Abstract
Previously, studies have demonstrated cortical impairments in those who complete or attempt suicide. Subcortical nuclei have less often been implicated in the suicidal vulnerability. In the present study, we investigated, with a specific design in a large population, variations in the volume of subcortical structures in patients with mood disorders who have attempted suicide. We recruited 253 participants: 73 suicide attempters with a past history of both mood disorders and suicidal act, 89 patient controls with a past history of mood disorders but no history of suicidal act, and 91 healthy controls. We collected 1.5 T magnetic resonance imaging data from the caudate, pallidum, putamen, nucleus accumbens, hippocampus, amygdala, ventral diencephalon, and thalamus. Surface-based morphometry (Freesurfer) analysis was used to comprehensively evaluate gray matter volumes. In comparison to controls, suicide attempters showed no difference in subcortical volumes when controlled for intracranial volume. However, within attempters negative correlations between the left (r = −0.35, p = 0.002), and right (r = −0.41, p < 0.0005) nucleus accumbens volumes and the lethality of the last suicidal act were found. Our study found no differences in the volume of eight subcortical nuclei between suicide attempters and controls, suggesting a lack of association between these regions and suicidal behavior in general. However, individual variations in nucleus accumbens structure and functioning may modulate the lethality of suicidal acts during a suicidal crisis. The known role of nucleus accumbens in action selection toward goals determined by the prefrontal cortex, decision-making or mental pain processing are hypothesized to be potential explanations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
With one million deaths and 10–20 million suicide attempts every year, suicidal behavior is a major source of mortality and morbidity (Hawton and van Heeringen 2009; Lesage et al. 2012). In young adults, suicide ranks amongst the leading causes of premature death, and hence its prevention constitutes an important societal priority. The identification of factors facilitating suicide is one major avenue toward improved prevention. To date, the assessment of suicidal risk relies entirely on socio-demographic and clinical factors. These factors often have high sensitivity but limited specificity (Pokorny 1983). Consequently, more specific assessment tools are needed to substantiate suicidal risk in addition to the clinical assessment.
Suicide is often modeled as a complex behavior resulting from the interaction of acute stressors, such as interpersonal conflicts or loss, with predisposing factors (Mann 2003). Research has identified several elements of the suicidal diathesis, including brain alterations and neurocognitive dysfunctions (Jollant et al. 2011). Brain imaging is emerging as a promising way of improving the evaluation of suicidal risk through the identification of brain markers. Moreover, structural neuroimaging acquisition is widely available in Western countries, which could facilitate its clinical use. One goal of this study was, therefore, to test the ability of a “simple” 1.5 T structural neuroimaging sequence to discriminate suicide attempters from non-attempters.
Structural brain anomalies of suicide attempters have mainly been found in the prefrontal cortex (Jollant et al. 2011). However, differences in subcortical regions are suspected regarding their role in emotional and behavioral regulation (Herrero et al. 2002; Haber and Calzavara 2009; Ochsner et al. 2012). Not surprisingly, several studies have reported structural changes in these regions in suicide attempters and completers. Increased right amygdala volume has been associated with a history of suicide attempts in patients with depression (Monkul et al. 2007) and schizophrenia (Spoletini et al. 2011). Decreased volumes in the right caudate (Benedetti et al. 2011; Vang et al. 2010) and globus pallidus (Vang et al. 2010) have also been described in depressed patients with a history of at least one suicide attempt. Volumes in the right caudate were also found to be reduced when the experimental sample aggregated patients with a familial history of a suicidal gesture with patients with a history of a suicide attempt in a single group considered to be at a high risk of suicide (Wagner et al. 2011). Elderly suicide attempters showed reduced voxel counts in the putamen (Dombrovski et al. 2012). Moreover, the thalamus has similarly been implicated in a neuroimaging study (Benedetti et al. 2011) and in a volumetric post-mortem study (Young et al. 2008). Taken together, there is substantial evidence to suggest that several subcortical structures may be structurally altered in suicide attempters and completers, and may represent relevant biomarkers of suicidal behavior.
Despite specific findings associated with suicidal behavior, the hitherto published structural neuroimaging literature suffers from several limitations that the present study aims to address. Many recent studies assessed small sample sizes, as few as seven to ten suicide attempters (Vang et al. 2010; Monkul et al. 2007), which limit their statistical power and increase the risk of false positives and negatives. Our study constitutes the largest structural Magnetic Resonance Imaging (MRI) study specifically targeting suicidal behavior in mood disorders. Only one other large study, in psychotic disorders, has been conducted to date (Giakoumatos et al. 2013). Furthermore, we used previously validated and a priori-chosen study design (Jollant et al. 2005) with the inclusion of non-depressed patients to exclude the acute effect of the depressive state, and a group of patients with a history of mood disorder but not suicide attempt to exclude the effect of co-morbid disorders while specifically examining suicide vulnerability.
Based on previous findings, we hypothesized that suicide attempters vs. controls would show volumetric differences in subcortical nuclei, including the basal ganglia, the amygdala and the thalamus.
Materials and methods
Population
Participants were 73 suicide attempters (SA), 89 patient controls (PC) and 91 healthy controls (HC). SA were individuals with a personal history of both suicidal behavior and mood disorder; PC individuals with a personal history of mood disorder but no lifetime personal history of suicidal behavior; HC were individuals with no current or past history of any major DSM-IV Axis I diagnoses and no history of suicidal behavior. Suicidal acts were defined as any non-fatal, self-inflicted potentially injurious behavior committed with any intent to die as a result of the behavior (Mann 2003). This definition, therefore, excludes non-suicidal self-injuries and aborted suicidal acts. Psychiatric diagnoses were based on DSM-IV-TR criteria (APA 2000).
The study pools three samples, one recruited at the Institute of Psychiatry in London, United Kingdom (sample 1), and two recruited independently at the academic hospital of Montpellier, France (samples 2 and 3). The three samples only differed in two selection criteria: 1) Samples 1 and 2 comprised only males aged between 18 and 60 whereas Sample 3 comprised only non-menopausal females aged between 18 and 50; 2) All patients in Sample 1 suffered from major depressive disorder (MDD) whereas Samples 2 and 3 included both major depressive disorder and bipolar disorders. Participants were excluded if they had a lifetime history of severe head trauma, central nervous system disorders, schizophrenia, and substance use disorder over the last 12 months, suicide attempt using firearms, pregnancy, and contraindications to MRI. Only right-handed individuals checked by the Edinburgh handedness index (Oldfield 1971) were recruited. Details on excluded participants from each sample are given in Supplementary Material.
Assessment
For all samples, patients were enrolled through advertising and in outpatient clinics. After an initial screening interview, an experienced clinical psychiatrist interviewed selected participants. All DSM-IV diagnoses were made using the Mini-International Neuropsychiatric Interview, version 5.0.0. (Sheehan et al. 1998). Symptom severity was assessed by the Hamilton Depression Rating Scale (HDRS) (Hamilton 1960) and the Beck Depression Inventory (BDI) (Beck et al. 1961). All subjects were euthymic during scanning, with a HDRS below 7. The last and the most severe suicidal acts were assessed using the Risk Rescue Rating Scale (RRRS) (Weisman and Worden 1972) and the Suicide Intent Scale (SIS) (Beck et al. 1974). The French or English versions of the National Adult Reading Test (NART) (Beardsall and Brayne 1990) were used to provide an estimation of verbal IQ. Barratt Impulsiveness Scale (BIS) version 10 was also used (Patton et al. 1995).
After complete description of the study to the subjects, written informed consent was obtained from all participants. The protocol was approved by respective site research ethics committees (Institute of Psychiatry or Montpellier Hospital research ethics board). Participants received compensation of £30 or 100€, respectively. A study with the same 3 samples has recently been published (Ding et al. in press).
MRI acquisition procedures and analysis
T1-weighted magnetic resonance images were acquired using a GE Signa 1.5 T Neuro-optimized MR system (General Electric, Milwaukee) in sample 1, and with a 1.5 whole-body MRI system (MAGNETON AVANTO, Siemens, Erlangen, Germany) in sample 2 and 3. Sample 1 used a spoiled gradient echo sequence with the following parameters: isotropic voxel dimension of 1.1 mm with field-of-view at 280 × 180 mm; TE of 5 ms and TR of 10.8 ms. 2D matrix 256 × 160 with 150 slices acquired, bandwidth of 122 Hz/pixel. Sample 2 used 3D T1 FLASH sequence with voxel dimension of 0.93 × 0.93 × 1 mm, field-of-view at 240 × 240 mm, matrix 256 × 256, 15 degrees Flip angle, TE of 5.2 ms and TR of 11 ms with 160 slices, bandwidth of 130 Hz/pixel. Sample 3 used 3DT1 MPRAGE with voxel dimension of 0.98 mm × 0.98 mm × 1 mm, field-of-view at 250 × 250 mm, matrix 256 × 256 with 160 slices, 15 degrees flip angle, TE of 4.1 ms, TR of 2100 ms and TI of 1100 ms, bandwidth of 140 Hz/pixel.
Surface-based morphometry (SBM) analyses were conducted using the Freesurfer image analysis suite (version v 5.1.0) (http://surfer.nmr.mgh.harvard.edu). The technical details and references for these procedures are described in prior publications listed online (http://surfer.nmr.mgh.harvard.edu/fswiki/FreeSurferWiki#References). Briefly, the processing includes motion correction (Reuter et al. 2010), removal of non-brain tissue using a hybrid watershed/surface deformation procedure (Segonne et al. 2004), automated Talairach transformation, segmentation of the subcortical white matter and deep gray matter volumetric structures (Fischl et al. 2002, 2004) intensity normalization (Sled et al. 1998), tessellation of the gray matter/white matter boundary, automated topology correction (Fischl et al. 2001; Segonne et al. 2007), and surface deformation following intensity gradients to optimally place the gray/white and gray/cerebrospinal fluid borders at the location where the greatest shift in intensity defines the transition to the other tissue class (Dale et al. 1999; Fischl and Dale 2000). FreeSurfer results were evaluated using the QDEC, and TkSurfer tools.
This study examined 8 subcortical regions namely the amygdala, hippocampus, caudate, globus pallidus, putamen, nucleus accumbens, ventral diencephalon, and thalamus. FreeSurfer performs an automatic subcortical segmentation, where each voxel in the normalized brain volume is assigned a label (including the 8 subcortical regions studied). Automatic segmentation of subcortical structures is based on an atlas containing probabilistic information on the location of structures (Fischl et al. 2002). This automated classification technique compares in accuracy with manual labeling, and was shown to be sufficiently sensitive to robustly detect changes in subcortical structures that predispose to the onset of major neurocognitive disorder (Fischl et al. 2002).
Although multi-site neuroimaging poses challenges, samples can be combined and analyzed when groups are balanced across samples (which is the case here, see tables in Supplementary Material) and multi-site samples are properly controlled for in the analysis (Pardoe et al. 2008; Takao et al. 2014). Group comparisons in volumes were also systematically controlled for intracranial volume (Buckner et al. 2004). Additional covariates were used as needed (see below).
Statistical analyses
Unpaired T-tests and ANOVA (followed by Tukey post-hoc pairwise comparisons if significant) were used to compare quantitative variables across groups. Qualitative variables were compared using a chi-squared test. Confounding variables (sample, age, level of education, intracranial volume, bipolar disorder, medication) were controlled using a multivariate general linear model. The ANOVA threshold for statistical analyses was set at a very conservative p < 0.003 (p < 0.05 divided by 8 subcortical structures × 2 sides) for statistical significance. Statistical analyses were carried out with SPSS.21 (IBM Corp., Armonk, NY). As recent reports underlined the limits of using the p-value in group comparison (Nuzzo 2014), we additionally calculated Cohen’s d effect sizes based on marginal means (taking into account the intracranial volume and sample) for each main comparisons i.e., between SA and PC. In order to parse the effect of different mood disorders, subanalyses were conducted with patients with unipolar depression only (from all 3 samples) or with patients with bipolar disorder only (from sample 2 and 3). Pearson product–moment correlation coefficients were computed to assess the relationship between the diverse sets of clinical measures (BDI, HDRS, NART, RSSS, SIS, BIS) and the subcortical volumes, using the same conservative statistical threshold (p < 0.003). Finally, we also conducted a multivariate ANCOVA to determine the effect of psychotropic medications on subcortical volumes in patients with mood disorders (PC and SA together), controlling for sample and intracranial volume.
Results
Socio-demographic and clinical comparisons
All three groups were equally distributed across the three samples. Comparison of socio-demographic and clinical variables across the three participant groups in the pooled sample (Table 1) showed that SA and PC were largely similar on all variables with the exception of higher use of antipsychotics and anxiolytics in SA. HC had a higher proportion of males and had more years of education. Also, patients had significantly higher HDRS and BDI scores than HC despite being below the threshold for depression. We did not covary for this latter variable as it was related to patient status.
Neuroimaging group comparisons
ANOVA revealed significant group differences (all p < 0.003) for left amygdala, left ventral diencephalon, and right hippocampus. However, none of these differences survived corrections for intracranial volume and sample, even after covarying for age, gender, level of education, bipolar disorder, and medication intake. All subcortical brain regions had minimal and non-significant effect sizes (Table 2). Moreover, subanalyses restricted to patients with unipolar depression or to patient with bipolar disorder yielded similar negative results. Intracranial volume was significantly different between groups after accounting for sample (F = 3.2, p = 0.04), but did not differ between SA and PC.
Clinical correlations
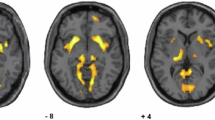
The lethality of the last suicidal act (as measured with the first part of the RRRS) was negatively correlated with the left (r = −0.35, n = 73, p = 0.002), and right accumbens volume (r = −0.41, n = 73, p < 0.0005). Scatterplots summarize these results (Fig. 1). Removing two outliers did not modify the results. After controlling for the effect of sample, gender, age, intracranial volume, BIS scores, NART scores, bipolar status and medication using partial correlations, these associations remained significant. The impulsivity score on the BIS did not correlate significantly with accumbens volumes when controlling for sample. HAMD negatively correlated with the right pallidum (r = −0.35, n = 253, p = 0.002). BDI and SIS did not correlate with any subcortical volumes.
Secondary analyses: effect of psychotropic medication
In order to determine the effect of medication on subcortical volumes in patients with mood disorders (PC and SA together), we conducted a MANCOVA controlling for sample and intracranial volume. Medication status as a whole did not have a significant overall effect on subcortical volumes (Wilks lambda F = 1.246, p = 0.2). When examining medication type, we did not find any effect of antidepressants, lithium, or antiepileptics on subcortical volumes. However, antipsychotics were associated with a general group effect on subcortical volumes (Wilks Lambda F = 1.801; p = 0.04; partial Eta square = 0.17). More specifically, antipsychotics were associated with smaller bilateral hippocampus and left ventral diencephalon. Additionally, benzodiazepines and hypnotics also had a significant global effect on subcortical volumes (Wilks’ Lambda F = 2.10, p = 0.01, partial Eta Squared = 0.19) with smaller bilateral hippocampus.
Discussion
We present here findings from the largest neuroimaging study conducted in suicidal behavior and mood disorders to date, with a specific design for investigating vulnerability to suicidal behavior taking into account comorbid mood disorders. Exploring subcortical nuclei volumes measured by 1.5 T MRI and using the surface-based morphometry tool Freesurfer, no significant group differences were detected in any of the 8 regions after controlling for sample and intracranial volumes. However, analysis revealed a negative correlation between the size of the accumbens nuclei and the lethality of the last suicidal act.
Our findings, based on a large population, do not support reports of volumetric differences in subcortical structures previously identified in suicidal behavior. Our results suggest that suicidal risk in mood disorders is inherently uncorrelated with subcortical volumes. The discrepancy with prior reports might be attributable to methodological differences including smaller samples increasing the risk of type-I errors, non-automatized tracing technique, the use of more liberal statistical threshold or idiosyncratic sample characteristics. Alternatively, differences in other reports could be explained by a higher intensity of the magnetic field used, although most positive reports used similar magnetic intensity (1.5 T) or similar voxel size (1 × 1 × 1 mm). For instance, Monkul et al. (Monkul et al. 2007), using a manual tracing technique and a 1.5 T magnetic field, found that suicide attempters had larger right amygdala. However, their sample consisted of only 7 suicide attempters, all females with MDD. Our own subanalysis in females with MDD, which comprised 23 SA, 30 PC and 29 HC, found no significant association with the right or left amygdala, nor any other subcortical regions. Spoletini et al. (Spoletini et al. 2011) with a larger sample of schizophrenic patients and using FSL, also reported increased amygdala volume (using 3 T magnetic field but similarly sized millimetric voxel). In contrast, Soloff et al. (Soloff et al. 2012) found no amygdalar differences between SA and PC in patients with borderline personality disorder using voxel-based morphometry (VBM).
Similarly, we found no volumetric differences in basal ganglia structures between SA and controls. This contrasts with reports of smaller right caudate nuclei (Vang et al. 2010; Wagner et al. 2011) and globus pallidus (Vang et al. 2010) using VBM or Freesurfer. Again, these prior reports had limited numbers of subjects which increase the likelihood of false positives: Wagner et al. (Wagner et al. 2011) had only 15 depressed subjects “at high risk for suicide” (some of them had never attempted suicide but had a family history of suicide) and Vang et al. (Vang et al. 2010) had only 7 SA, which were compared to 6 HC therefore limiting any definitive conclusion. In larger samples and using VBM, Benedetti et al. (Benedetti et al. 2011) reported smaller “basal ganglia” in 19 SA vs. 38 PC with bipolar disorder, and Dombrovski et al. (Dombrovski et al. 2012) found reduced putamen, but not pallidum or caudate, voxels counts in 13 elderly SA vs. 20 PC with depression. Only the report by Dombrovski et al. employed high magnetic filed (3 T), affording a better resolution, which could explain a difference with our findings.
The thalamus was previously implicated in the suicidal diathesis through neuroimaging studies showing reduced grey matter volumes in SA with bipolar (Benedetti et al. 2011) and psychotic disorders (Giakoumatos et al. 2013) (using VBM or Freesurfer, respectively). Our findings were not consistent with this in either our complete population or the bipolar patient sub-group. A lack of association was also reported by Spoletini and colleagues (Spoletini et al. 2011) whereas Lopez-Larson et al. (Lopez-Larson et al. 2013) reported increased thalamic volumes in SA vs PC in a complex population of depressed veterans with mild traumatic brain injury, using Freesurfer.
Finally, to our knowledge, hippocampal volume, although largely investigated in relation to mood disorders (Videbech and Ravnkilde 2004) and trauma history (Frodl and O’Keane 2013), was never directly associated with suicidal behavior (Soloff et al. 2012). Our study confirms the lack of a direct relationship. It is possible that hippocampal alterations are mainly the result of early traumatic events and, therefore, only affect a subset of SA (Turecki et al. 2012).
Although nucleus accumbens volumes did not discriminate attempters and non-attempters in general, our analyses suggest that this structure could modulate the lethality of the suicidal act i.e., medical consequences of the act. In as much as suicide is not a homogenous behavior at the clinical level, it is unlikely a homogenous phenomenon at the biological level. The common issue of phenotypic heterogeneity in psychiatry (Kapur et al. 2012) may explain the difficulty in finding reliable, reproducible group differences. Moreover, suicidal behaviors are complex acts varying in terms of intent, planification, or lethality.
Previous neuroimaging studies have suggested that some brain regions may modulate certain aspects of suicidal acts. Activity at rest in the medial prefrontal and anterior cingulate cortices has been correlated with impulsivity and suicidal intent (Oquendo et al. 2003). Correlations between basal ganglia structures and suicidal dimensions, or factors relevant to suicide, have also been found. For example, smaller putamen in elderly suicidal patients has been correlated with higher reward delay discounting (Dombrovski et al. 2012). Vang et al. (Vang et al. 2010) found a negative correlation between globus pallidus volumes and measures of impulsivity in suicidal patients (although we could not confirm this latter association in our study).
To date, the mechanisms linking the nucleus accumbens and the lethality of the suicidal act have not been investigated. However, based on related prior findings, some hypotheses can be suggested. Lethality reflects the consequences of different interacting factors including the level of suicidal intent, the choice of a suicidal method and, to a certain degree, the physical resistance of the individual. Of note, individuals committing more lethal acts seem to be closer to suicide completers than low-lethality attempters (Giner et al. 2014). In terms of the role of the nucleus accumbens, it is located at “the interface between cognition, emotion and action” (Floresco 2014), receiving inputs from the prefrontal cortex, hippocampus, basolateral amygdala and ventral tegmental area, and projecting toward motor effectors. This region has been involved in action selection (Leotti and Delgado 2011), notably in situations of ambiguity, based on goals defined by cortical regions. The nucleus accumbens may particularly bias the intensity and direction of planned actions. In a situation of suicidal crisis, the nucleus accumbens could therefore be implicated, not in committing a suicidal act per se, but in selecting the specific actions associated with this act, with suicidal intent (the goal) being encoded by and transmitted from the prefrontal cortex (Oquendo et al. 2003). Moreover, the nucleus accumbens encodes positive prediction error (McGinty et al. 2013; Dombrovski et al. 2013), and is involved in decision-making (Kuhnen and Knutson 2005). Impaired decision-making has been robustly found in suicide attempters (Richard-Devantoy et al. 2014), notably those using a violent mean (Jollant et al. 2005). Use of violent suicidal means has in turn been associated with more lethality (Giner et al. 2014). Dysfunctional nucleus accumbens activity in some individuals may therefore underlie disadvantageous decision-making, but also the choice of a more violent mean in a stressful situation, increasing the risk of serious medical consequences and death. Finally, the nucleus accumbens has been associated with psychological pain processing (O’Connor et al. 2008). Increased psychological pain has been linked to increased risk of suicidal acts (Olie et al. 2010). Moreover, a recent study suggest that mental pain interacts with difficulty communicating to modulate lethality (Levi-Belz et al. 2014). Nucleus Accumbens may therefore be the link between mental pain and suicide lethality. The link between these various factors (lethality, mental pain, impaired decision-making, violent acts) and the functional and structural integrity of the nucleus accumbens should be further investigated in future studies.
Although not specifically designed to address this question, secondary analyses emphasize the importance of taking into account medication status when examining subcortical volumes. We found antipsychotics and benzodiazepines to be associated with reduced volumes of the hippocampus in all patients together. A recent study in schizophrenia demonstrated that atypical antipsychotics were associated with decreased left hippocampal volume, which correlated with a decrease in serum BDNF levels (Rizos et al. 2014). There is limited neuroimaging evidence of the effect of antipsychotics on subcortical volumes in mood disorders. This question necessitates specific investigation.
Our study had several methodological limitations. The main limitation in our analysis of subcortical nuclei was that our data were pooled across three sites. This procedure added supplementary heterogeneity because it was not designed as a priori multi-center study, which resulted in different acquisition parameters (slices, TE, TR) from two different scanners. Covarying for the sites was therefore necessary although it might have decreased the power to detect differences (Glover et al. 2012). Nonetheless, the risk of type II errors may have been counterbalanced by the large sample size (n = 253) of our study, which was balanced across the three sites (see Supplementary Material). Indeed, analysis of cortical regions in the same samples revealed significant between-group differences in several prefrontal regions, despite covarying for the effect of the sample (Ding et al. in press). Secondly, given that data in males and females were obtained with different scanning procedures, examination of gender effects was not possible to distinguish from difference in scanning techniques. Our data were obtained with 1.5 T MRI scanners, which might lack the necessary power to detect subtle alterations. Higher isotropic resolution could theoretically render more accurate volumetric measurements of subcortical brain structures (Wu et al. 2010) and reduce systematic errors in registration (Simon et al. 1997). Fourth, different results among studies that have investigated volumetric differences may stem from the use of different analysis methods. Finally, we must take into account the heterogeneity in the psychiatric populations studied, which included moderately to severely ill and often medicated patients in order to be representative. Although, these medical factors were controlled for, this may have, nonetheless, resulted in additional heterogeneity.
In conclusion, this study adds new findings to the growing literature on the neurocognitive basis of suicidal behavior. No general association between subcortical volumes and suicidal behaviors could be confirmed contrary to what has been found in various cortical regions. New acquisition and analysis procedures may be necessary. However, our study also suggests that the nucleus accumbens may modulate the lethality of suicidal acts. More research is needed to understand the role of subcortical structures, and their link with cortical regions, in the development of the suicidal crisis and the modulation of this complex behavior.
References
APA (2000). Diagnostic and statistical manual of mental disorders (4th ed.). Washington: American Psychiatric Association.
Beardsall, L., & Brayne, C. (1990). Estimation of verbal intelligence in an elderly community: a prediction analysis using a shortened NART. The British Journal of Clinical Psychology, 29(Pt 1), 83–90.
Beck, A. T., Ward, C. H., Mendelson, M., Mock, J., & Erbaugh, J. (1961). An inventory for measuring depression. Archives of General Psychiatry, 4, 561–571.
Beck, R. W., Morris, J. B., & Beck, A. T. (1974). Cross-validation of the suicidal intent scale. Psychological Reports, 34(2), 445–446. doi:10.2466/pr0.1974.34.2.445.
Benedetti, F., Radaelli, D., Poletti, S., Locatelli, C., Falini, A., Colombo, C., et al. (2011). Opposite effects of suicidality and lithium on gray matter volumes in bipolar depression. Journal of Affective Disorders, 135(1–3), 139–147. doi:10.1016/j.jad.2011.07.006.
Buckner, R. L., Head, D., Parker, J., Fotenos, A. F., Marcus, D., Morris, J. C., et al. (2004). A unified approach for morphometric and functional data analysis in young, old, and demented adults using automated atlas-based head size normalization: reliability and validation against manual measurement of total intracranial volume. NeuroImage, 23(2), 724–738. doi:10.1016/j.neuroimage.2004.06.018.
Dale, A. M., Fischl, B., & Sereno, M. I. (1999). Cortical surface-based analysis. I. Segmentation and surface reconstruction. NeuroImage, 9(2), 179–194. doi:10.1006/nimg.1998.0395.
Ding, Y., Lawrence, N., Olie, E., Cyprien, F., le Bars, E., Bonafe, A., et al. (in press). Prefrontal cortex markers of suicidal vulnerability in mood disorders: a model-based structural neuroimaging study with a translational perspective. Transl Psychiatry.
Dombrovski, A. Y., Siegle, G. J., Szanto, K., Clark, L., Reynolds, C. F., & Aizenstein, H. (2012). The temptation of suicide: Striatal gray matter, discounting of delayed rewards, and suicide attempts in late-life depression. Psychological Medicine, 42(6), 1203–1215. doi:10.1017/S0033291711002133.
Dombrovski, A. Y., Szanto, K., Clark, L., Reynolds, C. F., & Siegle, G. J. (2013). Reward signals, attempted suicide, and impulsivity in late-life depression. JAMA Psychiatry. doi:10.1001/jamapsychiatry.2013.75.
Fischl, B., & Dale, A. M. (2000). Measuring the thickness of the human cerebral cortex from magnetic resonance images. Proceedings of the National Academy of Sciences of the United States of America, 97(20), 11050–11055. doi:10.1073/pnas.200033797.
Fischl, B., Liu, A., & Dale, A. M. (2001). Automated manifold surgery: constructing geometrically accurate and topologically correct models of the human cerebral cortex. IEEE Transactions on Medical Imaging, 20(1), 70–80. doi:10.1109/42.906426.
Fischl, B., Salat, D. H., Busa, E., Albert, M., Dieterich, M., Haselgrove, C., et al. (2002). Whole brain segmentation: automated labeling of neuroanatomical structures in the human brain. Neuron, 33(3), 341–355.
Fischl, B., Salat, D. H., van der Kouwe, A. J., Makris, N., Segonne, F., Quinn, B. T., et al. (2004). Sequence-independent segmentation of magnetic resonance images. NeuroImage, 23(Suppl 1), S69–84. doi:10.1016/j.neuroimage.2004.07.016.
Floresco, S. B. (2014). The nucleus accumbens: an interface between cognition, emotion, and action. Annual Review of Psychology. doi:10.1146/annurev-psych-010213-115159.
Frodl, T., & O’Keane, V. (2013). How does the brain deal with cumulative stress? a review with focus on developmental stress, HPA axis function and Hippocampal structure in humans. Neurobiology of Disease, 52, 24–37. doi:10.1016/j.nbd.2012.03.012.
Giakoumatos, C. I., Tandon, N., Shah, J., Mathew, I. T., Brady, R. O., Clementz, B. A., et al. (2013). Are structural brain abnormalities associated with suicidal behavior in patients with psychotic disorders? Journal of Psychiatric Research, 47(10), 1389–1395. doi:10.1016/j.jpsychires.2013.06.011.
Giner, L., Jaussent, I., Olie, E., Beziat, S., Guillaume, S., Baca-Garcia, E., et al. (2014). Violent and serious suicide attempters: one step closer to suicide? The Journal of Clinical Psychiatry, 75(3), e191–197. doi:10.4088/JCP.13m08524.
Glover, G. H., Mueller, B. A., Turner, J. A., van Erp, T. G., Liu, T. T., Greve, D. N., et al. (2012). Function biomedical informatics research network recommendations for prospective multicenter functional MRI studies. Journal of Magnetic Resonance Imaging, 36(1), 39–54. doi:10.1002/jmri.23572.
Haber, S. N., & Calzavara, R. (2009). The cortico-basal ganglia integrative network: the role of the thalamus. Brain Research Bulletin, 78(2–3), 69–74. doi:10.1016/j.brainresbull.2008.09.013.
Hamilton, M. (1960). A rating scale for depression. Journal of Neurology, Neurosurgery and Psychiatry, 23, 56–62.
Hawton, K., & van Heeringen, K. (2009). Suicide. Lancet, 373(9672), 1372–1381. doi:10.1016/S0140-6736(09)60372-X.
Herrero, M. T., Barcia, C., & Navarro, J. M. (2002). Functional anatomy of thalamus and basal ganglia. Child’s Nervous System, 18(8), 386–404. doi:10.1007/s00381-002-0604-1.
Jollant, F., Bellivier, F., Leboyer, M., Astruc, B., Torres, S., Verdier, R., et al. (2005). Impaired decision making in suicide attempters. The American Journal of Psychiatry, 162(2), 304–310. doi:10.1176/appi.ajp.162.2.304.
Jollant, F., Lawrence, N. L., Olie, E., Guillaume, S., & Courtet, P. (2011). The suicidal mind and brain: a review of neuropsychological and neuroimaging studies. The World Journal of Biological Psychiatry, 12(5), 319–339. doi:10.3109/15622975.2011.556200.
Kapur, S., Phillips, A. G., & Insel, T. R. (2012). Why has it taken so long for biological psychiatry to develop clinical tests and what to do about it? Molecular Psychiatry, 17(12), 1174–1179. doi:10.1038/mp.2012.105.
Kuhnen, C. M., & Knutson, B. (2005). The neural basis of financial risk taking. Neuron, 47(5), 763–770. doi:10.1016/j.neuron.2005.08.008.
Leotti, L. A., & Delgado, M. R. (2011). The inherent reward of choice. Psychological Science, 22(10), 1310–1318. doi:10.1177/0956797611417005.
Lesage, A., Moubarac, J. C., Desrochers, L., & Turecki, G. (2012). Interdisciplinary dialogue on the etiology and prevention of suicide in Quebec]. [editorial. Santé Mentale au Québec, 37(2), 25–30.
Levi-Belz, Y., Gvion, Y., Horesh, N., Fischel, T., Treves, I., Or, E., et al. (2014). Mental pain, communication difficulties, and medically serious suicide attempts: a case–control study. Archives of Suicide Research, 18(1), 74–87. doi:10.1080/13811118.2013.809041.
Lopez-Larson, M., King, J. B., McGlade, E., Bueler, E., Stoeckel, A., Epstein, D. J., et al. (2013). Enlarged thalamic volumes and increased fractional anisotropy in the thalamic radiations in veterans with suicide behaviors. Front in Psychiatry, 4, 83. doi:10.3389/fpsyt.2013.00083.
Mann, J. J. (2003). Neurobiology of suicidal behaviour. Nature Review Neuroscience, 4(10), 819–828. doi:10.1038/nrn1220.
McGinty, V. B., Lardeux, S., Taha, S. A., Kim, J. J., & Nicola, S. M. (2013). Invigoration of reward seeking by cue and proximity encoding in the nucleus accumbens. Neuron, 78(5), 910–922. doi:10.1016/j.neuron.2013.04.010.
Monkul, E. S., Hatch, J. P., Nicoletti, M. A., Spence, S., Brambilla, P., Lacerda, A. L., et al. (2007). Fronto-limbic brain structures in suicidal and non-suicidal female patients with major depressive disorder. Molecular Psychiatry, 12(4), 360–366. doi:10.1038/sj.mp.4001919.
Nuzzo, R. (2014). Scientific method: statistical errors. Nature, 506(7487), 150–152. doi:10.1038/506150a.
O’Connor, M. F., Wellisch, D. K., Stanton, A. L., Eisenberger, N. I., Irwin, M. R., & Lieberman, M. D. (2008). Craving love? enduring grief activates brain’s reward center. NeuroImage, 42(2), 969–972. doi:10.1016/j.neuroimage.2008.04.256.
Ochsner, K. N., Silvers, J. A., & Buhle, J. T. (2012). Functional imaging studies of emotion regulation: a synthetic review and evolving model of the cognitive control of emotion. The Annals of the New York Academy of Sciences, 1251, E1–24. doi:10.1111/j.1749-6632.2012.06751.x.
Oldfield, R. C. (1971). The assessment and analysis of handedness: the Edinburgh inventory. Neuropsychologia, 9(1), 97–113.
Olie, E., Guillaume, S., Jaussent, I., Courtet, P., & Jollant, F. (2010). Higher psychological pain during a major depressive episode may be a factor of vulnerability to suicidal ideation and act. Journal of Affective Disorders, 120(1–3), 226–230. doi:10.1016/j.jad.2009.03.013.
Oquendo, M. A., Placidi, G. P., Malone, K. M., Campbell, C., Keilp, J., Brodsky, B., et al. (2003). Positron emission tomography of regional brain metabolic responses to a serotonergic challenge and lethality of suicide attempts in major depression. Archives of General Psychiatry, 60(1), 14–22.
Pardoe, H., Pell, G. S., Abbott, D. F., Berg, A. T., & Jackson, G. D. (2008). Multi-site voxel-based morphometry: methods and a feasibility demonstration with childhood absence epilepsy. NeuroImage, 42(2), 611–616. doi:10.1016/j.neuroimage.2008.05.007.
Patton, J. H., Stanford, M. S., & Barratt, E. S. (1995). Factor structure of the Barratt impulsiveness scale. Journal of Clinical Psychology, 51(6), 768–774.
Pokorny, A. D. (1983). Prediction of suicide in psychiatric patients. Report of a prospective study. Archives of General Psychiatry, 40(3), 249–257.
Reuter, M., Rosas, H. D., & Fischl, B. (2010). Highly accurate inverse consistent registration: a robust approach. NeuroImage, 53(4), 1181–1196. doi:10.1016/j.neuroimage.2010.07.020.
Richard-Devantoy, S., Berlim, M. T., & Jollant, F. (2014). A meta-analysis of neuropsychological markers of vulnerability to suicidal behavior in mood disorders. Psychological Medicine, 44(8), 1663–1673. doi:10.1017/S0033291713002304.
Rizos, E., Papathanasiou, M. A., Michalopoulou, P. G., Laskos, E., Mazioti, A., Kastania, A., et al. (2014). A longitudinal study of alterations of Hippocampal volumes and serum BDNF levels in association to atypical antipsychotics in a sample of first-episode patients with schizophrenia. PLoS One, 9(2), e87997. doi:10.1371/journal.pone.0087997.
Segonne, F., Dale, A. M., Busa, E., Glessner, M., Salat, D., Hahn, H. K., et al. (2004). A hybrid approach to the skull stripping problem in MRI. NeuroImage, 22(3), 1060–1075. doi:10.1016/j.neuroimage.2004.03.032.
Segonne, F., Pacheco, J., & Fischl, B. (2007). Geometrically accurate topology-correction of cortical surfaces using nonseparating loops. IEEE Transactions on Medical Imaging, 26(4), 518–529. doi:10.1109/TMI.2006.887364.
Sheehan, D. V., Lecrubier, Y., Sheehan, K. H., Amorim, P., Janavs, J., Weiller, E., et al. (1998). The mini-international neuropsychiatric interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. The Journal of Clinical Psychiatry, 59(20), 22–33. quiz 34–57.
Simon, J. H., Scherzinger, A., Raff, U., & Li, X. (1997). Computerized method of lesion volume quantitation in multiple sclerosis: error of serial studies. AJNR. American Journal of Neuroradiology, 18(3), 580–582.
Sled, J. G., Zijdenbos, A. P., & Evans, A. C. (1998). A nonparametric method for automatic correction of intensity nonuniformity in MRI data. IEEE Transactions on Medical Imaging, 17(1), 87–97. doi:10.1109/42.668698.
Soloff, P. H., Pruitt, P., Sharma, M., Radwan, J., White, R., & Diwadkar, V. A. (2012). Structural brain abnormalities and suicidal behavior in borderline personality disorder. Journal of Psychiatric Research, 46(4), 516–525. doi:10.1016/j.jpsychires.2012.01.003.
Spoletini, I., Piras, F., Fagioli, S., Rubino, I. A., Martinotti, G., Siracusano, A., et al. (2011). Suicidal attempts and increased right amygdala volume in schizophrenia. Schizophrenia Research, 125(1), 30–40. doi:10.1016/j.schres.2010.08.023.
Takao, H., Hayashi, N., & Ohtomo, K. (2014). Effects of study design in multi-scanner voxel-based morphometry studies. NeuroImage, 84, 133–140. doi:10.1016/j.neuroimage.2013.08.046.
Turecki, G., Ernst, C., Jollant, F., Labonte, B., & Mechawar, N. (2012). The neurodevelopmental origins of suicidal behavior. Trends in Neurosciences, 35(1), 14–23. doi:10.1016/j.tins.2011.11.008.
Vang, F. J., Ryding, E., Traskman-Bendz, L., van Westen, D., & Lindstrom, M. B. (2010). Size of basal ganglia in suicide attempters, and its association with temperament and serotonin transporter density. Psychiatry Research, 183(2), 177–179. doi:10.1016/j.pscychresns.2010.05.007S0925-4927(10)00186-1.
Videbech, P., & Ravnkilde, B. (2004). Hippocampal volume and depression: a meta-analysis of MRI studies. The American Journal of Psychiatry, 161(11), 1957–1966. doi:10.1176/appi.ajp.161.11.1957.
Wagner, G., Koch, K., Schachtzabel, C., Schultz, C. C., Sauer, H., & Schlosser, R. G. (2011). Structural brain alterations in patients with major depressive disorder and high risk for suicide: evidence for a distinct neurobiological entity? NeuroImage, 54(2), 1607–1614. doi:10.1016/j.neuroimage.2010.08.082.
Weisman, A. D., & Worden, J. W. (1972). Risk-rescue rating in suicide assessment. Archives of General Psychiatry, 26(6), 553–560.
Wu, Y., Ragin, A. B., Du, H., Sidharthan, S., Dunkle, E. E., Koktzoglou, I., et al. (2010). Sub-millimeter isotropic MRI for segmentation of subcortical brain regions and brain visualization. Journal of Magnetic Resonance Imaging, 31(4), 980–986. doi:10.1002/jmri.22120.
Young, K. A., Bonkale, W. L., Holcomb, L. A., Hicks, P. B., & German, D. C. (2008). Major depression, 5HTTLPR genotype, suicide and antidepressant influences on thalamic volume. The British Journal of Psychiatry, 192(4), 285–289. doi:10.1192/bjp.bp.107.039180.
Acknowledgments
The authors would like to thank Mrs Corina Nagy for her help in the revision on the manuscript.
Study 1 was supported by the American Foundation for Suicide Prevention (Dr. Jollant), Fondation pour la Recherche Médicale (Action Dynamique en Psychiatrie to Dr Jollant), and the Royal Society and University of London Central Research Fund (to Dr. Lawrence). Study 2 was funded by a Projet Hospitalier de Recherche Clinique (to Drs. Jollant and Courtet). Dr. Olié received a grant from Académie Nationale de Médecine. Study 3 was funded by the Institut Servier (to Dr. Jollant). Dr Cyprien received an MSc grant from Institut Servier.
Mr. Ding currently holds a Fond de Recherche du Québec - Santé (FRQS) Ph.D. Grant # 24117. Dr. Jollant currently holds a “FRQS chercheur-boursier clinicien” salary Award.
Disclosures
Anthony J. Gifuni, Yang Ding, Emilie Olié, Natalia Lawrence, Fabienne Cyprien, Emmanuelle Le Bars, Alain Bonafé, Mary L. Phillips, Philippe Courtet, and Fabrice Jollant declare no conflict of interest.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, and the applicable revisions at the time of the investigation. Informed consent was obtained from all patients for being included in the study.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 114 kb)
Rights and permissions
About this article
Cite this article
Gifuni, A.J., Ding, Y., Olié, E. et al. Subcortical nuclei volumes in suicidal behavior: nucleus accumbens may modulate the lethality of acts.. Brain Imaging and Behavior 10, 96–104 (2016). https://doi.org/10.1007/s11682-015-9369-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11682-015-9369-5