Abstract
Apathy is a common but poorly understood neuropsychiatric disturbance in Parkinson’s disease (PD). In a recent study using event-related brain potentials we demonstrated impaired reward processing and compromised mesocortico-limbic pathways in PD patients with clinical symptoms of apathy. Here we aimed to further investigate the involvement of reward circuits in apathetic PD patients by assessing potential differences in brain structure. Using structural magnetic resonance imaging (MRI) and voxel-based morphometry (VBM) we quantified grey matter volume (GMV) in a sample of 18 non-demented and non-depressed PD patients with apathy, and 18 matched non-apathetic patients. Both groups were equivalent in terms of sociodemographic characteristics, disease stage, cognitive performance and L-Dopa equivalent daily dose. Apathetic patients showed significant GMV loss in cortical and subcortical brain structures. Various clusters of cortical GMV decrease were found in the parietal, lateral prefrontal cortex, and orbitofrontal cortex (OFC). The second largest cluster of GMV loss was located in the left nucleus accumbens (NAcc), a subcortical structure that is a key node of the human reward circuit. Isolated apathy in our sample is explained by the combined GMV loss in regions involved in executive functions, and cortical and subcortical structures of the mesolimbic reward pathway. The correlations observed between apathy and cognition suggests apathy as a marker of more widespread brain degeneration even in a sample of non-demented PD patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Among the whole spectrum of behavioral disturbances found in Parkinson’s disease (PD), apathy represents one of the most commonly reported (Pedersen et al. 2010; Aarsland et al. 2009). Apathy is defined as a state of diminished goal-directed behavior, reduced interest for pleasurable activities and flattened affect. These disturbances cannot be attributed to a decreased level of consciousness, cognitive impairment or depression (Marin 1991; Levy and Dubois 2006; Pagonabarraga et al. 2015). The prevalence of apathy in PD ranges from 17 % to 70 %, having a profound impact on the patient’s quality of life and increasing the burden of caregivers. Moreover, apathy severity has been associated with executive dysfunction and with an increased risk for the development of dementia. However, the executive deficits associated with apathy do not fully explain the clinical correlates and underlying mechanisms of apathy in PD.
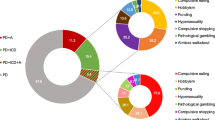
Better understanding on the different brain circuits that cause apathy in PD would help to provide more adequate treatment strategies for its management (Dujardin et al. 2007). Signs and symptoms of apathy recorded from clinical observation have been structured into four subdomains involving: a) executive dysfunction (decrease in cognitive interests); b) deficits in auto-activation (lack of self-initiated mental processes); c) emotional distress (negative affect); and d) deficits in reward processing (decreases response to positive reinforces).
These four subdomains have been associated with different neural substrates. Executive dysfunction is thought to involve the dorsolateral prefrontal cortex (DLPFC), the dorsal caudate and putamen and the anterior cingulate cortex (ACC). Alterations in this circuit would lead to decreased planning and cognitive inertia (Levy and Dubois 2006). Impaired auto-activation has been associated with deficits in the ventral tegmental area, territories in the dorsomedial prefrontral cortex (PFC) including the supplementary motor area and the ACC. Alterations at this level would lead to a decrease in self-initiated behavior. The emotional distress subdomain has been related with hyperactivity in the subgenual cingulate cortex, and hypometabolism of the PFC and dorsal ACC. These alterations have been related to negative emotions of depression such as sadness and hopelessness. Finally, deficits in reward processing would involve the mesocortico-limbic pathway that includes the ventral tegmental area, orbitofrontal cortex, and nucleus accumbens (NAcc). The NAcc is a key node of the reward circuit, with robust activation responses to positive reinforcers (Riba et al. 2008).
The dysexecutive basis for apathy in PD has been clearly explained by the massive disruption of the dorsal caudate reciprocal thalamo-cortical projections to DLPFC. However, it has been also shown that alterations in the mesocortico-limbic pathway play an important role in the development of apathy (Martinez-Horta et al. 2014). Decreased responsiveness at this level would underlie emotional flatness, decreased emotional resonance, and decreased response to positive and negative reinforcers, as can be clinically observed in apathetic PD patients.
In line with reward processing deficits, in a recent study using event-related brain potentials we demonstrated reduced sensitivity to monetary incentives in early-stage PD patients with apathy (Martinez-Horta et al. 2014). The study compared cognitively-preserved and non-depressed PD patients with clinical symptoms of apathy with matched non-apathetic PD patients. The study showed significant decreases in the amplitude of the feedback-related negativity or FRN, a neurophysiological correlate of incentive processing. These results strongly supported a compromised mesocortico-limbic pathway as a key process in the pathogenesis of apathy in PD.
In the present study, we aimed to investigate the presence of structural brain abnormalities in PD patients who have developed clinically relevant symptoms of apathy. Using magnetic resonance imaging (MRI) and voxel-based morphometry (VBM) we compared brain structure between two groups of matched PD patients with isolated apathy. According to standard criteria, all participants were classified as non-demented and non-depressed and only differed with regard to the presence or absence of apathy.
Methods
Patient recruitment
Thirty-six PD patients with isolated apathy were prospectively included in the study. The sample was recruited from outpatients regularly visiting the Movement Disorders Unit at Sant Pau Hospital The diagnosis of PD was established according to the Queens Square Brain Bank criteria (Daniel and Lees 1993).
The diagnosis of apathy was established by using a semi-structured clinical interview based on the standard diagnostic criteria for apathy (P. Robert et al. 2009). An initial screening for the presence of clinically relevant symptoms of apathy was conducted using item 4 of the UPDRS part I (Goetz et al. 2008). The item is scored on a five-point scale ranging from 0 to 4, with higher scores indicating more severe symptoms of apathy. A score of 2/3 was chosen as an adequate value to initially identify potential study participants, avoiding the inclusion of patients with extreme symptomatology associated with the minimal score of 1 or the maximum score of 4. The score of 2/3 has adequate sensitivity and specificity (Leentjens et al. 2008) and a recent study confirmed it value for detecting apathy in PD (Weintraut et al. 2016). The semi-structured interview was given to screened patients, and only those fulfilling the diagnostic criteria for apathy were included in the study (sees supplementary material).
Exclusion criteria were patients presenting clinically meaningful depression and/or anxiety, as assessed by a score ≥ 11 on the depression and/or anxiety items of the Hospital Anxiety and Depression Scale (HADS) (Mumford 1991). More comprehensive assessment for depressive symptoms was done through the administration of a semi-structured clinical interview based on the standard DSM-IV-R diagnostic criteria for depression and dystimia. Presence of motor fluctuations in response to L-dopa, or medium-to-advanced PD according to Hoehn and Yahr stages (H&Y > 2) (Hoehn and Yahr 1967) also constituted exclusion criteria. Patients with dementia were also excluded, as assessed by a score < 24 on the Mini-Mental State Examination (MMSE) (Folstein et al. 1975), and a score < 123 on the Dementia Rating Scale (DRS) (Llebaria et al. 2008), which constitutes a level 1 recommended instrument from the Movement Disorders Society Task Force for the screening of dementia in PD (PDD) (Litvan et al. 2011; Dubois et al. 2007; Emre et al. 2007). Patients with focal abnormalities in neuroimaging studies, alterations in blood tests, non-compensated systemic disease (i.e., diabetes, hypertension) and patients taking psychopharmacological medications were also excluded.
Each patient, with his or her caregiver if appropriate, was interviewed regarding disease onset and medication history, including type of motor response to L-dopa. All study participants were taking L-dopa and dopaminergic agonists (DA). Current medications and dosages were calculated for L-dopa daily dose, DA equivalent L-dopa daily dose and total L-dopa daily dose (LED) (Tomlinson et al. 2010). Participants were required to have received stable doses of dopaminergic drugs for the last 12 weeks and to show a stable response to medications. Motor status and disease stage were assessed by experienced neurologists in movement disorders (JP & JK) using the Unified Parkinson’s Disease Rating Scale (UPDRS).
Potential differences between groups in demographic, clinical, cognitive and behavioral characteristics were analyzed with independent two-tailed t-tests for continuous variables, Mann-Whitney test for ordinal data, and the χ2 test for categorical variables. Associations between the demographic, clinical and cognitive variables were analyzed with Pearson’s correlations. Significance was set at p < 0.05.
MRI acquisition
T1-weighted images were acquired on a Phillips 3 T Achieva in sagittal orientation (TR = 7.4 and TE = 3.4, matrix size =228 mm × 218 mm; flip angle =9°, FOV = 250x250x180, slice thickness = 1.1 mm, 300 slices, acquisition time = 4′55″, voxel size =0.98 × 0.98 × 0.6).
MRI data processing and statistics
Gray matter volume (GMV) analysis from T1-weighted images was carried out using voxel-based morphometry (VBM) analysis in SPM8. The preprocessing steps were as follows.
First, unified segmentation was applied to the structural T1-weighted images of each subject. During this segmentation step, affine regularization was performed applying the values for the ICBM space template for European brains. The resulting tissue probability maps (GM maps) were then normalized to a standard stereotactic space using the corresponding DARTEL transformations to achieve spatial normalization into Montreal Neurological Institute (MNI) space. All normalized GM images were further analyzed to identify regional differences in GMV (using “modulation” to compensate for the effect of spatial normalization). Finally, the normalized and modulated images were smoothed using an isotropic spatial filter (FHWN =8 mm) to reduce residual inter-individual variability.
The individual smoothed GMV images were entered into a voxel-wise second-level two-sample t-test between the apathetic and non-apathetic PD patient groups. Individual values of total intracranial volume (TIV) were extracted and included as a nuisance variable to correct for global differences in TIV and, since no one of the recorded clinical variables exhibited significant differences between groups, age and sex were included as covariates of no interest. Results showing p < 0.005 (uncorrected) (Lieberman and Cunningham 2009) and a minimum extent of 50 voxels were considered significant. For the clusters showing significant gray matter differences, a small-volume correction (SVC) was applied (Worsley et al. 1996). Specifically, results were small volume corrected for family-wise error (FWE p < 0.05) within a sphere of 15 mm of diameter around peak coordinates extracted from independent studies (van der Vegt et al. 2013; Reijnders et al. 2010).
GMV at the regions of interest (ROIs) extracted from the clusters obtained in the former voxel-wise analysis were computed from build-in SPM8 functions to perform further regression analysis with other clinical variables of interest.
Results
Socio-demographic and clinical matching
As shown in Table 1, groups were carefully matched for all clinical and socio-demographic variables. Only the presence of symptoms of apathy differentiated the two groups. Data in the table are expressed as means ± standard deviation (SD) for the continuous variables, as percentage for the categorical variables and as mean range for the ordinal variables.
As indicated in the table, the sample was clinically characterized by individuals in the early to middle stages of the disease (disease duration 7.5 ± 5.1 years; H&Y stage 1.8 ± 0.4). In both groups, total MMSE and DRS scores ranged above the proposed cut-off score for dementia. To address the presence of subtle signs of cognitive impairment, we applied the accepted MDS criteria for mild cognitive impairment associated to PD (PD-MCI). (Litvan et al. 2011) Thus, using the suggested cut-off score of total DRS score < 138, up to 64 % of patients accomplished criteria for PD-MCI. Based on these criteria, prevalence of PD-MCI was up to 77 % in the apathy group and 50 % in the non-apathy group. These percentages resulted in a non-significant trend of increased prevalence of PD-MCI on the apathy group (χ2 = 3.1; p = 0.083). This result is consistent with previous findings supporting more impaired cognitive performance in apathetic PD patients (Pluck and Brown 2002; Martinez-Horta et al. 2013; Santangelo et al. 2015).
Focusing on specific subdomains of the DRS, a slight significant decrease was found for conceptualization in the apathy group (p = .04), but no significant differences were found on memory, attention, initiation/perseveration or construction.
No relevant signs of anxiety or depression were evidenced on the HADS scores and subsequent clinical interviews.
Voxel-based morphometry and statistical results
As seen in Fig. 1, between group comparisons of the VBM analysis showed a significant reduction of GMV in a set of cortical and subcortical brain regions in the apathetic patient group.
Cortical GMV decreases were found in the left inferior parietal lobule (BA 40, SVC p = 0.002 FWE), left superior parietal gyrus (BA 7), left orbitofrontal cortex (BA 47), right postcentral gyrus (BA 3), right inferior frontal gyrus (BA 44, SVC p = 0.033 FWE) and right supplementary motor area (Table 2).
The only subcortical structure that showed statistically significant differences between groups was the left nucleus accumbens (NAcc, SVC p = 0.041 FWE), in the ventral part of the striatum (Fig. 2). Using less stringent criteria (p < 0.01, uncorrected) GMV decreases were found bilaterally (see supplementary data).
GMV at the identified ROIs showed a significant correlation with clinical variables. Decreased GMV in the NAcc significantly correlated with global cognitive performance as measured by the DRS total score (r = .831; p < .001). Focusing on the different DRS sub-scores, this relation appeared exclusively associated with performance on the memory domain (r = .388; p = .01). At the emotional level, a negative correlation between the left inferior orbital prefrontal cortex and depression HADS scores (r = −.523; p = .003) was found. At the cognitive level, significant correlations were found between GMV reduction in the right inferior frontal gyrus with lower DRS total score (r = .513; p = 0.001), and lower conceptualization (r = .371; p = .02), memory (r = .417; p = .01) and initiation/perseveration (r = .331; p = .04) item scores. Decreased GMV in the left superior parietal gyrus correlated also with lower score in the initiation/perseveration item of the DRS (r = .436; p = .008).
Discussion
In the present study, we searched for structural brain abnormalities in PD patients with clinical manifestations of isolated apathy. Based on previous data indicating deficits in reward processing in this population, we postulated that structural compromise will extend from territories linked to executive functions to structures within the mesocortico-limbic reward circuit. In keeping with this hypothesis, apathetic patients showed significant areas of GMV loss in subcortical and cortical brain regions. Significant clusters of GMV loss were located in the left NAcc and left inferior orbital PFC, both key nodes of the human reward circuit (Riba et al. 2008). Analysis on cortical findings showed spatially distributed clusters of grey matter decrease over the parietal and frontal lobes, involving functionally related areas that participate on action preparation/initiation, manipulation of information, as well as high-order integration of emotional stimuli.
Based on these findings, apathy in PD is associated with combined atrophy of fronto-parietal areas involved in executive functions, and regions of the human reward circuit. Initial research considered apathy in PD as a specific manifestation of the executive function caused by dopaminergic depletion of lateral prefrontal areas (Pluck and Brown 2002; Levy and Dubois 2006; Santangelo et al. 2015; Levy and Czernecki 2006). Apathy in PD has been consistently associated with the progressive executive dysfunction caused by decreased activation of lateral prefrontal and posterior parietal areas (Isella et al. 2002). In accordance, apathy in PD has been merely explained as secondary to functional deficits associated with nigrostriatal and mesocortical dopamine depletion in the putamen and caudate nucleus, respectively. (Santangelo et al. 2015; Pluck and Brown 2002; Martinez-Horta et al. 2013). However, when apathy in PD has been explored with more extensive neuropsychological batteries, it has also been observed to be associated with impairment in tasks involving reward or emotional processing (Martinez-Horta et al. 2013; Martinez-Corral et al. 2010). In agreement with this hypothesis, in recent study using event-related brain potentials we demonstrated reduced sensitivity to monetary incentives in apathetic PD patients. The study measured the amplitude of the feedback-related negativity (FRN) while participants performed a lottery task. This wave, with generators in the ventral striatum and other limbic regions, was found to be significantly decreased in the apathetic subgroup (Martinez-Horta et al. 2014).
Our current anatomical findings give additional support to the notion of impaired reward processing in PD patients who develop apathy, and underline the existence of a more complex related circuitry which subserves motivational, cognitive and behavioral functions. The NAcc and the OFC are key structures within the mesolimbic reward pathway. In contrast with the nigrostriatal pathway, this circuit had been previously considered to remain relatively spared in early and middle PD stages (Rowe et al. 2008; Gotham et al. 1988, 1986). In contrast, the decreases in grey matter found here in both the NAcc and the OFC support its compromise in patients who develop apathy, even in the early stages of the disease. The left-sided lateralized pattern we found is consistent with the eminent unilateral-to-bilateral course of PD pathology. In fact, using less strict p-value (p < 0.01) a significant decrease can be bilaterally seen showing that right NAcc is not free of more severe degeneration in apathetic PD patients (see supplementary data).
These results are in line with recent neuroimaging studies using various assessment techniques. In one study using resting-state fMRI, Baggio and colleagues found an association between apathy and altered functional connectivity between the limbic regions of the PFC and the striatum (Baggio et al. 2015). However, this study did not properly control the effect of depression in the studied sample. In another study using shape analysis, the authors found atrophy of the NAcc in association with more severe apathetic symptoms in PD. However, part of the studied sample did not accomplish criteria for apathy, and this relationship was found only in relation to symptom severity (Carriere et al. 2014). Different PET studies have also given evidence on the decreased mesocortico-limbic dopaminergic activity present in apathetic PD patients. By using [11C]-Raclopride, [11C]-RTI-32 and [18]-FDG decreased dopamine release capacity has been observed in the mesolimbic circuit, as well as reduced binding and metabolism in the ventral striatum (Thobois et al. 2010; Remy et al. 2005; G. H. Robert et al. 2014). Our results extend and support the existence of structural abnormalities in the NAcc in non-demented PD patients from the early and middle stages of the disease.
In addition to the NAcc, we found GMV decreases in cortical brain areas. Atrophy in these regions may account for manifestations pertaining to other symptomatology domains than reward processing. Grey matter loss was found in the premotor cortex, including the SMA, and the pars opercularis of the inferior frontal gyrus (BA44). This cluster included regions around the insular cortex, the DLPFC and the pars triangularis (BA45). These last two areas connect with the middle (BA46) and the orbital (BA47) frontal areas. The alteration of the premotor cortex in our apathetic patients could be linked to the disruption of self-initiated behavior and thus to deficits in the auto-activation domain. These deficits would be further supported by cortical atrophy around the insula and related frontal structures. GMV decreases at this level would be consistent with difficulties in the executive integration of plans of action.
Cortical regions connected with the limbic system also showed loss of GMV. Within the medial prefrontal cortex, isolated apathy was associated with decreased GMV in the OFC. The OFC is part of the mesocortico-limbic reward circuit, playing a critical role in incentive processing and higher order integration of emotion (Timbie and Barbas 2015). Abnormalities in the OFC have been associated not only to apathy, but also to depression, anxiety, and social cognition (Jenkins et al. 2014; Drevets 2007; Milad and Rauch 2007; Levy and Dubois 2006). The correlation observed between volume loss in the OFC and depression HADS scores could be interpreted as a marker of the emotional distress that may coexist even in apathetic patients without clinical criteria for depression(Pagonabarraga et al. 2015). On the contrary, it could be also the consequence that many items in commonly used scales for depression (including the HADS), are actually measuring decreased motivated behaviors. Since patients in our sample were free of clinically relevant depression, OFC atrophy –in conjunction with decreased volume in the NAcc– may indicate that not only loss of GMV in lateral aspects of the prefrontal cortex lead to apathy, but that the concurrent disruption of cortical and subcortical regions within the mesocortico-limbic reward are crucial for the clinical manifestation of decreased goal-directed behaviors.
Additional clusters of grey matter reduction were found in the inferior frontal gyrus and in the parietal lobes. These two structures have been associated with the cognitive aspects of apathy in PD (Pagonabarraga et al. 2015). Atrophy of these regions may account for previous evidence indicating a pattern of worse cognitive performance in apathetic patients (Martinez-Horta et al. 2013; Pluck and Brown 2002). These deficits were seen mainly in tasks involving frontal executive capacities, but also in others that rely on adequate parietal function (Martinez-Horta et al. 2013). Importantly, impairment in these tasks has been associated with more accelerated cognitive decline (Williams-Gray et al. 2009; Aarsland et al. 2011). This raises the question of a possible link between more severe global cognitive dysfunction and apathy. In PD various authors have shown that apathy may herald dementia (Williams-Gray et al. 2009; P. Robert et al. 2009), and grey matter atrophy and cortical thinning in posterior cortical regions have been associated with an increased risk of developing dementia (Aarsland et al. 2011; Bohnen et al. 2007; Bohnen et al. 2006). In the present study, the correlations observed between the NAcc and several cortical regions with global cognitive deterioration involving not only executive functions, suggests that the presence of apathy is a marker of more extensive cortical and subcortical degeneration even in a sample of non-demented patients.
Taken together, the present neuroimaging findings indicate the presence of structural abnormalities in PD patients with apathy. These abnormalities were observed in subcortical and cortical brain regions in a carefully selective sample of non-demented PD patients with isolated apathy in the early to mid-stages of the disease. GMV decreases in the NAcc demonstrate atrophy of a core structure of the mesocortico-limbic circuit and support a compromise of the reward circuit in this population. Areas of GMV decrease in the parietal lobe, as well as in the lateral and medial aspects of the prefrontal cortex fit well with the cognitive, auto-activation and emotional symptoms also present in apathy. Finally, the significant relation between structural changes and specific cognitive aspects links apathy to cognitive deterioration.
Given the highly specific characteristics of the patient subpopulation studied here, the present findings should be generalized with caution. Apathetic PD patients are only a subgroup of the broad range of PD patients usually encountered in the clinical practice. Also, symptom manifestations may evolve differently in the various domains that constitute apathy in the course of PD. Thus, the degree of compromise of the neural circuits discussed here may vary in the different stages of the disease.
References
Aarsland, D., Bronnick, K., Alves, G., Tysnes, O. B., Pedersen, K. F., Ehrt, U., et al. (2009). The spectrum of neuropsychiatric symptoms in patients with early untreated Parkinson's disease. Journal of Neurology, Neurosurgery, and Psychiatry, 80(8), 928–930. doi:10.1136/jnnp.2008.166959.
Aarsland, D., Muniz, G., & Matthews, F. (2011). Nonlinear decline of mini-mental state examination in Parkinson's disease. Movement Disorders, 26(2), 334–337. doi:10.1002/mds.23416.
Baggio, H. C., Segura, B., Garrido-Millan, J. L., Marti, M. J., Compta, Y., Valldeoriola, F., et al. (2015). Resting-state frontostriatal functional connectivity in Parkinson's disease-related apathy. Movement Disorders, 30(5), 671–679. doi:10.1002/mds.26137.
Bohnen, N. I., Kaufer, D. I., Hendrickson, R., Ivanco, L. S., Lopresti, B. J., Constantine, G. M., et al. (2006). Cognitive correlates of cortical cholinergic denervation in Parkinson's disease and parkinsonian dementia. Journal of Neurology, 253(2), 242–247. doi:10.1007/s00415-005-0971-0.
Bohnen, N. I., Kaufer, D. I., Hendrickson, R., Constantine, G. M., Mathis, C. A., & Moore, R. Y. (2007). Cortical cholinergic denervation is associated with depressive symptoms in Parkinson's disease and parkinsonian dementia. Journal of Neurology, Neurosurgery, and Psychiatry, 78(6), 641–643. doi:10.1136/jnnp.2006.100073.
Carriere, N., Besson, P., Dujardin, K., Duhamel, A., Defebvre, L., Delmaire, C., et al. (2014). Apathy in Parkinson's disease is associated with nucleus accumbens atrophy: a magnetic resonance imaging shape analysis. Movement Disorders, 29(7), 897–903. doi:10.1002/mds.25904.
Daniel, S. E., & Lees, A. J. (1993). Parkinson's Disease Society Brain Bank, London: overview and research. Journal of Neural Transmission. Supplementum, 39, 165–172.
Drevets, W. C. (2007). Orbitofrontal cortex function and structure in depression. Annals of the New York Academy of Sciences, 1121, 499–527. doi:10.1196/annals.1401.029.
Dubois, B., Burn, D., Goetz, C., Aarsland, D., Brown, R. G., Broe, G. A., et al. (2007). Diagnostic procedures for Parkinson's disease dementia: recommendations from the movement disorder society task force. Movement Disorders, 22(16), 2314–2324. doi:10.1002/mds.21844.
Dujardin, K., Sockeel, P., Devos, D., Delliaux, M., Krystkowiak, P., Destee, A., et al. (2007). Characteristics of apathy in Parkinson's disease. Movement Disorders, 22(6), 778–784. doi:10.1002/mds.21316.
Emre, M., Aarsland, D., Brown, R., Burn, D. J., Duyckaerts, C., Mizuno, Y., et al. (2007). Clinical diagnostic criteria for dementia associated with Parkinson's disease. Movement Disorders, 22(12), 1689–1707 quiz 1837. doi:10.1002/mds.21507.
Folstein, M. F., Folstein, S. E., & McHugh, P. R. (1975). “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12(3), 189–198.
Goetz, C. G., Tilley, B. C., Shaftman, S. R., Stebbins, G. T., Fahn, S., Martinez-Martin, P., et al. (2008). Movement Disorder Society-sponsored revision of the unified Parkinson's disease rating scale (MDS-UPDRS): scale presentation and clinimetric testing results. Movement Disorders, 23(15), 2129–2170. doi:10.1002/mds.22340.
Gotham, A. M., Brown, R. G., & Marsden, C. D. (1986). Levodopa treatment may benefit or impair “frontal” function in Parkinson's disease. Lancet, 2(8513), 970–971.
Gotham, A. M., Brown, R. G., & Marsden, C. D. (1988). 'Frontal' cognitive function in patients with Parkinson's disease 'on' and 'off' levodopa. Brain, 111(Pt 2), 299–321.
Hoehn, M. M., & Yahr, M. D. (1967). Parkinsonism: onset, progression and mortality. Neurology, 17(5), 427–442.
Isella, V., Melzi, P., Grimaldi, M., Iurlaro, S., Piolti, R., Ferrarese, C., et al. (2002). Clinical, neuropsychological, and morphometric correlates of apathy in Parkinson's disease. Movement Disorders, 17(2), 366–371.
Jenkins, L. M., Andrewes, D. G., Nicholas, C. L., Drummond, K. J., Moffat, B. A., Phal, P., et al. (2014). Social cognition in patients following surgery to the prefrontal cortex. Psychiatry Research, 224(3), 192–203. doi:10.1016/j.pscychresns.2014.08.007.
Leentjens, A. F., Dujardin, K., Marsh, L., Martinez-Martin, P., Richard, I. H., Starkstein, S. E., et al. (2008). Apathy and anhedonia rating scales in Parkinson's disease: critique and recommendations. Movement Disorders, 23(14), 2004–2014. doi:10.1002/mds.22229.
Levy, R., & Czernecki, V. (2006). Apathy and the basal ganglia. Journal of Neurology, 253(Suppl 7), VII54–VII61. doi:10.1007/s00415-006-7012-5.
Levy, R., & Dubois, B. (2006). Apathy and the functional anatomy of the prefrontal cortex-basal ganglia circuits. Cerebral Cortex, 16(7), 916–928. doi:10.1093/cercor/bhj043.
Lieberman, M. D., & Cunningham, W. A. (2009). Type I and Type II error concerns in fMRI research: re-balancing the scale. Social Cognitive and Affective Neuroscience, 4(4), 423–428. doi:10.1093/scan/nsp052.
Litvan, I., Aarsland, D., Adler, C. H., Goldman, J. G., Kulisevsky, J., Mollenhauer, B., et al. (2011). MDS task force on mild cognitive impairment in Parkinson's disease: critical review of PD-MCI. Movement Disorders, 26(10), 1814–1824. doi:10.1002/mds.23823.
Llebaria, G., Pagonabarraga, J., Kulisevsky, J., Garcia-Sanchez, C., Pascual-Sedano, B., Gironell, A., et al. (2008). Cut-off score of the Mattis dementia rating scale for screening dementia in Parkinson's disease. Movement Disorders, 23(11), 1546–1550. doi:10.1002/mds.22173.
Marin, R. S. (1991). Apathy: a neuropsychiatric syndrome. The Journal of Neuropsychiatry and Clinical Neurosciences, 3(3), 243–254.
Martinez-Corral, M., Pagonabarraga, J., Llebaria, G., Pascual-Sedano, B., Garcia-Sanchez, C., Gironell, A., et al. (2010). Facial emotion recognition impairment in patients with Parkinson's disease and isolated apathy. Parkinsons Disease, 2010, 930627. doi:10.4061/2010/930627.
Martinez-Horta, S., Pagonabarraga, J., Fernandez de Bobadilla, R., Garcia-Sanchez, C., & Kulisevsky, J. (2013). Apathy in Parkinson's disease: more than just executive dysfunction. Journal of the International Neuropsychological Society, 19(5), 571–582. doi:10.1017/S1355617713000131.
Martinez-Horta, S., Riba, J., de Bobadilla, R. F., Pagonabarraga, J., Pascual-Sedano, B., Antonijoan, R. M., et al. (2014). Apathy in Parkinson's disease: neurophysiological evidence of impaired incentive processing. The Journal of Neuroscience, 34(17), 5918–5926. doi:10.1523/JNEUROSCI.0251-14.2014.
Milad, M. R., & Rauch, S. L. (2007). The role of the orbitofrontal cortex in anxiety disorders. Annals of the New York Academy of Sciences, 1121, 546–561. doi:10.1196/annals.1401.006.
Mumford, D. B. (1991). Hospital anxiety and depression scale. The British Journal of Psychiatry, 159, 729.
Pagonabarraga, J., Kulisevsky, J., Strafella, A. P., & Krack, P. (2015). Apathy in Parkinson's disease: clinical features, neural substrates, diagnosis, and treatment. Lancet Neurology, 14(5), 518–531. doi:10.1016/S1474-4422(15)00019-8.
Pedersen, K. F., Alves, G., Bronnick, K., Aarsland, D., Tysnes, O. B., & Larsen, J. P. (2010). Apathy in drug-naive patients with incident Parkinson's disease: the Norwegian ParkWest study. Journal of Neurology, 257(2), 217–223. doi:10.1007/s00415-009-5297-x.
Pluck, G. C., & Brown, R. G. (2002). Apathy in Parkinson's disease. Journal of Neurology, Neurosurgery, and Psychiatry, 73(6), 636–642.
Reijnders, J. S., Scholtissen, B., Weber, W. E., Aalten, P., Verhey, F. R., & Leentjens, A. F. (2010). Neuroanatomical correlates of apathy in Parkinson's disease: A magnetic resonance imaging study using voxel-based morphometry. Movement Disorders, 25(14), 2318–2325. doi:10.1002/mds.23268.
Remy, P., Doder, M., Lees, A., Turjanski, N., & Brooks, D. (2005). Depression in Parkinson's disease: loss of dopamine and noradrenaline innervation in the limbic system. Brain, 128(Pt 6), 1314–1322. doi:10.1093/brain/awh445.
Riba, J., Kramer, U. M., Heldmann, M., Richter, S., & Munte, T. F. (2008). Dopamine agonist increases risk taking but blunts reward-related brain activity. PloS One, 3(6), e2479. doi:10.1371/journal.pone.0002479.
Robert, P., Onyike, C. U., Leentjens, A. F., Dujardin, K., Aalten, P., Starkstein, S., et al. (2009). Proposed diagnostic criteria for apathy in Alzheimer's disease and other neuropsychiatric disorders. European Psychiatry, 24(2), 98–104. doi:10.1016/j.eurpsy.2008.09.001.
Robert, G. H., Le Jeune, F., Lozachmeur, C., Drapier, S., Dondaine, T., Peron, J., et al. (2014). Preoperative factors of apathy in subthalamic stimulated Parkinson disease: a PET study. Neurology, 83(18), 1620–1626. doi:10.1212/WNL.0000000000000941.
Rowe, J. B., Hughes, L., Ghosh, B. C., Eckstein, D., Williams-Gray, C. H., Fallon, S., et al. (2008). Parkinson's disease and dopaminergic therapy--differential effects on movement, reward and cognition. Brain, 131(Pt 8), 2094–2105. doi:10.1093/brain/awn112.
Santangelo, G., Vitale, C., Trojano, L., Picillo, M., Moccia, M., Pisano, G., et al. (2015). Relationship between apathy and cognitive dysfunctions in de novo untreated Parkinson's disease: a prospective longitudinal study. European Journal of Neurology, 22(2), 253–260. doi:10.1111/ene.12467.
Thobois, S., Ardouin, C., Lhommee, E., Klinger, H., Lagrange, C., Xie, J., et al. (2010). Non-motor dopamine withdrawal syndrome after surgery for Parkinson's disease: predictors and underlying mesolimbic denervation. Brain, 133(Pt 4), 1111–1127. doi:10.1093/brain/awq032.
Timbie, C., & Barbas, H. (2015). Pathways for Emotions: Specializations in the Amygdalar, Mediodorsal Thalamic, and Posterior Orbitofrontal Network. The Journal of Neuroscience, 35(34), 11976–11987. doi:10.1523/JNEUROSCI.2157-15.2015.
Tomlinson, C. L., Stowe, R., Patel, S., Rick, C., Gray, R., & Clarke, C. E. (2010). Systematic review of levodopa dose equivalency reporting in Parkinson's disease. Movement Disorders, 25(15), 2649–2653. doi:10.1002/mds.23429.
van der Vegt, J. P., Hulme, O. J., Zittel, S., Madsen, K. H., Weiss, M. M., Buhmann, C., et al. (2013). Attenuated neural response to gamble outcomes in drug-naive patients with Parkinson's disease. Brain, 136(Pt 4), 1192–1203. doi:10.1093/brain/awt027.
Weintraut, R., Karadi, K., Lucza, T., Kovacs, M., Makkos, A., Janszky, J., et al. (2016). Lille apathy rating scale and MDS-UPDRS for screening apathy in Parkinson's disease. Journal of Parasitic Diseases, 6(1), 257–265. doi:10.3233/JPD-150726.
Williams-Gray, C. H., Evans, J. R., Goris, A., Foltynie, T., Ban, M., Robbins, T. W., et al. (2009). The distinct cognitive syndromes of Parkinson's disease: 5 year follow-up of the CamPaIGN cohort. Brain, 132(Pt 11), 2958–2969. doi:10.1093/brain/awp245.
Worsley, K. J., Marrett, S., Neelin, P., Vandal, A. C., Friston, K. J., & Evans, A. C. (1996). A unified statistical approach for determining significant signals in images of cerebral activation. Human Brain Mapping, 4(1), 58–73. doi:10.1002/(SICI)1097-0193(1996)4:1<58::AID-HBM4>3.0.CO;2-O10.1002/(SICI)1097-0193(1996)4:1 < 58::AID-HBM4 > 3.0.CO;2-O.
Acknowledgments
The work of Frederic Sampedro is supported by a Spanish Government FPU doctoral grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Financial disclosures
Saul Martinez-Horta, Frederic Sampedro, Ramon Fernandez-Bobadilla and Juan Marin-Lahoz declare that they have no conflict of interest.
Javier Pagonabarraga: Has received honoraria for lecturing or consultation from Boehringer Ingelheim, UCB, Allergan, Ipsen, and Lundbeck.
Jaime Kulisevsky: Has received honoraria for lecturing or consultation from the Michael J Fox Foundation, Merck Serono, AbbVie, Boehringer Ingelheim, UCB, Zambon, MSD, Italfarmaco, General Electric, and Lundbeck.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, and the applicable revisions at the time of the investigation. Informed consent was obtained from all patients for being included in the study.
Conflict of interest
All the authors report no conflict of interest.
Funding sources
This study was partially funded by public research grants from CIBERNED (Fundación CIEN, Instituto de Salud Carlos III, Spain). The work of Frederic Sampedro is supported by a Spanish Government FPU doctoral grant.
Additional information
Saul Martinez-Horta and Frederic Sampedro are contributed equally to this work
Rights and permissions
About this article
Cite this article
Martinez-Horta, S., Sampedro, F., Pagonabarraga, J. et al. Non-demented Parkinson’s disease patients with apathy show decreased grey matter volume in key executive and reward-related nodes. Brain Imaging and Behavior 11, 1334–1342 (2017). https://doi.org/10.1007/s11682-016-9607-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11682-016-9607-5