Abstract
We investigated potential brain volumetric differences in a sample of former high school football players many years after these injuries. Forty community-dwelling males ages 40–65 who played high school football, but not college or professional sports, were recruited. The experimental group (n = 20) endorsed experiencing two or more mTBIs on an empirically validated mTBI assessment tool (median = 3, range = 2–15). The control group (n = 20) denied ever experiencing an mTBI. Participants completed a self-report index of current mTBI symptomatology and underwent high-resolution T1-weighted MRI scanning, which were analyzed using the Freesurfer software package. A priori regions of interest (ROIs) included total intracranial volume (ICV), total gray matter, total white matter, bilateral anterior cingulate cortex, bilateral hippocampi, and lateral ventricles. ROIs were corrected for head size using a normalization method that took ICV into account. Despite an adequate sample size and being matched on age, education, estimated premorbid IQ, current concussive symptomatology, there were no statistically significant volumetric group differences across all of the ROIs. These data suggest that multiple mTBIs from high school football may not be associated with measurable brain atrophy later in life. Accounting for the severity of injury and chronicity of sport exposure may be especially important when measuring long-term neuroanatomical differences.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction and literature review
Mild traumatic brain injuries (mTBI) are common, as over 75% of the 1.7 million traumatic brain injuries in the United States each year are classified as mild using a Glasgow Coma Scale score between 13 and 15 (CDC 2010; Faul et al. 2010). The symptoms of an mTBI are clinically heterogeneous, typically manifesting as a variety of cognitive (e.g. reduced attention and memory), somatic (e.g. headaches, dizziness, nausea), affective (e.g. sad, emotionally labile), and sleep-related difficulties (CDC 2010; McCrory et al. 2009; Arciniegas et al. 2000; Hall et al. 2005). However, accurate diagnosis of an mTBI can be difficult due to the lack of radiological evidence of a brain injury, as the brain is frequently deemed to be normal on traditional brain imaging modalities such as computerized tomography (CT) and magnetic resonance imaging (MRI) (e.g., Bazarian et al. 2007; Hughes et al. 2004; Iverson et al. 2000). Thus, the diagnosis of an mTBI is typically based on self-reported clinical and cognitive symptoms following head trauma. This can be problematic as the symptoms of an mTBI are nonspecific and can occur in a variety of other medical and psychological conditions (Stein and McAllister 2009).
There may be ways to improve the sensitivity of neuroimaging methods to detect brain abnormalities sustained related to an mTBI. There is evidence that there are, in fact, pathophysiological changes associated with an mTBI, as autopsy studies have suggested that some who have experienced an mTBI with negative radiological findings have microscopic axonal injuries (Bigler 2004; Blumbergs et al. 1994). These changes are likely the result of the mechanical impact of the head injury. Rapid acceleration and deceleration forces related to the concussive event are thought to stretch, twist, and shear axons or cause alterations in cell function that manifest as the acute symptoms of an mTBI (Blennow et al. 2012). Magnetic resonance imaging (MRI) scans show promise in detecting these abnormalities, as they are more sensitive in detecting white matter shearing, small subacute hemorrhages, small contusions, and small foci of axonal injury as compared to CT (see Niogi and Mukherjee 2010). MRI can also better differentiate brain and CSF as well as edema as compared to CT scans (Johnston et al. 2001), which are important considerations when evaluating mTBI using imaging modalities.
Several studies have suggested chronic (i.e. greater than six months post injury) differences in brain volume following a concussion, such as decreased overall brain volume (Gale et al. 1995; MacKenzie et al. 2002). Further, these studies suggested that loss of consciousness and worse neurocognitive functioning was associated with smaller brain volumes in the patient groups. Symptomatic patients with an mTBI at an average of two years post-injury had a higher rate of atrophy in forebrain parenchyma, cerebral white matter, and cerebellar volume compared to controls at two different time points (Ross et al. 2012). Cortical thinning in the left superior temporal and left superior frontal gyri was shown in veterans with blast-related mTBI within 18-months of injury (Tate et al. 2014), which was associated with abnormal language and audition scores on behavioral measures.
Longitudinal studies of neuroanatomical changes in mTBI have produced mixed findings. A group of people with a documented mTBI in an emergency department setting exhibited global brain atrophy compared to a control group on longitudinal scans taken acutely after the mTBI and again at 1-year post-injury (Zhou et al. 2013). In collegiate hockey players, global volume reductions were noted at 2-weeks and 2-months post- concussion (Jarrett et al. 2016). Region of interest analyses indicated reduced gray matter volume in the precuneus and white matter volume in the anterior cingulate, which correlated with memory and attention performance (Zhou et al. 2013). Hofman et al. (2001) showed that when scanned again at six months post-injury, patients with abnormal MRIs had a greater rate of brain atrophy than those without MRI abnormalities. In another study, the patient group had abnormally rapid atrophy in whole brain parenchyma and cerebral white matter between the time of the injury and an average of 1.7 years later, while the cerebellum and brainstem enlarged rapidly over the first year and a half and then diminished over the following year, suggesting that different brain regions are affected by a TBI in different ways (Ross et al. 2014). However, in a study examining ventricular volume, gray matter volume, and cortical thickness during the acute (i.e. within three weeks) and semi-acute phase of recovery (i.e. four months later), there were no significant differences between the mTBI group and a matched control group (Ling et al. 2013). Examining specific bran regions has also showed differences associated with mTBI. Monti et al. (2013) found that those who experienced a medically diagnosed mTBI before the age of 25 years old had smaller bilateral hippocampi compared to well-matched control participants at an average of 30 years post-injury. They also found that this sample did worse on a face-scene relational memory task and had less functional MRI activity in memory-related regions in the parietal and prefrontal cortices. However, these differences were not evident in younger samples after an average of four years post-injury (Monti et al. 2013), suggesting that these subcortical changes may take place over a longer amount of time.
Many of the studies presented thus far have been conducted in medical populations, where a concussion may occur at one discrete time point. However, athletes that play contact sports may have different brain changes in response to a concussion due to the accumulation of chronic impact to the head. In a sample of current college football players, participants that experienced a clinician-diagnosed mTBI had smaller bilateral hippocampi compared to a sample of non-concussed teammates as well as a sample of non-concussed non-athletes at a post-injury period ranging from 1 day to 4.5 years (Singh et al. 2014). Additionally, the non-concussed football players had smaller bilateral hippocampi compared to the control group, suggesting that the sub-concussive impact associated with football may have an impact on brain structure. The time players reported engaging in football was negatively correlated with hippocampal volume suggestive of a dose-response relationship (Singh et al. 2014).
More chronic changes have also been documented in sports-related mTBI. Cortical thinning of the right temporal lobe and left insula was seen in a sample of young adult athletes with multiple concussions who had not had a concussion in the past 6-months as compared to non-concussed controls (List et al. 2015). Former college athletes ages 50–75 who experienced between one and five concussions (average = 2.08) before their mid-20s showed cortical thinning in various areas, lateral ventricular enlargement, and worse memory performance when compared to their non-concussed teammates (Tremblay et al. 2013). Similar cohorts of middle-aged former athletes with remote concussions have also been showed to have differences in event-related potentials (Broglio et al. 2012; De Beaumont et al. 2009) and white matter integrity (Hart et al. 2013; Tremblay et al. 2014; see Henry et al. 2016 for review). These findings resemble patterns of abnormal aging reflected in neurodegenerative conditions often seen later in life.
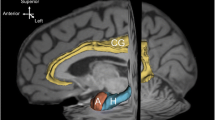
We extended the current literature with our examination of former high school football players who had at least two mild TBIs related to their high school football experiences. However, these former athletes have not received a concussion since that time, a period of at least fifteen years. We compared the concussed group to a matched group of control participants who also played high school football but do not have a history of concussive injuries. We also examined how these injuries may be related to worse cognitive performance. We used high-resolution FSPGR MRI scans from a 3-Tesla imaging system to elucidate volumetric differences between the past-concussed group and the control group with a priori hypotheses that the past-concussion group would have less total brain volume (i.e. intracranial volume, ICV), total white matter volume, total gray matter volume, hippocampal volume, anterior cingulate volume, and lateral ventricular volume compared to the control group. Further, we explored two brain-behavior correlations: the relationship between hippocampal volume with memory functioning based on previous studies implicating medial temporal lobe structures are related to delayed recall (Tremblay et al. 2013), as well as between gray matter volume and overall cognitive functioning based on previous aging literature showing this broad relationship (Kramer et al. 2007).
Method
Participants
Data collection for this study began in 2012 as part of a larger dataset. Preliminary functional MRI data were previously published on a subset of these participants (Terry et al. 2015). Recruitment took place through newspaper and online advertisements, news articles about the study, or public records and football alumni listservs. Participants were included if they were right-handed, male, and aged 40–65 years. This age range was selected to maximize the number of participants who may have sustained a concussion in their remote history, but limit the frequency of people who by virtue of their age may be experiencing symptoms of a Minor or Major Neurocognitive disorder, as this could be a confounding factor. Participants were excluded if they reported: being incompatible with the MRI environment, being illiterate, learning English as a second language, a history of alcohol or drug abuse/dependency within the past five years, a history of a neurological disorder (e.g., seizures, epilepsy), a history of a developmental learning disorder (e.g. learning disability, ADD, ADHD), current use of any psychotropic medications, or a diagnosis of bipolar disorder or schizophrenia. One hundred and forty-five potential participants were screened, from which 45 were successfully recruited and consented by signing an Institutional Review Board approved consent form. Of these participants, imaging data is only available for 40 participants (i.e. n = 20 for each group) due to claustrophobia and late-identified MRI incompatibility. Participants were given a small stipend ($50) for their participation.
Participants were divided into two groups: one with a history of two or greater concussions in the context of their high school football experiences but no other lifetime concussions (total n = 25; imaging n = 20); and one without any concussive history (total n = 20; imaging n = 20). Concussions were identified through two ways. First, participants completed an in-house self-report questionnaire regarding concussive history aimed at validating the presence of at least two concussions in the context of high school football based on criteria set by the American Congress of Rehabilitation Medicine (Medicine 1993), where a mTBI was suspected when at least one of the following criteria was met after an injury involving the head: (1) any period of loss of consciousness; (2) any loss of memory for events immediately before or after the accident; (3) any alteration in mental state at the time of the accident (e.g. feeling dazed, disoriented or confused) and (4) focal neurological deficit(s) that may or may not be transient (Medicine 1993; Cassidy et al., 2004). Participants were then administered the Acute Concussion Evaluation (ACE; Gioia and Collins 2006), a systematic evidence-based clinical protocol designed to assess 1) the specific characteristic of the injury including the details of the blow to the head, 2) a full array of 22 symptoms and 5 signs associated with mTBI, and 3) risk factors that might predict a prolonged recovery. The ACE was shown to have moderate to high internal consistency (α = 0.82) and adequate content, predictive, and convergent validity when compared to other concussion assessments (Gioia et al. 2008). Previous studies using retrospective reporting showed adequate recall of remote historical events with acceptable one-month test-retest reliability (Kendler et al. 2008; Moffitt et al. 2007). Participants were excluded if they reported exactly one concussion or enduring a concussion outside of high school football. The non-concussed group denied a lifetime history of concussions.
All participants completed a concussion symptom checklist to index current post-concussive symptoms, if any, as this could have been a potential confound in the neuroimaging analysis. The Symptom Assessment Scale (SAS) is a 22-item symptom list where the participant first answers “yes” or “no” as to whether they have experienced any of the symptoms over the past 24 h. For those symptoms positively endorsed, they rank both the duration and the severity of each system over the past 24 h using a Likert scale (0 to 6); the maximum total score is 132 on each of the two sub-scales (Broglio et al. 2007). The severity sub-scale is anchored with not severe at all and as severe as possible, and the duration scale is anchored with briefly and always.
The Repeatable Battery for the Assessment of Neuropsychological Status (RBANS) was used to assess cognitive functioning (Randolph et al. 1998). A total of 12 subtests are used to generate 5 index scores (i.e., Visuospatial/Constructional, Attention, Language, Immediate Memory, and Delayed Memory) and one Overall Scaled Score for the whole test. Raw scores are converted to standard scores (i.e., mean = 100, standard deviation = 15) based on age (Fig. 1).
Neuroimaging
All images were acquired using a General Electric (GE; Waukesha, WI) Signa HDx 3 T MRI. This scanner is equipped with 16 RF receiver channels with TQ Engine gradients (amplitude, 45 mT/m [z-axis], 40 mT/m [x, y-axes]; slew rate, 200 T/m/s) and an 8-channel head coil. 3D structural scans were acquired using a fast spoiled gradient recalled echo (FSPGR) protocol; TE ≤ = 2 ms, TR = 7.5 ms, flip angle =20°, 154 axial slices, slice thickness = 1 mm, and FOV = 256 × 256 mm. These images cover from the top of the head to the brainstem. Acquisition time for this sequence was 6 min 20 s. Total scanning time was approximately 55 min.
Volumetric MRI analysis
Automated segmentation of cortical and subcortical regions was conducted using Freesurfer (version 5.1). Details of these segmentation processes are available in Fischl et al. (2002, 2004a). This automated method has been shown to be statistically indistinguishable from the manual tracing of cortical and subcortical structures (Fischl et al. 2002) and has been shown to be sensitive to volumetric differences between groups (Morey et al. 2009). Additionally, it is relatively insensitive to changes in acquisition parameters (Fischl et al. 2004b), making this procedure robust and generalizable across different research settings. While studies show differences in Freesurfer analyses across scanner platforms (Wilde et al. 2016), this is likely not problematic in the present study given we only used one scanner.
An automated measure of total intracranial volume (ICV) was also used in conjunction with the Freesurfer package (Buckner et al. 2004). Extracting ICV using this method has also been shown to be comparable to manual tracing. This volume served as both a dependent measure as well as a way to correct ROIs for overall head size. Total gray matter volume and white matter volume were extracted directly from the Freesurfer output. The anterior cingulate cortex comprised the volumes labeled the caudal anterior cingulate and rostral anterior cingulate. Our hypotheses were not hemisphere specific, so the left and right volumes for the hippocampus, lateral ventricles, and anterior cingulate (i.e., caudal + rostral) were summed to represent their respective bilateral structures. To control for ROIs, the slope (b) of the ROI volume was regressed onto the ICV. That variable was entered into the following equation to normalize each ROI for head size:
This correction procedure has been used in multiple studies that have extracted subcortical volumes and is less affected by systematic and random error compared to other normalization methods (e.g. Erickson et al. 2009; Head et al. 2008; Sanfilipo et al. 2004)
Behavioral data analysis
Data were analyzed using the Statistical Package for Social Sciences (SPSS version 21.0). Between-groups independent samples t-test were conducted at a significance threshold of p < .01, which is corrected to control for multiple comparisons. The following t-tests were run between the concussed group and control groups: 1) whole brain volume, 2) normalized white matter volume, 3) normalized gray matter volume, 4) normalized bilateral hippocampal volume, 5) normalized bilateral anterior cingulate volume, 6) normalized bilateral lateral ventricle volume. We also calculated Pearson correlation coefficients for two hypothesized relationships: between normalized bilateral hippocampal volume and RBANS Delayed Memory, and between normalized gray matter volume and RBANS Total Score, for each group.
Results
When comparing the previously concussed group with the non-concussed group, there were no statistically significant differences with respect to age [t(38) = 1.31, p = 0.20], years of formal education [t(38) = 0.59, p = 0.56], and pre-morbid IQ level as measured by the Wechsler Test of Adult Reading [t(38) = 0.49, p = 0.63] based on independent samples t-test analyses (Table 1). On the SAS, both participant groups reported experiencing a modest number of symptoms over the previous 24 h (previously concussed group M = 4.6; non-concussed group M = 3.6) similar to rates of baseline symptom reporting in other studies (Piland et al. 2010). However, there were no group differences in the total number of symptoms reported [t(38) = 0.85, p = 0.40], the duration of those symptoms over the past 24 h [t(38) = 1.17, p = 0.25], or the symptom severity [t(38) = 1.49, p = 0.14]. There were no between-group differences on cognitive variables from the RBANS (see Table 1). Time since the most recent injury was M = 36.7 years (SD = 7.2, range = 25–44).
Independent t-test analysis comparing whole brain volume between the concussed and the control groups was not significant [t(38) = 0.029, p = .98] (Table 2). The average ICV for the sample was 1,405,323 mm3, which was used to calculate the normalized volumes for each of the ROIs. There were no statistically significant differences in volumes between the two groups when comparing overall gray matter volume [t(38) = 0.451, p = .65], overall white matter volume [t(38) = 0.432, p = .66], bilateral lateral ventricles [t(38) = −0.538, p = .59], bilateral anterior cingulate volume [t(38) = 0.509, p = .61], or bilateral hippocampal volume [t(38) = 0.033, p = .74]. Given the potential influence of other variables, we employed an analysis of covariance (ANCOVA) to ensure that age did not affect the relationship between group status and volumes. Covarying for age, ANCOVAs did not reveal any statistically significant group differences (all p-values > .05).
In exploratory post-hoc analyses, we sought to examine if there was a differential relationship between cognition and brain volumes. Using bivariate Pearson correlations, bilateral hippocampal volumes were not correlated with the Delayed Memory index score on the RBANS for the concussed group [r = −.03, p = .90] or the control group [r = .12, p = .62]. However, better overall cognitive functioning was related to more adjusted gray matter volume in both groups [concussed: r = .53, p = .01; control: r = .44, p = .06]. There was not a statistically significant difference when comparing this relationship between groups [z = 0.032, p = .37].
Discussion
Results of our study suggest a lack of volume differences in the brains of middle-aged men who experienced multiple mTBIs compared to those without mTBIs in the context of their high school football careers. This lack of volumetric differences was seen in both overall intracranial volume as well as in specific regions that have previously been associated with smaller volumes such as overall gray matter, white matter, lateral ventricles, the anterior cingulate, and the hippocampus.
It important to understand the sample recruited for this study in the context of its null results. The individuals in this study were community dwelling and actively recruited to take place in this research study based on local advertisements and historical records. This sample may be different than previous studies that recruited participants who sought professional medical attention or experienced loss of consciousness (e.g., Monti et al. 2013). Further, the mTBI group participants cumulatively reported only receiving medical attention after 31% of their concussions. Thus, our sample may represent more mild cases on the spectrum of what could be classified as an mTBI. Also unlike some previous studies, the mTBI group was not experiencing a statistically different number of concussion-like symptoms as compared to the non-mTBI control group, nor were they labeled as having abnormal MRI findings from a clinical brain scan at the time of the injury (e.g., Hofman et al. 2001). Further, this sample assessed participants more remotely than many of the previous studies that reported positive findings (e.g., Singh et al. 2014). Thus, it is possible that frank neuronal loss may only occur in the context of chronically symptomatic individuals or in the presence of positive imaging findings.
Statistical power to detect differences is important to consider in a study reporting a lack of statistically significant findings. An a priori power analysis calculated that a sample size of 38 (i.e. 19 per group) would achieve a power of .80 based on the effect sizes of previous empirical studies that examined gross anatomic volumes (e.g. whole brain parenchyma, cortical gray matter, cortical white matter; Ross et al. 2012) and hippocampal volume (Monti et al. 2013; Singh et al. 2014). This value is consistent with the typical sample sizes of the literature in this field, as similar studies with group differences had individual group sizes of n = 10 (Monti et al. 2013) and n = 15 (Tremblay et al. 2013) examining group differences. There also do not appear to be any meaningful effect sizes when examining the means and standard deviations of our volumetric data. This suggests that the current results are likely not an artifact of low power to detect differences.
Lack of volumetric differences as suggested by these data does not mean this sample is free of neural-related differences. In a subsample (n = 36) of these participants, we previously showed that the mTBI group exhibited less blood-oxygen-level dependent (BOLD) signal in left hemisphere brain regions associated with memory encoding and recognition during a verbal-paired associates task despite comparable task performance and memory scores on traditional neuropsychological tasks (Terry et al. 2015). Additionally, preliminary analyses of diffusion tensor imaging data on this sample indicate reduced fractional anisotropy in the mTBI group in the right genu/body of the corpus callosum, bilateral internal capsule, bilateral superior longitudinal fasciculus, and bilateral infero-frontal longitudinal fasciculus (Terry and Miller 2016). Other groups examining the long-term effects of sports-related concussions have also showed differences in white matter (Hart et al. 2013; Tremblay et al. 2014) as well as electrophysiology, potentially in the fronto-parietal networks (Broglio et al. 2012; De Beaumont et al. 2009; for review, see Henry et al. 2016). Taken together, there may be some neuroanatomical abnormalities in these participants, but they have not yet reached the level of gross brain atrophy or functional impairments in everyday life.
Exploratory post-hoc analyses did not show a relationship between hippocampal volume and memory functioning as would have been expected in this community-based sample. However, they did show a positive relationship between overall cognitive functioning and gray matter volume as other studies have also shown between brain metrics and cognition (Tate et al. 2014; Tremblay et al. 2013). This relationship did not differ between the concussed and control groups.
There are several limitations to this study. The heterogeneity of types of mTBI (e.g. severity, location of impact, loss of consciousness, acute symptom presentation, duration of symptoms, etc.) limits the specificity of our results. Differences in injury characteristics likely influence the specific pathophysiological processes associated with the injury and may also influence long-term anatomic changes. Further, the retrospective nature of reporting about these concussive events and the lack of medical records associated with the injury limits our ability to ensure a truly accurate diagnosis of a concussion, its severity, and statistically model other factors contributing to injury heterogeneity. However, given the under-diagnosis of mTBIs due to historical views about mTBI, desire to continue to play, and other factors, we found that including subjects without professional medical attention would increase the external validity of the sample. The sample size common in imaging studies of this nature limits the ability to model the known injury characteristics (e.g., loss of consciousness). We did not compare anatomical volumes by hemispheres because we lacked specific lateralized hypotheses and wanted to limit the number of statistical comparisons. Another limitation is the cross-sectional nature of this study, which would limit our ability to conclude that group differences are the product of the mTBI events. In the wake of null findings, there is always the potential that other variables that were not accounted for modified or masked the volumetric differences between groups. Lastly, the current null findings may be an artifact of the time since the injury. It is possible that functional MRI and white matter differences may predict later volumetric differences and cognitive decline in the future as is seen in neurodegenerative disorders (Canu et al. 2010; Wierenga and Bondi 2007).
It is also worth commenting on the effect size analysis on the demographic data between the two groups. These analyses showed small-to-medium effect sizes, such that the concussed group was older and reported more concussive-like symptoms compared to the control group. We do not believe that these potential group differences influenced the analysis or interpretation of our data, given that both increased age and concussion-related pathology would likely lead to smaller volumes (Du et al. 2006; Ross et al. 2014; Terribilli et al. 2011). Including age as a covariate did not influence our findings. We did not deem it necessary to examine other covariates.
This study adds to the overall body of literature related to potential neuroanatomic changes post-mTBI. This is one of few studies to examine potential brain volume differences in former high school football players with multiple concussions. Data suggests there are no statistically significant differences in intracranial volume, white matter volume, gray matter volume, and lateral ventricle volume. Further, there was a lack of group differences in more specific regions previously associated with mTBI (i.e. hippocampus, ACC). Future research is needed to assess whether volumetric differences manifest in these individuals later in life given the function imaging and diffusion tensor imaging findings.
References
American Congress of Rehabilitation Medicine. (1993). Definition of mild traumatic brain injury. Journal of Head Trauma Rehabilitation, 8, 86–87.
Arciniegas, D., Olincy, A., Topkoff, J., McRae, K., Cawthra, E., Filley, C., et al. (2000). Impaired auditory gating and P50 Nonsuppression following traumatic brain injury. The Journal of Neuropsychiatry and Clinical Neurosciences, 12, 77–85.
Bazarian, J. J., Zhong, J., Blyth, B., Zhu, T., Kavcic, V., & Peterson, D. (2007). DTI detects clinically important axonal damage after mild TBI: A pilot study. Journal of Neurotrauma, 24, 1447–1459. doi:10.1089/neu.2007.0241.
Bigler, E. D. (2004). Neuropsychological results and neuropathological findings at autopsy in a case of mild traumatic brain injury. Journal of the International Neuropsychological Society, 10, 794–800. doi:10.1017/S1355617704105146.
Blennow, K., Hardy, J., Zetterberg, H. (2012). The neuropathology and neurobiology of traumatic brain injury. Neuron, 6,(76), 886–899.
Blumbergs, P. C., Scott, G., Manavis, J., Wainwright, H., Simpson, D. A., & McLean, A. J. (1994). Staining of amyloid precursor protein to study axonal damage in mild head injury. Lancet, 344, 1055–1056. doi:10.1016/S0140-6736(94)91712-4.
Broglio, S. P., Macciocchi, S. N., & Ferrara, M. S. (2007). Neurocognitive performance of concussed athletes when symptom free. Journal of Athletic Training, 42, 504–508.
Broglio, S. P., Eckner, J. T., Paulson, H. L., & Kutcher, J. S. (2012). Cognitive decline and aging: The role of concussive and subconcussive impacts. Exercise and Sport Sciences Reviews, 40, 138–144. doi:10.1097/JES.0b013e3182524273.
Buckner, R. L., Head, D., Parker, J., Fotenos, A. F., Marcus, D., Morris, J. C., & Synder, A. Z. (2004). A unified approach for morphometric and functional data analysis in young, old, and demented adults using automated atlas-based head size normalization: Reliability and validation against manual of total intracranial volume. NeuroImage, 23, 724–738. doi:10.1016/j.neuroimage.2004.06.018.
Canu, E., McLaren, D. G., Fitzgerald, M. E., Bendlin, B. B., Zoccatelli, G., Alessandrini, F., et al. (2010). Microstructural diffusion changes are independent of macrostructural volume loss in moderate to severe Alzheimer’s disease. Journal of Alzheimer’s Disease, 19, 963–976. doi:10.3233/JAD-2010-1295.
Cassidy, J. D., Carroll, L. J., Peloso, P. M., Borg, J., von Holst, H., Holm, L., Kraus, J., Coronado, VG.; WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. (2004). Incidence, risk factors and prevention of mild traumatic brain injury: results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. Journal of Rehabilitation Medicine, 43(suppl), 28–60.
CDC (2010). Injury, prevention, & control: Traumatic brain injury. Center for Disease Control and Prevention. Retrieved from http://www.cdc.gov/traumaticbraininjury/statistics.html.
De Beaumont, L., Théoret, H., Mongeon, D., Messier, J., Leclerc, S., Tremblay, S., et al. (2009). Brain function decline in healthy retired athletes who sustained their last sports concussion in early adulthood. Brain, 132, 695–708. doi:10.1093/brain/awn347.
Du, A.-T., Schuff, N., Chao, L. L., Kornak, J., Jagust, W. J., Kramer, J. H., et al. (2006). Age effects on atrophy rates of entorhinal cortex and hippocampus. Neurobiology of Aging, 27, 733–740. doi:10.1016/j.neurobiolaging.2005.03.021.
Erickson, K. I., Prakash, R. S., Voss, M. W., Chaddock, L., Hu, L., Morris, K. S., et al. (2009). Aerobic fitness is associated with hippocampal volume in elderly humans. Hippocampus, 19, 1030–1039. doi:10.1002/hipo.20547.
Faul, M. D., Xu, L., Wald, M. M., & Coronado, V. G., (2010). Traumatic brain injury in the United States: Emergency department visits, hospitalizations, and deaths 2002–2006. Atlanta: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, pp. 2–70.
Fischl, B., Salat, D., Busa, E., Albert, M., Dieterich, M., Haselgrove, C., et al. (2002). Whole brain segmentation: Automated labeling of neuroanatomical structures in the human brain. Neuron, 33(3), 341–355. doi:10.1016/S0896-6273(02)00569-X.
Fischl, B., van der Kouwe, A., Destrieux, C., Halgren, E., Ségonne, F., Salat, D. H., et al. (2004a). Automatically parcellating the human cerebral cortex. Cerebral Cortex, 14(1), 11–22. doi:10.1093/cercor/bhg087.
Fischl, B., Salat, D. H., van der Kouwe, A. J., Makris, N., Ségonne, F., Quinn, B. T., & Dale, A. (2004b). Sequence-independent segmentation of magnetic resonance images. NeuroImage, 23, S69–S84. doi:10.1016/j.neuroimage.2004.07.016.
Gale, S. D., Johnson, S. C., Bigler, E. D., & Blatter, D. D. (1995). Trauma-induced degenerative changes in brain injury: A morphometric analysis of three patients with preinjury and postinjury MR scans. Journal of Neurotrauma, 12(2), 151–158. doi:10.1089/neu.1995.12.151.
Gioia, G. A., & Collins, M. W. (2006) Acute concussion evaluation (ace): physician/clinician version. Available at: http://ww.cdc.gov/ncipc/tbi/PhysiciansToolKit.htm.
Gioia, G. A., Collins, M. W., & Isquith, P. K. (2008). Improving identification and diagnosis of mild traumatic brain injury with evidence: Psychometric support for the acute concussion evaluation. The Journal of Head Trauma Rehabilitation, 23, 230–242. doi:10.1097/01.HTR.0000327255.38881.ca.
Hall, R. C., Hall, R. C., & Chapman, M. J. (2005). Definition, diagnosis, and forensic implications of postconcussional syndrome. Psychosomatics, 46(3), 195–202. doi:10.1176/appi.psy.46.3.195.
Hart Jr., J., Kraut, M. A., Womack, K. B., Strain, J., Didehbani, N., Bartz, E., et al. (2013). Neuroimaging of cognitive dysfunction and depression in aging retired National Football League players: A cross-sectional study. JAMA Neurology, 70, 326–335. doi:10.1001/2013.jamaneurol.340.
Head, D., Rodrigue, K. M., Kennedy, K. M., & Raz, N. (2008). Neuroanatomical and cognitive mediators of age-related differences in episodic memory. Neuropsychology, 22(4), 491–507. doi:10.1037/0894-4105.22.4.491.
Henry, L. C., Tremblay, S., & De Beaumont, L. (2016). Long-term effects of sports Concussions: Bridging the Neurocognitive Repercussions of the Injury with the Newest Neuroimaging Data. Neuroscientist. doi:10.1177/1073858416651034
Hofman, P. A., Stapert, S. Z., van Kroonenburgh, M. J., Jolles, J., de Kruijk, J., & Wilmink, J. T. (2001). MR imaging, single-photon emission CT, and neurocognitive performance after mild traumatic brain injury. American. Journal of Neuroradiology, 22(3), 441–449.
Hughes, D. G., Jackson, A., Mason, D. L., Berry, E., Hollis, S., & Yates, D. W. (2004). Abnormalities on magnetic resonance imaging seen acutely following mild traumatic brain injury: Correlation with neuropsychological tests and delayed recovery. Neuroradiology, 46(7), 550–558. doi:10.1007/s00234-004-1227-x.
Iverson, G. L., Lovell, M. R., Smith, S., & Franzen, M. D. (2000). Prevalence of abnormal CT- scans following mild head injury. Brain Injury, 14(12), 1057–1061. doi:10.1080/02699050050203559.
Jarrett, M., Tam, R., Hernández-Torres, E., Martin, N., Perera, W., Zhao, Y., et al. (2016). A prospective pilot investigation of brain volume, white matter Hyperintensities, and hemorrhagic lesions after mild traumatic brain injury. Frontiers in Neurology, 7, 11. doi:10.3389/fneur.2016.00011.
Johnston, K. M., Ptito, A., et al. (2001). New frontiers in diagnostic imaging in concussive head injury. Clinical Journal of Sport Medicine, 11(3), 166–175. doi:10.1097/00042752-200107000-00007.
Kendler, K. S., Jacobson, K., Myers, J. M., & Eaves, L. J. (2008). A genetically informative developmental study of the relationship between conduct disorder and peer deviance in males. Psychological Medicine, 38, 1001–1011. doi:10.1017/S0033291707001821.
Kramer, J. H., Mungas, D., Reed, B. R., Wetzel, M. E., Burnett, M. M., Miller, B. L., et al. (2007). Longitudinal MRI and cognitive change in healthy elderly. Neuropsychology, 21(4), 412–418. doi:10.1037/0894-4105.21.4.412.
Ling, J. M., Kilmaj, S., Toulouse, T., & Mayer, A. R. (2013). A prospective study of gray matter abnormalities in mild traumatic brain injury. Neurology, 81, 2121–2127. doi:10.1212/01.wnl.0000437302.36064.b1.
List, J., Ott, S., Bukowski, M., Lindenberg, R., & Flöel, A. (2015). Cognitive function and brain structure after recurrent mild traumatic brain injuries in young-to-middle-aged adults. Frontiers in Human Neuroscience, 9, 228. doi:10.3389/fnhum.2015.00228.
MacKenzie, J. D., Siddiqi, F., Babb, J. S., Bagley, L. J., Mannon, L. J., Sinson, G. P., & Grossman, R. I. (2002). Brain atrophy in mild or moderate traumatic brain injury: A longitudinal quantitative analysis. American Journal of Neuroradiology, 23(9), 1509–1515.
McCrory, P., Meeuwisse, W., Johnston, K., Dvorak, J., Aubry, M., Molloy, M., & Cantu, R. (2009). Consensus statement on concussion in sport - the 3rd international conference on concussion in sport held in Zurich. PM R, 1, 406–420. doi:10.1016/j.pmrj.2009.03.010.
Moffitt, T. E., Harrington, H., Caspi, A., Kim-Cohen, J., Goldberg, D., Gregory, A. M., & Poulton, R. (2007). Depression and generalized anxiety disorder: Cumulative and sequential comorbidity in a birth cohort followed prospectively to age 32 years. Archives of General Psychiatry, 64, 651–660. doi:10.1001/archpsyc.64.6.651.
Monti, J. M., Voss, M. W., Pence, A., McAuley, E., Kramer, A. F., & Cohen, N. J. (2013). History of mild traumatic brain injury is associated with deficits in relational memory, reduced hippocampal volume, and less neural activity later in life. Frontiers in Aging Neuroscience, 5, 41. doi:10.3389/fnagi.2013.00041.
Morey, R. A., Petty, C. M., Xu, Y., Hayes, J. P., Wagner, H. R., Lewis, D. V., et al. (2009). A comparison of automated seg- mentation and manual tracing for quantifying hippocampal and amygdala volumes. NeuroImage, 45, 855–866. doi:10.1016/j.neuroimage.2008.12.033.
Niogi, S. N., & Mukherjee, P. (2010). Diffusion tensor imaging of mild TBI. The Journal of Head Trauma Rehabilitation, 25(4), 241–255. doi:10.1097/HTR.0b013e3181e52c2a.
Piland, S. G., Ferrara, M. S., Macciocchi, S. N., Broglio, S. P., & Gould, T. E. (2010). Investigation of baseline self-report concussion symptom scores. Journal of Athletic Training, 45(3), 273–278. doi:10.4085/1062-6050-45.3.273.
Randolph, C., Tierney, M., Mohr, E., & Chase, T. (1998). The Repeatable Battery for the assessment of neuropsychological status (RBANS): Preliminary clinical validity. Journal of Clinical and Experimental Neuropsychology, 20, 310–319. doi:10.1076/jcen.20.3.310.823.
Ross, D. E., Ochs, A. L., Seabaugh, J. M., DeMark, M. F., Shrader, C. R., Marwitz, J. H., & Havranek, M. D. (2012). Progressive brain atrophy in patients with chronic neuropsychiatric symptoms after mild traumatic brain injury: A preliminary study. Brain Injury, 26, 1500–1509. doi:10.3109/02699052.2012.694570.
Ross, D. E., Ochs, A. L., DeSmit, M. E., & Seabaugh, J. M. (2014). Back to the future estimating pre-injury brain volume in patients with traumatic brain injury. NeuroImage. doi:10.1016/j.neuroimage.2014.07.043.
Sanfilipo, M. P., Benedict, R. H., Zivadinov, R., & Bakshi, R. (2004). Correction for intracranial volume in analysis of whole brain atrophy in multiple sclerosis: The proportion vs. residual method. NeuroImage, 22, 1732–1743.
Singh, R., Meier, T. B., Kuplicki, R., Savitz, J., Mukai, I., Cavanagh, L., Allen, T., Teague, T. K., et al. (2014). Relationship of collegiate football experience and concussion with hippocampal volume and cognitive outcomes. JAMA, 311, 1883–1888. doi:10.1001/jama.2014.3313.
Stein, M. B., & McAllister, T. W. (2009). Exploring the convergence of posttraumatic stress disorder and mild TBI. The American Journal of Psychiatry, 166(7), 768–776. doi:10.1176/appi.ajp.2009.08101604.
Tate, D. F., York, G. E., Reid, M. W., Cooper, D. B., Jones, L., Robin, D. A., Kennedy, J. E., & Lewis, J. (2014). Preliminary findings of cortical thickness abnormalities in blast injured service members and their relationship to clinical findings. Brain, Imaging, and Behavior, 8, 102–109. doi:10.1007/s11682-013-9257-9.
Terribilli, D., Schaufelberger, M. S., Duran, F. L. S., Zanetti, M. V., Curiati, P. K., Menezes, P. R., et al. (2011). Age-related gray matter volume changes in the brain during non-elderly adulthood. Neurobiology of Aging, 32(2–6), 354–368. doi:10.1016/j.neurobiolaging.2009.02.008.
Terry, D. P., & Miller, L. S. (2016). Microstructural white matter differences in former high school football players with a history of multiple concussions. In Paper presented at the National Academy of Neuropsychology annual conference, October 2016. Seattle, WA.
Terry, D. P., Adams, T. E., Ferrara, M. S., & Miller, L. S. (2015). FMRI hypoactivation during verbal learning and memory in former high school football players with multiple concussions. Archives of Clinical Neuropsychology, 30, 341–355. doi:10.1093/arclin/acv020.
Tremblay, S., De Beaumont, L., Henry, L. C., Boulanger, Y., Evans, A. C., Bourgouin, P., et al. (2013). Sports concussions and aging: A neuroimaging investigation. Cerebral Cortex, 23, 1159–1166. doi:10.1093/cercor/bhs102.
Tremblay, S., Henry, L. C., Bedetti, C., Larson-Dupuis, C., Gagnon, J. F., Evans, A. C., et al. (2014). Diffuse white matter tract abnormalities in clinically normal ageing retired athletes with a history of sports-related concussions. Brain, 137, 2997–3011. doi:10.1093/brain/awu236.
Wierenga, C. E., & Bondi, M. W. (2007). Use of functional magnetic resonance imaging in the early identification of Alzheimer’s disease. Neuropsychology Review, 17(2), 127–143. doi:10.1007/s11065-007-9025-y.
Wilde, E. A., Bigler, E. D., Huff, T., Wang, H., Black, G. M., Christensen, Z. P., et al. (2016). Quantitative structural neuroimaging of mild traumatic brain injury in the chronic effects of Neurotrauma consortium (CENC): Comparison of volumetric data within and across scanners. Brain Injury, 30, 1442–1451. doi:10.1080/02699052.2016.1219063.
Zhou, Y., Kierans, A., Kenul, D., Ge, Y., Rath, J., Reaume, J., Grossman, R. I., & Lui, Y. W. (2013). Mild traumatic brain injury: Longitudinal regional brain volume changes. Radiology, 267, 880–890. doi:10.1148/radiol.13122542.
Acknowledgements
This research was made possible by the charitable contributions of the John & Mary Franklin Foundation and the BioImaging Research Center at the University of Georgia. There are no other funding agencies or conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by partial support to D.P. Terry by the John and Mary Franklin Foundation and the University of Georgia BioImaging Research Center.
Conflict of interest
D.P. Terry and L.S. Miller declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the University of Georgia Institutional Review Board and with the 1964 Helsinki declaration and its later amendments.
Additional information
Submitted as an Original Report to the Brain Imaging and Behavior
Rights and permissions
About this article
Cite this article
Terry, D.P., Miller, L.S. Repeated mild traumatic brain injuries is not associated with volumetric differences in former high school football players. Brain Imaging and Behavior 12, 631–639 (2018). https://doi.org/10.1007/s11682-017-9719-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11682-017-9719-6