Johnson, B., Pennell, D., Sebastianelli, W., Horovitz, S., & Hallett, M. (2011). Alteration of brain functional network at rest and in response to YMCA physical stress test in concussed athletes: RsFMRI study. NeuroImage, 55(4), 1716–1727. https://doi.org/10.1016/j.neuroimage.2011.01.024.
Snell, F. I., & Halter, M. J. (2010). A signature wound of war. Journal of Psychosocial Nursing and Mental Health Services, 48, 1–7. https://doi.org/10.3928/02793695-20100108-02.
Sours, C., Zhuo, J., Janowich, J., Aarabi, B., Shanmuganathan, K., & Gullapalli, R. P. (2013). Default mode network interference in mild traumatic brain injury – A pilot resting state study. Brain Research, 1537, 201–215. https://doi.org/10.1016/j.brainres.2013.08.034.
Sripada, R. K., King, A. P., Welsh, R. C., Garfinkel, S. N., Wang, X., Sripada, C. S., & Liberzon, I. (2012). Neural Dysregulation in posttraumatic stress disorder: Evidence for disrupted equilibrium between salience and default mode brain networks. Psychosomatic Medicine, 74(9), 904–911. PMC. https://doi.org/10.1097/PSY.0b013e318273bf33.
Stevens, M. C., Lovejoy, D., Kim, J., Oakes, H., Kureshi, I., & Witt, S. T. (2012). Multiple resting state network functional connectivity abnormalities in mild traumatic brain injury. Brain Imaging and Behavior, 6(2), 293–318. https://doi.org/10.1007/s11682-012-9157-4.
Vakhtin, A. A., Calhoun, V. D., Jung, R. E., Prestopnik, J. L., Taylor, P. A., & Ford, C. C. (2013). Changes in intrinsic functional brain networks following blast-induced mild traumatic brain injury. Brain Injury, 27(11), 1304–1310. https://doi.org/10.3109/02699052.2013.823561.
Vasterling, J. J., Brailey, K., Proctor, S. P., Kane, R., Heeren, T., & Franz, M. (2012). Neuropsychological outcomes of mild traumatic brain injury, post-traumatic stress disorder and depression in Iraq-deployed US Army soldiers. In British Journal of psychiatry, 201(3), 186–192 (Vol. 201, pp. 186–192). Cambridge: Core. https://doi.org/10.1192/bjp.bp.111.096461.
Verfaellie, M., Lafleche, G., Spiro, A., & Bousquet, K. (2014). Neuropsychological outcomes in OEF/OIF veterans with self-report of blast exposure: Associations with mental health, but not MTBI. Neuropsychology, 28(3), 337–346. https://doi.org/10.1037/neu0000027.
Vergara, V. M., Mayer, A. R., Damaraju, E., Kiehl, K. A., & Calhoun, V. (2016). Detection of mild traumatic brain injury by machine learning classification using resting state functional network connectivity and fractional anisotropy. Journal of Neurotrauma, 34(5), 1045–1053. https://doi.org/10.1089/neu.2016.4526.
Wang, T., Liu, J., Zhang, J., Zhan, W., Li, L., Wu, M., Huang, H., Zhu, H., Kemp, G. J., & Gong, Q. (2016). Altered resting-state functional activity in posttraumatic stress disorder: A quantitative meta-analysis. Scientific Reports, 6, 27131.
Yurgil, K., Barkauskas, D., Vasterling, J., et al. (2014). Association between traumatic brain injury and risk of posttraumatic stress disorder in active-duty marines. JAMA Psychiatry, 71(2), 149–157. https://doi.org/10.1001/jamapsychiatry.2013.3080.
Zhang, J., Tan, Q., Yin, H., Zhang, X., Huan, Y., Tang, L., Wang, H., Xu, J., & Li, L. (2011). Decreased gray matter volume in the left hippocampus and bilateral calcarine cortex in coal mine flood disaster survivors with recent onset PTSD. Psychiatry Research: Neuroimaging, 192(2), 84–90. https://doi.org/10.1016/j.pscychresns.2010.09.001.
Zhou, Y., Milham, M. P., Lui, Y. W., Miles, L., Reaume, J., Sodickson, D. K., Grossman, R. I., & Ge, Y. (2012). Default-mode network disruption in mild traumatic brain injury. Radiology, 265(3), 882–892. https://doi.org/10.1148/radiol.12120748.
Zhu, H., Zhang, J., Zhan, W., Qiu, C., Wu, R., Meng, Y., Cui, H., Huang, X., Li, T., Gong, Q., & Zhang, W. (2014). Altered spontaneous neuronal activity of visual cortex and medial anterior cingulate cortex in treatment-naïve posttraumatic stress disorder. Comprehensive Psychiatry, 55(7), 1688–1695. https://doi.org/10.1016/j.comppsych.2014.06.009.
Acknowledgments
We thank the Service Members for their generous time and effort in making this research possible. We also recognize the clinical effort and expertise of the Brooke Army Medical Center Brain Injury and Rehabilitation Service staff in the recruitment, consenting, and treatment of Service Members involved in this study. The view(s) expressed herein are those of the authors and do not reflect the official policy or position of the Defense and Veterans Brain Injury Center, Brooke Army Medical Center, the US Army Medical Department, the US Army Office of the Surgeon General, the Department of the Army, the Department of the Air Force, Department of Defense, or the US Government.
Funding sources
This work was supported in part by the Defense and Veterans Brain Injury Centers, the U.S. Army Medical Research and Materiel Command (USAMRMC; W81XWH-13-2-0025) and the Chronic Effects of Neurotrauma Consortium (CENC; PT108802-SC104835).
Availability of data
Data are available from the first author upon request.
Author information
Authors and Affiliations
Contributions
Author contributions included: Conceptualization, C.L.P., D.F.T.; Methodology, C.L.P., D.F.T., C.S.V., B.S.C.W.; Investigation, C.S.V., A.M.D., A.O.B., D.B.C., J.E.K., J.D.L., M.W.R., G.E.Y., E.A.W., D.F.T.; Formal Analysis, C.L.P., C.S.V, D.F.T.; Writing – Original Draft, C.L.P, D.F.T.; Writing – Review & Editing, C.L.P, C.S.V., B.S.C.W., A.M.D., D.B.C., J.E.C., J.E.K., A.O.B., J.D.L., M.W.R., G.E.Y., M.R.N., E.A.W., D.F.T.; Visualization, C.L.P. All authors take responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding authors
Ethics declarations
Compliance with ethical standards
The research was approved by the Institutional Review Boards at the Brooke Army Medical Center and University of Missouri-St. Louis and written informed consent was obtained from all study subjects prior to their participation. Privacy and confidentiality were maintained by deidentifying all data and giving each participant a unique subject ID.
Conflict of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 31 kb)
Rights and permissions
About this article
Cite this article
Philippi, C.L., Velez, C.S., Wade, B.S. et al. Distinct patterns of resting-state connectivity in U.S. service members with mild traumatic brain injury versus posttraumatic stress disorder. Brain Imaging and Behavior 15, 2616–2626 (2021). https://doi.org/10.1007/s11682-021-00464-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11682-021-00464-1