Abstract
Background
Additional pathologies accompanying calcific tendinitis of the rotator cuff still remain unknown. The hypothesis of this study was that there are various additional pathologies accompanying calcific tendinitis, which might need further treatment. This study aimed to document intra-articular pathologies and investigate whether the location and spread of calcific tendinitis are associated with intra-articular pathologies and impairment in range of motion.
Methods
Arthroscopy was performed on 53 patients for chronic calcific tendinitis. Documentation included demographic baseline variables, intraoperative findings of all structures in the glenohumeral joint, range of motion, joint laxity under general anesthesia, and basic details of intraoperative procedures.
Results
In all, 189 additional pathologies were found, 77 during intra-articular arthroscopy. Of all extra- and intra-articular pathologies, 74 and 70%, respectively, required surgical treatment. A mean of 3.6 additional pathologic findings per patient were observed; 19% of all patients had multiple (i. e., ≥2) calcific spots. The main additional pathologies were bursitis (87%), type II–III acromion (Bigliani classification, 70%), and synovitis (47%). No statistical significance was found for any associations tested between the localization of the deposit and the documented pathologies.
Conclusion
Patients with symptomatic, chronic calcific tendinitis of the shoulder may suffer from multiple and therapeutically relevant disorders of the glenohumeral joint requiring surgical care. The frequency of findings underlines the importance of a diagnostic and therapeutic arthroscopy of the shoulder in order to ensure that surgeons properly address intra-articular pathologies.
Zusammenfassung
Hintergrund
Mögliche Begleitbefunde der Tendinosis calcarea des Schultergelenkes sind bis dato nicht ausreichend geklärt. Die Hypothese der vorliegenden Studie lautet, dass zahlreiche Begleitbefunde bei einer Tendinosis calcarea vorliegen dürften, welche ebenfalls therapiebedürftig seien. Zielsetzung dieser Studie war die Dokumentation intraartikulärer pathologischer Veränderungen und die Untersuchung möglicher Korrelationen der Lage und Verteilung der Kalkdepots mit intraartikulären Veränderungen sowie Bewegungseinschränkungen.
Methoden
Aufgrund einer chronischen Tendinosis calcarea wurden 53 Patienten arthroskopisch therapiert. Die Dokumentation umfasste demographische Basisvariablen der Patienten, intraoperative Befunde aller Strukturen des Glenohumeralgelenks, passive Bewegungsumfänge, Instabilitätszeichen in Allgemeinnarkose sowie Grundinformationen zum intraoperativen Vorgehen.
Ergebnisse
Es wurden 189 pathologische Veränderungen entdeckt, 77 während der Arthroskopie. Chirurgisch therapiert wurden 74 % aller (extra- und intra-) bzw. 70 % der intraartikulären Befunde. Im Mittel wurden 3,6 zusätzliche pathologische Veränderungen pro Patient dokumentiert. Bei 19 % der Patienten bestanden mehrere (≥2) kalzifizierende Herde. Die häufigsten begleitenden Veränderungen waren Bursitis (87 %), ein Akromion vom Typ II–III (Bigliani-Klassifikation, 70 %) oder Synovialitis (47 %). Es wurde kein statistisch signifikanter Zusammenhang zwischen der Kalklokalisation und den dokumentierten Begleitbefunden festgestellt.
Schlussfolgerung
Patienten mit symptomatischer chronischer Tendinosis calcarea können multiple und therapeutisch relevante Begleitverletzungen aufweisen, welche eine chirurgische Therapie notwendig machen. Dies unterstreicht den Stellenwert der Arthroskopie bei diesem Krankheitsbild.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Past studies on surgery for calcific tendinitis of the shoulder considered extra-articular pathologies as secondary findings associated with the disease prompting surgery. Anatomic structures potentially affected by calcific tendinitis include the acromion, the acromioclavicular (AC) joint, the bursa, rotator cuff, synovia, capsule, long head of biceps tendon, and the chondral layer of the glenohumeral (GH) [19] joint.
Introduction
The reported incidence of calcific tendinitis of the shoulder ranges from 2.7 to 22.0% in routine clinical and radiographic examinations [25]. About 80% of calcified deposits are located in the supraspinatus tendon [16]. Although calcific tendinitis is a common finding, its causes, etiology, and pathogenesis remain unknown [12]. In 2007, Harvie et al. reported that 66 of 102 patients with calcific tendinitis of the GH joint suffered from thyroid dysfunction or disturbances in estrogen metabolism [10]. Apart from systemic diseases, repetitive overhead physical activity is widely regarded as a risk factor of tendon calcification, although this was refuted by Sansone et al. in a recent study of 199 female cashiers and 304 controls [23].
Although impingement or hooked acromia were widely presumed to be risk factors, they did not individually contribute to the risk of calcific tendinitis of the supraspinatus tendon in several studies [13, 14, 21]. Furthermore, the degree of pain and impairment of shoulder function were not related to the extent of the calcium deposits.
The vast majority of patients respond well to conservative treatment. According to the literature, less than 10% of patients need surgical treatment—mainly because of the severity of their symptoms and their request for treatment of the pain [8, 19].
We aimed to investigate whether the localization and spread of calcific tendinitis are associated with certain intra-articular pathologies and impaired range of motion (ROM) of the affected shoulder joint. We hypothesized that there are various additional pathologies accompanying calcific tendinitis, which might need further treatment during arthroscopy.
Patients and methods
Between October 2012 and May 2014, 53 patients undergoing arthroscopic removal of a calcium deposit of the shoulder joint were enrolled in a prospective observational case series.
Patients ≥18 years old presenting with a chronic, uni- or bilateral calcific tendinitis of the shoulder joint were enrolled. All patients were symptomatic for ≥6 months and did not respond to conservative treatment (i. e., nonsteroidal anti-inflammatory drugs, ultrasound, physiotherapy).
Exclusion criteria were: osteoarthritis of the shoulder, symptomatic GH instability, and previous operations or injuries of the shoulder joint (e. g., fractures of the humeral head, traumatic tears of the rotator cuff etc.).
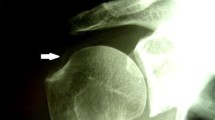
Classification
Radiographs of patients were acquired in three standardized views (anterior–posterior, axillary, and outlet view). The images showed radiological evidence of calcific tendinitis of the GH joint. All the deposits treated had been interpreted on x‑ray as homogeneous and clearly circumscribed in the sense of chronic calcification without signs of dissolution [7].
Documentation of the extra pathological findings included partial tearing of the supraspinatus tendon according to Habermeyer’s classification concerning the longitudinal spread (type 1–3) and sagittal spread (type A–C) [9]. Ellman’s classification was used to categorize partial thickness tears of the rotator cuff on the articular side [5]. Moreover, the extent of anomalies of the anchor of the long head of the biceps tendon was classified according to Snyder [24] (type I–VII) and the hooked shape of the acromion on the x‑ray according to Bigliani (type I–III) [3].
Surgical care
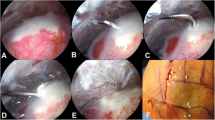
Surgery was performed by three equally experienced shoulder surgeons from the same institute. Patients were placed in the beach chair position. Arthroscopy commenced with a posterior standard portal, followed by lateral and/or anterior portals to address further pathologies. All aspects of the GH joint were investigated and documented in a standardized fashion, using intraoperative image and video recording. This included documentation of key surgical procedures. The calcific deposit was marked from the subacromial side with a needle. In order to remove the calcifications, the bursal side fascia was incised longitudinally and the calcification was scraped out completely. If necessary, the calcific deposit was identified on x‑ray. Intra-articular pathologies were treated according to clinical practice guidelines and established standards.
Data collection and processing
Data were recorded by surgeons on case report forms developed for this study. This documentation included pre-operative data (e. g., demographic baseline variables) as well as all intraoperative findings and procedures.
Statistical analysis
All statistical analyses were conducted in an explorative way. We recorded numbers, frequencies, means and mean differences (with standard deviations [SD]), as well as medians (with ranges or interquartile ranges [IQR]), as appropriate. Whenever possible, we calculated 95% confidence intervals (CI) as the preferred measures of uncertainty.
Exact univariate logistic regression was employed to investigate whether: (1) certain demographic or anatomic variables predict multiple calcifications, and (2) multiple calcifications predict the presence of intra-articular pathologies and the need for surgical intervention. Odds ratios (OR) were reported with 95% CI.
To analyze inter-subject differences regarding ROM parameters between the affected and contralateral shoulder, a multivariate analysis of variance was calculated. The Pillai–Spur criterion was used as test statistic.
SPSS 19.0 (IBM Company, N.Y.) and STATA 11.0 (StataCorp LP, Tex.) were used for all analyses.
Results
Data from 53 patients formed the basis of this study, which included 27 female and 26 male patients. The mean age was 54 years (38–73; SD: 8). The dominant shoulder was affected in 33 (63%) of all patients. Table 1 summarizes the baseline profile of the study sample.
The mean ROM of the affected and contralateral shoulder is documented in Table 2. The affected and contralateral shoulder showed statistically significant differences in ROM: F(3/50) = 4.81, p = 0.005 for the overall multivariate analysis. There was a statistically significant difference between both shoulders in external rotation (mean difference=8°, F(1/52) = 14.06, p < 0.001) and as well in flexion (F(1/52) = 9.38, p = 0.003) and abduction (F(1/52) = 4.25, p = 0.044). Only three patients presented a mild instability in the examination of the affected shoulder joint under anesthesia (6%), eight patients (15%) had a 1+ sulcus sign, and in four patients (8%) a 1+ anterior translation was documented but not further investigated in the statistical analysis.
Most calcific deposits were located in the supraspinatus tendon. Table 3 illustrates the prevalence of intraoperative findings. The size of deposits on the x‑ray was evaluated in 40 patients and ranged from 4 to 25 mm (mean: 9.3; SD: 4.7 mm).
A total of eight partial tears of the rotator cuff were documented; seven were situated in the supraspinatus and one in the subscapularis tendon. Three of these tears needed single-row repair (Ellman type II), whereas another five (Ellman type I) were treated with surgical debridement. After removal of calcifications, eight additional rotator cuff defects needed single-row repair because of larger rotator cuff defects close to the insertion zone and another one surgical debridement.
Apart from calcific tendinitis, arthroscopy revealed 189 additional pathologic findings in 53 shoulders, 77 of which were found inside the GH joint. Approximately three quarters of all findings (140/189, 74%; 95% CI: 67–80%) and 54 of 77 intra-articular findings (70%; 95% CI: 59–80%) required specific surgical care. Among 53 shoulders, 42 (79%; 95%: CI 66–89%) and 34 (64%; 95% CI: 50–77%) showed some or therapeutically relevant additional intra-articular pathology. Fig. 1 shows the number of side pathologies and treatments.
In all, 24 of 53 shoulders (45%; 95% CI: 32–60%) showed biceps tendon abnormalities, 15 needed surgical treatment, e. g., tenotomy and tenodesis, SLAP repair, or trimming. The prevalence of type 2 and 3 acromial variants was 36 of 53 cases (70%; 95% CI: 56–82%), 32 of which needed subacromial decompression.
Bursitis was present in 46 of 53 cases (87%; 95% CI: 75–95%), and all but one inflamed bursa were completely removed.
Synovitis was detected in 25 of 53 cases (47%; 95% CI: 33–61%), and treated by synovectomy in 18 patients (34%; 95% CI: 22–48%). Capsulitis was diagnosed in seven of 53 patients (13%; 95% CI: 5–25%). Five stiff shoulders were either treated by capsulotomy or mobilized under general anesthesia.
The AC joint showed degenerative changes on the radiographs and pain in the examination in three of 53 cases (6%; 95% CI: 1–16%), all of which required Acromioclavicular joint (AC joint) resection.
Finally, chondral lesions affected the humeral head in two cases and the glenoid in three cases, prompting microfracture in all five patients.
Because an intraoperative quantification of the deposits was not sufficiently possible, quantitative analysis was limited to the stratum of singular and multiple spots.
Gender did not contribute to the risk of multiple calcific lesions (OR = 0.95; 95% CI: 0.24–3.78). For patients aged >54 years (n = 25), involvement of the dominant arm and acromion types 2 and 3 were considered to increase the likelihood of multiple spots; however, this association was not statistically significant (OR dominant arm = 2.28 [95% CI: 0.19–27.93], OR age >54 = 3.24 [95% CI: 0.74–14.26]) (see Fig. 2).
Multiple deposits appeared to predict both synovitis and the need for synovectomy. The strongest, yet nonsignificant association, was observed between multiple calcifications and presence of capsulitis (OR: 4.18; 95% CI 0.76–22.86; p = 0.099).
Patients with multiple calcific deposits showed larger side differences in ROM, mainly in rotation (see Fig. 3). Again, these differences were not statistically significant.
Discussion
This study aimed to document intra-articular pathologies and investigate whether the location and spread of calcific tendinitis are associated with intra-articular pathologies and impairment in ROM. In this study, 189 additional pathologies were found, 77 during intra-articular arthroscopy. Of all extra- and intra-articular pathologies, 74 and 70%, respectively, required surgical treatment. A mean of 3.6 additional pathologic findings per patient were observed. Of all patients, 19% had multiple (i. e., ≥2) calcific spots. There was no statistical significance for any associations tested between the localization of the deposit and any of the documented pathologies.
Conservative and surgical care options for calcific tendinitis are of ongoing clinical debate and scientific interest [4, 16, 18, 22, 26, 27]. Arthroscopic removal of the calcium deposit is considered an effective treatment and shows good results after long-term follow-up [1, 2, 7, 20]. Despite this, the pathomechanisms behind calcific tendinitis remain unclear [12].
Multiple studies have been performed on associated side pathologies in patients suffering from calcific tendinitis. Loew et al. did not find a significant correlation between the shape of the acromion, subacromial impingement, and the presence of calcific tendinitis on radiographs and magnetic resonance images of 75 patients [14]. Prato et al. did not find a significant difference in the average acromion tilt angle between shoulders affected by calcific tendinitis and healthy shoulders on radiographs of 243 shoulders. The investigators concluded that calcium deposits are not related to shoulder impingement [21]. Kircher et al. reported no statistically significant correlation between pain, function, or Constant scores and deposit size or acromial index in patients with calcific tendinitis [13]. Furthermore, the compelling hypothesis that the calcific deposit leads to increased upward forces against the subacromial undersurface and thus causes pain and a deficit in ROM could not be confirmed.
In 2002, Maier et al. developed the idea that calcific tendinitis does not occur as a singular pathology of the shoulder joint. They evaluated outcomes after open surgery with extirpation of the calcium deposit in 36 shoulders [17]. All patients with accompanying pathologies of the shoulder joint had poor outcomes at the final follow-up. This study highlights the need for careful exploration of the shoulder joint during surgery for calcific tendinitis, and for reconstruction, repair, or debridement of all joint components in a single-stage fashion.
Altogether, the results of this study are in line with these previous investigations. Pathologic shapes of the acromion were detected in 68% of arthroscopies, and there was no clear correlation with the localization of a calcium deposit. Of note, the predicted absolute risk of multiple deposits was 13% with Bigliani type 1 and 22% with type 2/3 acromion morphology.
Bursitis was documented in 87% of all cases in this study, and 49% were classified as generalized or with formation of villi. This is in contrast to the findings of Ishii and coworkers, who noted inflammatory changes of the bursa in only six of 43 (14%) histological specimens from shoulders with calcific tendinitis [11]. Owing to the sample size and statistical issues (i. e., model saturation), we did not explore the association between bursitis and calcific deposits in more detail. For descriptive purposes only, exact logistic regression revealed odds ratios for the coincidence of multiple calcific deposits (OR = 2.5) and bursitis with the need for a bursectomy (OR = 2.1).
Regarding the side pathologies that needed surgical treatment, the causes of the preoperatively chronic and on-going pain need to be elucidated. Despite the chronic calcification, the additional pathologies could have caused at least some of the recorded symptoms, i. e., 23 of 53 patients had pathologies of the long head of the biceps tendon, which clinically often present with chronic anterior shoulder pain [15]. Since the indication to address the side pathologies was drawn independently from the calcific deposit and all the detected changes are known to cause pain and dysfunction of the shoulder joint as well, it seems unlikely that the calcific tendinitis alone can be held responsible for the noted symptoms. Furthermore, this study cannot explain whether removal of the calcification alone would have sufficiently decreased the symptoms or whether the surgical treatments of the side pathologies would lead to a satisfying outcome.
Nevertheless, the large number of accompanying inflammatory reactions (bursitis 87% [46/53], synovitis 47% [25/53], capsulitis 13% [7/53]) is in line with the statistically significant difference in ROM between the affected and contralateral shoulder (p = 0.005). The inflammatory reaction around the calcific tendinitis could lead to a capsular and intra-articular process resulting in synovitis and capsulitis, which leads to a painful impairment of the ROM [6].
It can be summarized that the large number of additional findings during the arthroscopies has confirmed the study hypothesis.
Limitations
The present study is a single-center case series with the expected methodological limitations pertinent to this kind of research. Data are naturally susceptible to indication, selection, and performance bias. Only perioperative data were recorded, and cannot provide any information about long-term follow-up. With regard to risk estimates, the major limitation is the lack of a control group (i. e., a healthy sample of patients with shoulder disorders other than calcific tendinitis). Three surgeons performed the surgical interventions; nevertheless, they all came from one surgical center with a comparable amount of expertise and the same standards of care that apply to this surgical center.
However, the carefully documented intraoperative findings described here provide further insights into the associations between multiple calcific spots in calcific tendinitis and accompanying intra-articular pathologies, and highlights the need for further detailed research on this issue. The results presented may be helpful for designing future studies and computing clinically and statistically meaningful sample sizes.
Conclusion
Patients with symptomatic, chronic calcific tendinitis of the shoulder resistant to conservative treatment may suffer from multiple disorders of the GH joint requiring surgical care. Although no statistically significant association between the side pathologies and the calcific deposits could be proven, the number of findings underlines the importance of a diagnostic and therapeutic arthroscopy of the GH joint in order to detect intra-articular pathologies that might need to be addressed by the surgeon.
References
Ark JW, Flock TJ, Flatow EL, Bigliani LU (1992) Arthroscopic treatment of calcific tendinitis of the shoulder. Arthroscopy 8(2):183–188
Balke M, Bielefeld R, Schmidt C, Dedy N, Liem D (2012) Calcifying tendinitis of the shoulder: midterm results after arthroscopic treatment. Am J Sports Med 40(3):657–661. https://doi.org/10.1177/0363546511430202
Bigliani LU, Ticker JB, Flatow EL, Soslowsky LJ, Mow VC (1991) The relationship of acromial architecture to rotator cuff disease. Clin Sports Med 10(4):823–838
Daecke W, Kusnierczak D, Loew M (2002) Extracorporeal shockwave therapy (ESWT) in tendinosis calcarea of the rotator cuff. Long-term results and efficacy. Orthopäde 31(7):645–651. https://doi.org/10.1007/s00132-002-0324-y
Ellman H (1990) Diagnosis and treatment of incomplete rotator cuff tears. Clin Orthop Relat Res 25(4):64–74
Fernandes MR (2013) Arthroscopic capsular release for refractory shoulder stiffness. Rev Assoc Med Bras 59(4):347–353. https://doi.org/10.1016/j.ramb.2013.02.004
Gartner J, Heyer A (1995) Calcific tendinitis of the shoulder. Orthopäde 24(3):284–302
Gschwend N, Patte D, Zippel J (1972) Therapy of calcific tendinitis of the shoulder. Arch Orthop Unfallchir 73(2):120–135
Habermeyer P, Krieter C, Tang KL, Lichtenberg S, Magosch P (2008) A new arthroscopic classification of articular-sided supraspinatus footprint lesions: a prospective comparison with Snyder’s and Ellman’s classification. J Shoulder Elbow Surg 17(6):909–913. https://doi.org/10.1016/j.jse.2008.06.007
Harvie P, Pollard TC, Carr AJ (2007) Calcific tendinitis: natural history and association with endocrine disorders. J Shoulder Elbow Surg 16(2):169–173. https://doi.org/10.1016/j.jse.2006.06.007
Ishii H, Brunet JA, Welsh RP, Uhthoff HK (1997) “Bursal reactions” in rotator cuff tearing, the impingement syndrome, and calcifying tendinitis. J Shoulder Elbow Surg 6(2):131–136
Kachewar SG, Kulkarni DS (2013) Calcific tendinitis of the rotator cuff: a review. J Clin Diagn Res 7(7):1482–1485. https://doi.org/10.7860/JCDR/2013/4473.3180
Kircher J, Morhard M, Patzer T, Magosch P, Lichtenberg S, Habermeyer P (2012) Do anatomic variants of the acromion shape in the frontal plane influence pain and function in calcifying tendinitis of the shoulder? Knee Surg Sports Traumatol Arthrosc 20(2):368–372. https://doi.org/10.1007/s00167-011-1563-4
Loew M, Sabo D, Wehrle M, Mau H (1996) Relationship between calcifying tendinitis and subacromial impingement: a prospective radiography and magnetic resonance imaging study. J Shoulder Elbow Surg 5(4):314–319
Lorbach O, Trennheuser C, Anagnostakos K (2014) Diagnostics and therapy of isolated proximal biceps lesions. Obere Extremität 9(1):10–16. https://doi.org/10.1007/s11678-013-0243-z
Louwerens JK, Sierevelt IN, van Noort A, van den Bekerom MP (2014) Evidence for minimally invasive therapies in the management of chronic calcific tendinopathy of the rotator cuff: a systematic review and meta-analysis. J Shoulder Elbow Surg 23(8):1240–1249. https://doi.org/10.1016/j.jse.2014.02.002
Maier M, Krauter T, Pellengahr C, Schulz CU, Trouillier H, Anetzberger H, Refior HJ (2002) Open surgical procedures in calcifying tendinitis of the shoulder—concomitant pathologies affect clinical outcome. Z Orthop Ihre Grenzgeb 140(6):656–661. https://doi.org/10.1055/s-2002-36033
Marder RA, Heiden EA, Kim S (2011) Calcific tendonitis of the shoulder: is subacromial decompression in combination with removal of the calcific deposit beneficial? J Shoulder Elbow Surg 20(6):955–960. https://doi.org/10.1016/j.jse.2010.10.038
McLaughlin HL (1963) The selection of calcium deposits for operation; the technique and results of operation. Surg Clin North Am 43:1501–1504
Oliva F, Via AG, Maffulli N (2011) Calcific tendinopathy of the rotator cuff tendons. Sports Med Arthrosc 19(3):237–243. https://doi.org/10.1097/JSA.0b013e318225bc5f
Prato N, Peloso D, Franconeri A, Tegaldo G, Ravera GB, Silvestri E, Derchi LE (1998) The anterior tilt of the acromion: radiographic evaluation and correlation with shoulder diseases. Eur Radiol 8(9):1639–1646. https://doi.org/10.1007/s003300050602
Rebuzzi E, Coletti N, Schiavetti S, Giusto F (2008) Arthroscopy surgery versus shock wave therapy for chronic calcifying tendinitis of the shoulder. J Orthop Traumatol 9(4):179–185. https://doi.org/10.1007/s10195-008-0024-4
Sansone VC, Meroni R, Boria P, Pisani S, Maiorano E (2014) Are occupational repetitive movements of the upper arm associated with rotator cuff calcific tendinopathies? Rheumatol Int. https://doi.org/10.1007/s00296-014-3086-z
Snyder SJ, Karzel RP, Del Pizzo W, Ferkel RD, Friedman MJ (1990) SLAP lesions of the shoulder. Arthroscopy 6(4):274–279
Uhthoff HK, Loehr JW (1997) Calcific tendinopathy of the rotator cuff: pathogenesis, diagnosis, and management. J Am Acad Orthop Surg 5(4):183–191
Vavken P, Holinka J, Rompe JD, Dorotka R (2009) Focused extracorporeal shock wave therapy in calcifying tendinitis of the shoulder: a meta-analysis. Sports Health 1(2):137–144. https://doi.org/10.1177/1941738108331197
Yoo JC, Park WH, Koh KH, Kim SM (2010) Arthroscopic treatment of chronic calcific tendinitis with complete removal and rotator cuff tendon repair. Knee Surg Sports Traumatol Arthrosc 18(12):1694–1699. https://doi.org/10.1007/s00167-010-1067-7
Acknowledgements
The authors thank Prof. Peter Habermeyer for performing some of the surgeries and for supporting the study. The authors thank Dr. Roland Ventura for scientific advice.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
S.M. Hünnebeck, D. Stengel, S. Lichtenberg, C. Güthoff, and M. Loew declare that they have no competing interests.
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975. Informed consent was obtained from all patients included in the study. Ethical committee approval was received by the ethical committee of the ATOS Clinic Heidelberg, no. 5/14.
Rights and permissions
About this article
Cite this article
Hünnebeck, S.M., Stengel, D., Lichtenberg, S. et al. Intra-articular findings in shoulder joints affected by calcific tendinitis. Obere Extremität 12, 242–247 (2017). https://doi.org/10.1007/s11678-017-0429-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11678-017-0429-x