Abstract
Detection of Alzheimer’s disease (AD) in an early stage is receiving increasing attention for a number of reasons, such as the failure of drug trials in more advanced disease stages, the demographic evolution, the financial impact of AD, and the approval of amyloid tracers for clinical use. Five focus group interviews with stakeholders (healthy elderly, informal caregivers, nursing staff, researchers, and clinicians) were conducted.. The verbatim transcripts were analysed via the Nvivo 11 software. Most stakeholder groups wanted to know their own amyloid PET scan result. However, differences occurred between FGs: two groups (informal caregivers and researchers) wanted to know, whilst in the three other groups (healthy elderly, nursing staff, and clinicians) FG members opted not to know or were still in doubt about their decision. Stakeholders provided insight into their reasons for wanting to know their amyloid PET scan result (e.g., the need for clarity, to inform relatives, to make arrangements), for not wanting to know their result, or why they were in doubt about their decision (e.g., fear of AD, not wanting to burden their social environment). Several advantages (e.g., to know what is going on with their health, to plan for the future) and disadvantages (e.g., absence of a disease modifying treatment, risks when undergoing tests) were mentioned as part of knowing their amyloid PET scan result. Certain considerations were clustered in a grey zone, in between advantage and disadvantage, such as the emotional consequences. Clinicians, researchers, and policymakers ought to be aware of the diversity of reasons for (not) wanting to know their result and how possible benefits and risks can be viewed differently. The current findings are of importance for future early diagnosis and disclosure of results in the research setting.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Today, many clinicians, researchers, pharmaceutical companies, and healthcare and dementia organizations emphasize the importance of detection of Alzheimer’s disease (AD) in an early pre-dementia or even preclinical phase. This idea has gained considerable momentum for several reasons: Novel treatment may have a better outcome when initiated in an early stage before irreversible brain damage has occurred due to AD. Given the failure of many recent trials in AD in a more advanced stage of dementia, clinical trials have started to target individuals earlier in the disease course at the stage of mild cognitive impairment (MCI) before the onset of dementia and before significant functional impairment (Petersen et al. 2001). Detection of Alzheimer in these early stages has only become possible thanks to the development of biomarkers. These are biological indicators that can gauge the presence of a disease and can be used to detect abnormalities at an earlier, pre-dementia or even at a preclinical stage (Grill, Johnson, and Burns 2013). One of the biomarkers used to support a diagnosis of AD is brain amyloid, which can be visualized by positron emission tomography (PET) (Witte et al. 2015). Besides being potentially useful for clinical practice, PET imaging of beta-amyloid plaques is also being used in brain research on AD (Witte et al. 2015; Vandenberghe, Adamczuk, and Van Laere 2013b; Vandenberghe et al., 2013a). Research to validate biomarkers for clinical use and to develop new AD biomarkers is ongoing (Herholz and Ebmeier 2011). The Food and Drug Administration (FDA) and the European Medicine Agency (EMA) have approved three amyloid radiotracers that have high affinity for binding to beta-amyloid plaques (flutemetamol, florbetapir, and florbetaben labelled with (18)F for PET imaging) for diagnostic purposes in cognitively impaired patients who are being evaluated for AD (Johnson, et al. 2013). In a research setting, the FDA and EMA approval along with the Appropriate Use Criteria for Amyloid PET have been put forward as arguments pro-disclosure in the debate whether or not to return individual research results (IRR) to the study or research participant (Lerner 2013; Johnson, et al. 2013). To date, the degree to which IRRs are disclosed varies depending on the trial, as there is no legal obligation for the researcher to return IRRs (Roberts, Dunn, and Rabinovici 2013; Lingler and Klunk 2013).
These and other elements have been put forward in favour of an early detection of AD and hence early disclosure of an AD diagnosis, yet several ethical questions emerge: What are the ethical benefits and risks of an early disclosure? Would people want to know an early diagnosis or an IRR as part of a clinical trial when current treatment options are still limited? Whether and how should the researcher disclose the IRR? Is the road of early disclosure the road clinicians and researchers want to take?
To our knowledge, only a few qualitative studies have been conducted in the past, such as interviews with patients and/or their carers on the topic of amyloid PET disclosure (Lawrence et al. 2014; Grill et al. 2017). With regard to published focus group interviews, these were often limited to a specific topic, such as the diagnostic disclosure of dementia and the emotional impact of dementia diagnosis. Hence, they were mostly conducted from one or two perspectives, such as the views from patients, carers, or general practitioners (GPs) (Lawrence et al. 2014; Connell et al. 2004; Cahill et al. 2008; van Hout et al. 2000; De Lepeleire et al. 2008).
However, little is known about stakeholders’ (patients, relatives, informal caregivers, clinicians, researchers, patient and dementia organizations, and healthy elderly who are often perceived as an at-risk group for getting AD) views and experiences on the following topics: How early would individuals seek a medical consultation from a general practitioner or at the memory clinic? What would attract or withhold individuals from seeking medical advice? What are the motivations to enrol in a clinical trial? Why would stakeholders opt for the disclosure of their amyloid PET scan result, and what do they perceive as risks/benefits from this disclosure? The views of these stakeholders are vital, as all these groups are either involved in or concerned about the ethical issues in the above-mentioned topics. Exploring the views, experiences, and concerns of stakeholders will allow us to enhance early diagnostic disclosure, trial recruitment, and participant follow-up, as these items will be based on the expectations, needs, and concerns of these stakeholders.
Therefore, we sought to explore these issues from multiple perspectives by conducting focus group interviews with several stakeholders.
Methodology
Recruitment
After ethical clearance from the Social and Societal Ethics Committee of the University of Leuven (SMEC, Belgium, study number G-2015 05 250) focus group (FG) interviews with stakeholders were conducted between December 2015 and February 2017. Recruitment was done through one contact person belonging to the stakeholder group. This methodology was best suited, as people volunteered within a group that consisted of the same characteristics, and via the network of the contact person, most people within the group knew each other before the interview took place. This created an open atmosphere for discussing and reflecting on the topic. We aimed for five to ten participants per FG (Mortelmans 2007). Via the contact person, an invitation letter and information brochure were handed over or emailed to the participants before the FG interview took place.
Before the start of the FG interview, the interviewer (GV) provided each participant with a printed information brochure and orally explained the procedure of the FG, participants’ rights, the fact that the FG would be recorded, and that subsequent data would be used for scientific publications. Participants were assured that all personal data would remain confidential. Participants were then invited to sign the informed consent form (IC) and to complete the socio-demographic form. In addition, participants could fill in their contact details on the IC if they wished to be informed about the general results after the completion of the study.
An hour and a half was allotted to each FG. A moderator and observer were always present. A location and time were chosen that best suited the participants. After completion of the FG interview, participants received a small token (box of chocolates) for their willingness to collaborate in this study.
Data Collection and Analysis
Focus groups were used to explore participants’ views and experiences and to provide insight into the topic addressed (Kitzinger 1995). A semi-structured format for the FGs was favoured by using the same scenarios for each FG. The scenarios used (see Supplementary material) were designed by the authors (GV, KD, and RV) and were based upon ethical issues addressed in the available literature published on this topic. The scenarios were presented to the SMEC ethics commission as part of applying for ethical clearance.
Analysis of the data was done in two steps:
-
(1)
The data from the socio-demographic forms is presented in table 1. In appendices 1 to 3 in the Supplementary material, we present additional data collected throughout the FG interviews. Appendix 1 in the Supplementary material represents the chosen positions (wife, husband, and general practitioner as part of scenario 1) as chosen by the FG members. Appendices 2 and 3 in the Supplementary material represent the rationale for wanting to know or not to know the IRR (scenario 2, exercise A) and the clustered advantages and disadvantages of knowing the IRR (scenario 2, exercise B) as written down by the participants. For scenario 3, no additional tools, with the exception of the scenario, were used. Hence, no additional data is available in the Supplementary material regarding scenario 3.
-
(2)
Content analysis was used for the verbatim transcripts and by using the qualitative software of NVIVO 11 (Mortelmans 2007; Bazeley 2007; Hsieh and Shannon 2005). This was done in four phases: (a) An initial coding by GV of all FG transcripts separately; (b) Two to three weeks after the initial coding process, all FG transcripts were separately coded a second time; (c) The codes from the second coding process were then compared with the codes from the initial coding process; (d) Lastly, all codes were double-checked by another researcher (KD) to avoid misinterpretation.
All of the FG interviews were conducted in Dutch. Citations used in this article were translated into English. To protect privacy, names are replaced by X or Y in the quotes.
Results
-
1.
Demographics of the Study Population and Structure of the Results
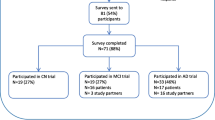
In total, forty individuals participated in five FGs, conducted between December 2015 and February 2017. The demographics and recruitment strategy of each focus group are listed in table 1.
We have structured the results section of this article based on the topics as discussed in our FGs. This format is well suited as it provides a clear representation of the FG discussions. Table 2 presents an overview of the structure of the results sections and where to find additional information in the Supplementary material.
In each presented topic in our results section, we cover the general findings where all FG groups agreed. Where possible we refer to the FG differences at the end of the presented results section.
-
2.
To Seek Medical Advice After Recognition or Experience of Memory Complaints
In the first presented case (box 1), we explored how participants thought about seeking medical advice after recognizing or experiencing their first memory complaints, which attitude or position they would adhere to (the position of the wife, husband, or general practitioner (GP)) in the presented case and which difficulties may emerge throughout that process. The summary of the elements discussed under this case are presented in appendix 1 in the Supplementary material.
Box 1 Description of presented scenario 1 and opening question
Scenario 1: A man of sixty-three starts to experience his first memory complaints, yet minimizes these problems: “Everyone forgets something and especially at this age.” His wife is more concerned and pushes her husband to seek medical advice from the general practitioner (GP). The GP thinks the problem is stress due to an overload of work and advises the man to come back in three months if the situation has not changed. The wife is still concerned and wants her husband to go for further testing to a memory clinic, yet the man is in doubt: “Do I already want to know if there is something wrong with me? I am sixty-three and still working.” Which of the three positions (wife, husband, GP) would you take? |
2.1 The Right (not) to Know of the Patient Versus Family Pressure and Burden
Most participants opted for the position of the wife to seek medical advice and to know what is going on. The pushy attitude of the wife was also perceived by most FG participants as a good attitude; “He starts to doubt under the pressure of his wife. Thank God, maybe, that possibly facilitated his diagnosis” (Clinician, man). For other participants the attitude of the wife can only lead to increased levels of uncertainty and stress with the patient, as it is his decision to know or not to know what is going on: “[…] That would be my biggest concern. What quality of life will I give to him when suggesting him to seek medical advice? To make him doubt? That would be important for me” (Nursing staff, woman).
Some participants mentioned that it is understandable that some patients opt not to know and prefer to remain in ignorance as there is currently no disease modifying treatment available or due to anxiety about AD.
The focus group of informal caregivers and nursing staff also pointed to the impact of a patient’s decision to know or not to know, as both decisions have implications for the partner. On the one hand, not knowing can be difficult for the partner who often notices these changes first and who often stimulates the patient to seek medical advice. On the other hand, knowing the news affects both patient and family members:
So I personally think that if you get the diagnosis, and I have told that to the professor X [Caregiver referred to the consulted neurologist who is also professor] last time, then I actually think they should also inform the partner that their life completely changes, because the person himself does not know it. For Y it is normal way of life, but in one year’s time my life has enormously changed. Not just in that one year since we know [ The diagnosis of husband], but from that moment onwards it has really changed. (Carer, woman)
2.2 GP’s Role
Most FG members found that the GP in the presented scenario should have taken the memory complaints more serious, should have provided more information about possible next steps, and should have referred the patient to the memory clinic for further testing. However, two nuances were reported. Firstly, a few individuals (addressed in the FG of the researchers, healthcare staff, and healthy elderly) stated that the advice of the GP to give it a few more months to see how the memory complaints evolve was a good approach, as the GP was not causing immediate stress and concern towards the patient. Secondly, the group of healthy elderly reported that there is no fault in the GP’s decision to wait and see, as there is no cure available for AD.
Furthermore, FGs reflected on the difficulties for GPs in recognizing these symptoms of cognitive decline. An element mentioned in all FGs was the GPs’ perceived lack of experience with AD and dementia patients as it was thought that they often only have a few of these cases per year. Certain FGs addressed difficulties for the GP in recognizing these symptoms of cognitive decline. For example, informal caregivers stated that via their own concrete experiences, some patients deny or hide their symptoms and act in a socially desirable way in front of their GP, family members, and friends. As they described it:
It is a very lonely period because Y succeeded in behaving in a desirable way in social situations toward friends, with the GP, with professor X. Every time again and again […]. (Carer, woman)
The FG of clinicians reported on another difficulty for the GPs, whereby they are often not aware about new diagnostic possibilities to detect the disease and that GPs often become “selectively blind” as they follow up and know some patients for a long period of time;
Participant 1: Of course, and that is also another problem, that is that they become selectively blind due to the fact they follow their patient for a long time. You become part of the furniture of their house; well, this is something GPs also admit, that sometimes a fresh look at the case can give a few new insights.
Participant 2: Indeed, but if the GP knows the family well and knows the reliability of the wife of the patient who notices something and reports this […].
Participant 3: […] That is because we already receive a referred to and selective population. I think that it is not easy for a GP to refer everybody just like that. They see many people with vague complaints that may possibly be cognitive.
Participant 1: What you are saying is that the GP could also dig a bit deeper. He could take a mini mental state, could also perform a blood test.
Participant 3: Yes, the simple things that don’t demand too much time.
(Dialogue between three clinicians, all men)
Clinicians and researchers referred to the importance of a more in-depth consultation by conducting a few simple tests, such as the Mini-Mental State Examination (MMSE) and the necessity of patient referral to the memory clinic. Yet, clinicians admitted that it is not always easy to refer a patient to the memory clinic, especially when cognitive symptoms are not being detected.
-
3.
Reasons to Know or not to Know the Amyloid PET Scan Result
The second case (box 2) presented the possibility of enrolling in a clinical trial and the option of being informed of the amyloid PET scan result.
Box 2 Description of presented scenario 2
Scenario 2: A woman of sixty-eight has received a diagnosis of MCI at the Memory Clinic and was provided with the option to participate in a clinical trial, where she can opt for the disclosure of her amyloid PET scan result. This amyloid PET scan result could reveal to the participant that her MCI is due to AD. She is doubting whether or not to know the result as, according to her, there are several advantages and disadvantages when knowing this result. |
In appendix 2 in the Supplementary material we present the chosen positions (to know, not to know or in doubt) and the provided rationale to support their decision as written down by our FG participants as part of the first exercise of scenario 2.
In the group of the informal caregivers and the researchers, there was a strong tendency toward opting for their amyloid PET scan result. In the group of healthy elderly, nursing staff and clinicians, a mix between the participants was noticed as some opted to know and others preferred not to know or were still in doubt about their decision.
3.1 Rationale in Favour of Opting for Amyloid PET Disclosure
The following three reasons were mentioned the most amongst all FGs:
-
(1)
The need for clarity about their health condition. Participants wrote down sentences such as: “I know what is going on,” “To know if there is a risk of getting AD,” “Desire for clarity and not to remain in doubt.”
-
(2)
To inform partner, children, and other family members about the result. Informing family members implies that they can understand the patient’s situation and anticipate future cognitive decline and character or personality changes.
-
(3)
To make arrangements for the future while the person is still capable of doing so. Arrangements about finances, quality of social relationships, advance directives, and end-of-life decisions were discussed. In particular, euthanasia was mentioned by many participants amongst the different FGs as part of arranging their future. Addressed by members within the groups of informal caregivers, healthcare staff, and clinicians was the difference between thinking of euthanasia and the actual implementation of euthanasia. For example, a clinician described it in the following way:
I would be tempted to say, or I can imagine, that I would choose for euthanasia in such circumstances. But on the other hand, I have already seen many people firmly deciding that if they would get Alzheimer’s during their life, they would want euthanasia, but the moment they become ill, they change their mind. So I don’t dare to stick my hand in the fire that I would choose for euthanasia in this situation, but it is a possibility that I would keep open for myself, I think […] (Clinician, man)
Another reason that was often simultaneously given with the rationale of planning for the future was to enjoy life more by creating a bucket list or by doing the things now, such as travelling, while the patient is still capable of doing so.
A stakeholder difference in the rationale of knowing their IRR was noticed. To enrol and participate in clinical trials was brought up by the group of researchers and clinicians yet was not expressed by the other FGs.
3.2 Rationale for not Wanting to Know the Amyloid PET Scan Result or for Doubting What to Decide
Two common reasons were mentioned amongst the FG members who wished not to know or who were still in doubt about their decision for the situation as presented in scenario 2 (Box 2). These were: (1) Fear or anxiety for AD. Participants used words such as: “Fear for what can happen. I would become anxious.” (2) The fact that currently no disease modifying medication is available for AD provided many FG members with an argument to doubt whether they would want to know or to opt for not knowing the result: “Yes, if they can provide effective help or cure. No, if they cannot provide effective help or cure, I don’t want to know” (Healthy elderly, woman).
A stakeholder difference regarding the rationale for not knowing the IRR was noticed. The burden of medical investigation and risks when undergoing tests were mentioned by healthy elderly and nursing staff as a reason for not opting for the result yet did not occur among the other groups. In the group of researchers, one researcher expressed the opinion that PET scans are not invasive, so there is no burden regarding this type of test.
-
4.
Advantages and Disadvantages of Knowing the Amyloid PET Scan Result
The second exercise as part of the second scenario (Box 2) aimed to explore how FG members classify possible advantages and disadvantages of knowing their result, which is different from exploring their motivation and rationale to know or not to know the result.
In more concrete terms, FG members were provided with an envelope that contained several small sheets of paper with advantages and disadvantages written on them. The sheets addressed the following aspects: no cure for AD, emotional/psychological consequences, no absolute certainty with the result, more clarity/to know what is going on with health, to plan for the future, to inform others, to start early treatment/intervention, to enjoy life more, to change lifestyle, risks when undergoing tests. Participants also had the possibility to write down any other possible advantages and disadvantages they were thinking of.
This resulted into the schedule as presented in appendix 3 in the Supplementary material, where the advantages and disadvantages of knowing their IRR were categorized per group and according to the frequency of how many participants within the group used an advantage/disadvantage/grey zone in their schedule.
The most common perceived advantages in all FGs were to know what is going on with their health, to plan for the future, to change their lifestyle, and to enjoy life more. Another frequently mentioned advantage was to inform others about the received result.
The most common perceived disadvantages between all FGs were the absence of a disease modifying treatment for AD and the risks of undergoing tests. A few participants in the FG group of healthy elderly added additional elements to the risks associated with tests. These were the fear of undergoing the tests, the burden of going to the hospital, and the burdensome process of undergoing many tests before receiving a diagnosis. The lack of absolute certainty about the test result was also mentioned under the category of disadvantage.
The previous two paragraphs discussed the most common clustered elements under the category of advantage or disadvantage. However, a minority of FG members classified a topic which was mostly classified under “advantage” as a disadvantage, which indicates that for a minority of FG members, this specific topic was perceived in a different way compared to the majority of FG members. For example, to inform others was mentioned above as an advantage. However, informing others was also categorized by a minority of FG members under the category of disadvantage. On the one hand, informing others can be beneficial to receive practical support and also to receive emotional support and understanding for the patients’ and informal caregivers’ situation. Some informal caregivers reported the difficulties of a patient’s decision not to inform others, as they cannot talk about the emotional difficulties and burden they are experiencing. On the other hand, the question was raised whether people will still treat the patient in the same way once they know the result.
On the other hand, some of the elements classified as a “disadvantage” were clustered by a minority of FG participants as an advantage. For example, the absence of absolute certainty about the test result was mostly clustered under the category of disadvantage. However, a few participants from the four FGs (healthy elderly, informal caregivers, nursing staff, and researchers) described this as an advantage. They elaborated that a high/low chance or risk perception is also meaningful information that provides more clarity about their health situation. Some participants stated that it is important that the result is disclosed as it is, which means that also the risk perception and the lack of certainty in the result needs to be addressed. The FG of nursing staff and researchers discussed which percentage of risk they would like to receive themselves. These two FGs stated that it was not easy to attribute a number to the meaningfulness of a risk percentage, yet both groups agreed that the risk percentage should be at least fifty per cent to have some valuable information concerning one’s health.
Another example is the emotional and psychological consequences after receiving the result which was mostly mentioned under the category of disadvantage. Again, a few participants described it as an advantage. These participants described that not knowing the result and remaining in doubt would be emotionally and psychologically burdensome too. Although it was mentioned that receiving bad news can be emotionally difficult at first, knowing the result provides these participants with the opportunity to cope and move on with life.
Also, some FG members classified elements in a “grey zone.” This grey zone indicates that a topic could have both advantageous and disadvantageous aspects depending on the situation. The grey zone was only used by a few FG members of the informal caregivers and the nursing staff. All other groups clustered the elements under either advantage or disadvantage. Aspects mentioned in the grey zone were, for example, to inform others, to enjoy life more, and psychological and emotional consequences.
-
5.
Post Disclosure of the Result
The third presented scenario (box 3) aimed at exploring how participants would respond to possible difficulties after the disclosure of the result.
Box 3 Description of the presented scenario 3 and opening question
Scenario 3: A man of seventy-six with MCI participated two years ago in a clinical trial where he opted to be informed about his amyloid PET scan result. He received a positive amyloid PET scan result. After two years his memory complaints are still stable and did not become worse. After the disclosure of the result, his wife over-reacted, taking over his household tasks and not allowing him to drive the car. In addition, his neighbours started to look at him as if he already had AD. He regrets his decision of opting for the disclosure of the result two years ago. In his opinion, not knowing the result would have resulted in fewer consequences. What do you think of the man’s decision based on the consequences he experienced? |
5.1 Need for Adequate Information and Follow-Up After Disclosure
If clinical trials and research settings provide participants with the option of IRR disclosure, a consensus of all FG members was that research participants should know beforehand what the implications of IRR can be and what the possible consequences can be after the disclosure. Especially, they agreed that the risk perception and the limited predictive value should be explained to the research participant.
The FG group of researchers and clinicians added two nuances. Firstly, researchers and clinicians referred to the difficulty of estimating, in advance, the psychological strength and coping capabilities of participants to deal with this information.
Secondly, they reported that it is often difficult to explain this limited predictive value to the research participant. Even when the limited predictive value is well explained, it is likely that participants misinterpret these findings or regret their decision to be informed:
Participant 1, man: That is very difficult.
Participant 2, man: You cannot give a clear message.
Participant 1, man: You can give the message of the risk exactly, but you cannot determine what the perception of the individual is.
Participant 3, woman: That is another problem.
Participant 2, man: Also, you cannot say what the likelihood is.
Participant 1, man: Imagine that you could do that, even then? What does that mean?
Participant 3, woman: The period. Seventy percent within ten year or within twenty years? (Dialogue between three researchers)
Besides the need for adequate information, all FG members reported the need of more communication, support, and follow-up. This should not be limited to clinical trials; it is also of importance in the clinical setting when disclosing a clinical diagnosis to the patient. Psychosocial support should in their opinion not be restricted to the patient but should also include support for partners and informal caregivers. Support and counselling is important to explain to the participant/patient and their relatives how to interpret this result and the possibilities of cognitive rehabilitation and to stimulate the capabilities the patient can still do well. This was considered to be a task of both researchers and GPs.
5.2 Who to Inform and What to Say About the Result
Focus group members discussed two concrete consequences that may occur after informing others, more specifically stigmatization and patronization, whereby family members, for example, take over practical tasks:
(A) Patronizing: Most participants reflected that they would not like to be patronized themselves. However, some informal caregivers reported that it is a very recognizable situation to take over from the patient. Informal caregivers clarified that it is often well intentioned, but that for the patient this patronizing attitude may be counterproductive. Some FG members said it is also up to the patients themselves to clearly communicate about the things they still can do well. This is especially important for people at an early and often (very) mild stage of the disease.
(B) Stigmatization: The FGs of informal caregivers and nursing staff provided several experienced situations with stigmatization and reported that it is not always easy to inform others as people either have a negative perception about AD or do not know how to respond to the news. The need was raised to inform society more about what AD is and to make AD discussable.
So, from the moment onward that we disclosed, X got immediately labelled, and that is really a stigma. People look at him like, “He is about to do something whereby I will see that he has got Alzheimer’s,” while there are moments that there is nothing going on with him. […]. And what Y also said, that evasive behaviour where people address me while he is standing next to me. I always have to say: “Ask him. He is standing there, so ask him. It doesn’t mean that he cannot do anything.” So, you have to constantly educate people […]. (Carer, woman)
Based on these two consequences, FGs discussed the importance of first communicating with partners and family about who to inform and what to tell. Especially in the case of receiving a positive amyloid PET scan result, the FG of researchers and clinicians referred to the importance of others being aware that this result does not imply that the patient already has AD.
Discussion
This focus group study aimed, as the first of its kind, at exploring multiple stakeholders’ views on early diagnosis, clinical trial participation, and disclosure of amyloid PET scan results. The strength of this study is that several perspectives, from informal caregivers to clinicians, were explored. This enables us to get in-depth insight into the views from one specific group and to compare stakeholder groups. Here, we will raise additional ethical insights and comments relating to the following findings:
(1) Difficulty of Recognizing First Symptoms of AD
Many participants in our FG study referred to the difficulties of recognizing first symptoms of AD by their GP. Firstly, it became clear throughout the FD discussions that there is no consensus on what a first symptom for AD might be. While for some, forgetting groceries would be a first sign, for others this was not the case. Actual triggers for seeking medical advice were the urgency and the feeling of worry of the participants.
Secondly, throughout the FG discussions, especially with the informal caregivers, it became clear that many patients act in a socially desirable way, or in denial, and try to hide their memory complaints. The combination of the lack of clarity of a first symptom and the denial or socially desirable attitude can make it more difficult for the GP to interpret the complaints as early signs or triggers for AD.
Our findings confirm the surveys that have reported on the difficulties for GPs in diagnosing AD, whereby recognizing symptoms was mentioned as one of these struggles (Cahill et al. 2008; van Hout et al. 2000; Turner et al. 2004). Although these difficulties were reported in general AD literature, they are possibly of increasing interest when moving toward earlier diagnosis. For example, GPs might overlook the first symptoms of MCI and misinterpret these symptoms as signs of burn-out or stress (Cahill et al. 2008). Research also describes how it can take up to two years between the first consultation and the disclosure of the diagnosis (Cahill et al. 2008; Antoine and Pasquier 2013). This can be problematic as in many cases the GP is the first clinician to be contacted by the patient or even the only clinician involved in making the diagnosis (van Hout et al. 2000).
(2) To Know or not to Know
In the FG of informal caregivers and researchers, all members opted for knowing their result, whilst in three other groups (healthy elderly, nursing staff, and clinicians) there was a mix between the members who wanted to know, did not want to know, or were still in doubt. The findings from this FG study provide a more nuanced answer to the recently published studies that reported high numbers of respondents expressing the desire to know their genetic risk result for AD (Roberts et al. 2005; Green et al. 2009; Neumann et al. 2001). For example, all of the MCI participants who enrolled in a longitudinal observation amyloid PET study opted for disclosure of their amyloid PET scan result, but it remains unclear to which degree this can be generalized to a wider population (Vanderschaeghe, Schaeverbeke, Vandenberghe, and Dierickx 2017b).
Only limited research has been performed to explore the views of individuals who prefer not to know their result. The current study can provide insight into the rationale of the people who would prefer not to know or who are in doubt about their decision. Reasons for not wanting to know or for doubting were: fear and anxiety for AD once the result is known; feeling worried, stressed, or depressed; not wanting to burden the close social environment, and the lack of a treatment for AD.
(3) Early or Timely Diagnosis?
In the current study, most FG members reflected on the topic of “early diagnosis.” Only one FG member, a clinician, explicitly referred to the concept of “timely diagnosis” and favoured this concept above an “early diagnosis.” Timely diagnosis seems to be a clinically highly relevant concept in AD diagnostics that raises a number of questions: how does a timely differ from an early diagnosis and how do we define an early diagnosis? For some, MCI and MCI due to AD is already an early pre-dementia diagnosis. For others, early refers to asymptomatic preclinical AD. Dubois et al. (2016, 35) define a timely diagnosis as: “a diagnosis at the stage when patients come to the attention of clinicians because of concerns of changes in cognition, behavior or functioning and can be still free of dementia and functionally independent.” According to this definition, a timely diagnosis is made at the right time for the individual patient, irrespective of the disease stage, and is therefore not expressed in chronological terms (Dhedhi, Swinglehurst, and Russell 2014; Dubois et al. 2016; Robinson, Tang, and Taylor 2015). This means that a timely diagnosis does not exclude an early diagnosis. An early and timely diagnosis both occur after exploring the patient’s wish about testing for and knowing the result. However, a timely diagnosis gives the impression of respecting the decision-making process of the patient more compared to a society and industry moving towards earlier diagnosis and eventually resulting in “overdiagnosis” and screening for a disease in healthy individuals.
Furthermore, a study by Dhedhi Swinglehurst, and Russell (2014) reported the following two findings: (a) GPs favoured timely above early diagnosis. (b) The failure of making a diagnosis does not point to GPs’ lack of awareness or training skills. According to them, the policy focus on education and training to improve the awareness of GPs toward the benefits of early diagnosis may be misguided. They argue that it would be better to focus on supporting GPs in managing the complexity and uncertainty of the disease and in helping GPs with the dilemmas about providing family support after the diagnosis. However, in our FG study, participants often expressed the opinion that there was a lack of training and experience amongst GPs. In addition, the focus group of informal caregivers, nursing staff, and clinicians mentioned the long duration of the diagnostic process. Most of these FG members used an earlier diagnosis as a term, with only one clinician who explicitly favoured the term “timely diagnosis.” This highlights that although the concept of a timely diagnosis is beneficial and respects the decision-making of patients, for other groups, and especially mentioned in the FG of informal caregivers, an early diagnosis was perceived as important and training and education for GPs was recommended to enhance and facilitate the diagnostic process. In this way, the current study, with multiple stakeholders, provides additional insight to the views of GPs as described in the study by Dhedhi, Swinglehurst, and Russell (2014).
-
(1)
Impact of the News on Both Patient and Relatives
Our FG with informal caregivers showed how the decision to know or not to know affects both patients and their relatives. Informal caregivers also argued that the GP needs to inform the partner that his/her life will change after the disclosure of the news to the patient. This finding is in line with previous reported literature that addressed the burden of a diagnosis on the patient and his family members, and in particular the carer (Frank et al. 2006; Betts Adams 2006; De Vugt and Verhey 2013; Connell, Janevic, and Gallant 2001).
Based on respect for patients’ rights, it is a standard procedure in many countries that only the patient first is informed of the results. If the patient agrees, as a second step, relatives may be informed of this news. This view focuses on the perspective of the patient, whereby it is up to the patient himself to decide whether to undergo testing and whether to be informed of this result. This view ignores the difficulties and impact of the patients’ decision on their relatives. However, it is important that patients can take this decision voluntarily, without being pushed or pressured by relatives who wish to know what is going on with their family member.
-
(2)
Advantages and Disadvantages of IRR Disclosure
Our FG study reported on several advantages (e.g. to plan for the future, to inform others) and disadvantages (e.g. absence of a disease modifying treatment) of knowing an IRR. These findings are in line with previously reported studies. For example, the REVEAL study reported via a survey the views from asymptomatic adults on the disclosure of their genetic APOE status (Roberts et al. 2005). The interview study from Grill et al. (2017) focused on both patient and carer views on amyloid imaging, whilst the interview study by Vanderschaeghe and colleagues explicitly focused on the views from aMCI patients (Vanderschaeghe, Schaeverbeke, Vandenberghe, and Dierickx 2017b; Vanderschaeghe, Schaeverbeke, Bruffaerts, et al. 2017a).
However, our study differs from the previously mentioned studies, as multiple stakeholders’ views were explored on this topic using the same scenarios. Also, our FG study indicates how certain advantages and disadvantages were put in “the grey zone” by some FG members. This reveals how individuals can interpret and perceive these elements in different ways depending on, for example, personal views, values, and coping strategy. A concrete example was the emotional and psychological consequences of knowing the result, which is often described in the literature as an ethical challenge and as a disadvantage of knowing an early diagnosis or IRR. Here, the emotional implications were clustered under both advantage and disadvantage and has been put forward by some FG members as a topic in the grey zone. This finding highlights that researchers need to explain all possible risks/benefits as they are and let the participant decide whether these elements are perceived by their own personal views and values as benefits/risks or elements in the grey zone.
-
(3)
Different Interpretation on the Notion of “Risk” Depending on Stakeholders’ Viewpoint
Our FG study with several stakeholders revealed how a given FG can assign their own important nuances to a discussed topic. For example, the burden of going to the hospital, the fear for undergoing medical tests, and the burdensome process of undergoing multiple medical examinations and tests before receiving a diagnosis provided another interpretation to the word “risk” mentioned specifically and only by the group of healthy elderly. This result is also in line with a previous study, which concluded that risks as perceived by researchers can be viewed differently from the patient’s perspective (Vanderschaeghe, Schaeverbeke, Vandenberghe, and Dierickx 2017b). Additionally, the FG finding refers to the importance of clearly explaining to the patient, prior to the testing, which tests and how many tests are needed to establish a diagnosis.
-
(4)
No Absolute Certainty and the Unpredictability of the Disease Progression
The absence of absolute certainty about the received result was mentioned in our FG study under the category of disadvantage. However, as described in the results, some FG members pointed out that a high/low chance or risk is also meaningful information about their health. Two FG groups, nursing staff and researchers, discussed the topic of which percentage of risk would be meaningful to them. Both groups indicated that any test percentage above fifty percent contains valuable information. This was lower than the value that we had expected a priori, as the lack of absolute certainty and the limited predictive value of an AD diagnosis is often mentioned as an ethical concern in the literature (Antoine and Pasquier 2013; Prvulovic and Hampel 2011; Porteri et al. 2010; Porteri and Frisoni 2014; Chiu and Brodaty 2013; Werner and Korczyn 2008). However, the fifty percent mentioned by the two FG groups might indicate that adequate information about the limited predictive value and the risk perception is perhaps more important than the exact percentage of risk.
The risk estimation and the unpredictability of the progression was at first only mentioned by a few FG members in our study as a reason to doubt or opt for not knowing the result. Only when FG members were asked to categorize predefined elements as either a perceived advantage or as a disadvantage, this element was mentioned more as a concern. This reveals that, at first, many individuals are not aware of these issues. Again, this shows the importance of informing individuals about the risk estimation and about the unpredictability of possible disease progression prior to any testing.
-
(5)
The “Then Self” and the “Now Self” in the Quest for Euthanasia
In the FG groups of informal caregivers, nursing staff, and clinicians, the request for euthanasia was mentioned under the category of making arrangements for the future. However, it was nuanced in that there is a difference between “thinking of” and “the actual implementation.”
In the literature on advance directives and end-of-life decisions, there are similar reflections available. In particular the difference between the “then self” and the “now self” (Vollmann 2001; Gastmans and Denier 2010; Levi and Green 2010; Widdershoven and Berghmans 2001; Draper et al. 2010). The then self refers to the person making the necessary arrangements prior to the onset of dementia. The now self refers to the same person with the onset of dementia. This process should not be perceived as two separate decision-making processes or as a dichotomy, yet rather, as Gastmans (2017, 212) writes: “both past and present views of the person with dementia should be considered.” The idea behind this is that one may plan and make certain decisions before the onset of a disease, yet this can change throughout the disease course.
Limitations
The strength of this qualitative study was the in-depth focus group interviews with stakeholders, which enabled us to better understand and explore the different opinions, experiences, and perspectives about this topic. Qualitative research provides researchers with the opportunity to go beyond numerical quantitation and is very suitable for uncovering the reasons behind participants’ answers.
A limitation of the recruitment strategy of purposive sampling was that we used contact persons from specific settings, such as a pharmaceutical company. In addition, the FGs of healthy elderly, informal caregivers, and nursing staff consisted of participants from the same province in Belgium; somewhat different findings may emerge when recruiting in a different province of Belgium. This is combined with a limitation inherent to all qualitative research studies, namely that participants are embedded in a cultural and societal setting which can influence the results. For example, the mentioned euthanasia arrangement in our study is understandable due to the Belgian legislation on euthanasia yet would be unlikely in countries where euthanasia is forbidden. Another limitation is the absence of certain stakeholders, such as patient and dementia organizations, GPs, and family members. A strength of this study is the in-depth insight granted by the semi-structured methodology of presenting scenarios or cases and by using a starting question. This however limits the attention to other potentially interesting themes. Due to the large amount and richness of collected data, the presented results were limited to the most common addressed themes and important differences between FGs. However, the Supplementary material represents all data based on the concrete exercises participants filled out. This provides readers with the opportunity to have insight into the findings and smaller details of the data. Lastly, the discussions took place in Dutch, and used citations were translated in English, which means that some of the participants’ nuances may be lost.
Research agenda
Based on our study findings, future research should focus on the three following issues. Firstly, the views of stakeholders who wish not to know the result of their amyloid PET scan should be explored, as little insight is available in this matter. What are possible factors that may influence stakeholders to know or not to know their amyloid PET scan result? Secondly, what is the impact of knowing the amyloid PET scan result in the long term? Studies have mostly reported on the short-term consequences of knowing this type of information. Thirdly, the discrepancy of the “then self” versus the “now self” should be investigated. Studies have reported on this discrepancy in the decision-making process of the patient, yet only limited studies have investigated this topic from a qualitative matter. Qualitative studies with patients who have recently received an early diagnosis of AD may help to clarify this matter
Educational Implications
This exploratory focus group study reported on the views of five stakeholder groups and revealed two educational implications in the field of AD. Firstly, previous studies reported on high numbers of individuals who wish to know their result. This focus group study shows that many individuals do favour an early diagnosis and desire to be informed about their health. However, there were individuals who were in doubt about, or who preferred not to know, this result. The mentioned rationale to support their decision included the fear of AD, not wanting to burden their social environment, and the lack of an effective treatment for AD. This indicates that researchers and clinicians should never assume that all patients and participants want to be informed of their result.
Secondly, FG members reflected on several advantages and disadvantages of knowing their result, while it became clear that some topics were categorized between advantage and disadvantage, resulting in a “grey zone.” This indicates how possible consequences can be interpreted differently depending on personal coping strategy and personal views and values. For clinicians, researchers, and policymakers, it is important to describe these consequences to the individual prior to testing and to let patients decide by themselves whether they consider these consequences an advantage, a disadvantage, or in the “grey zone”.
Ethical Clearance
The study protocol and all necessary documents were submitted to the Social and Societal Ethics Commission (SMEC) of the University of Leuven (Belgium). The study and participant recruitment started after being granted permission by the Commission (study number G-2015 05 250). All study participants have signed an informed consent (IC).
References
Antoine, P., and F. Pasquier. 2013. Emotional and psychological implications of early AD diagnosis. The Medical Clinics of North America 97(3): 459–475.
Bazeley, P. 2007. Qualitative data analysis with NVivo, 2nd ed. SAGE Publications Ltd.
Betts Adams, K. 2006. The transition to caregiving: The experience of family members embarking on the dementia caregiving career. Journal of Gerontological Social Work 47(3/4) (June): 3–29.
Cahill, S., M. Clark, H. O’Connell, B. Lawlor, R.F. Coen, and C. Walsh. 2008. The attitudes and practices of general practitioners regarding dementia diagnosis in Ireland. International Journal of Geriatric Psychiatry 23(7): 663–669.
Chiu, H.F.K., and H. Brodaty. 2013. Arguments against the biomarker-driven diagnosis of AD. Journal Article. International Psychogeriatrics / IPA 25 (2): 177–181.
Connell, C.M., M.R. Janevic, and M.P. Gallant. 2001. The costs of caring: Impact of dementia on family caregivers. Journal of Geriatric Psychiatry and Neurology 14(4): 179–187.
Connell, C.M, L. Boise, J.C. Stuckey, S.B. Holmes, and M.L. Hudson. 2004. Attitudes toward the diagnosis and disclosure of dementia among family caregivers and primary care physicians. The Gerontologist 44(4): 500–507.
De Lepeleire, J., A.W. Wind, S. Iliffe, et al. 2008. The primary care diagnosis of dementia in Europe: An analysis using multidisciplinary, multinational expert groups. Aging & Mental Health 12(5): 568–576.
De Vugt, M.E., and F.R.J. Verhey. 2013. The impact of early dementia diagnosis and intervention on informal caregivers. Progress in Neurobiology 110: 54–62.
Dhedhi, S.A., D. Swinglehurst, and J. Russell. 2014. “Timely” diagnosis of dementia: What does it mean? A narrative analysis of GPs’ accounts. BMJ Open 4(3): e004439.
Draper, B., C. Peisah, J. Snowdon, and H. Brodaty. 2010. Early dementia diagnosis and the risk of suicide and euthanasia. Editorial review. Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association. United States.
Dubois, B., A. Padovani, P. Scheltens, A. Rossi, and G. Dell’Agnello. 2016. Timely diagnosis for Alzheimer’s Disease: A literature review on benefits and challenges. Journal of Alzheimer’s Disease 49(3): 617–631.
Frank, L., A. Lloyd, J.A. Flynn, et al. 2006. Impact of cognitive impairment on mild dementia patients and mild cognitive impairment patients and their informants. International Psychogeriatrics 18(1): 151.
Gastmans, C. 2017. Euthanasia in persons with severe dementia. In Euthanasia and Assisted Suicide: Lessons from Belgium, edited by C. Jones, D.A. Gastmans, and C. Mackellar, 212–216. Cambridge: Cambridge University Press.
Gastmans, C., and Y. Denier. 2010. What if patients with dementia use decision aids to make an advance euthanasia request? The American Journal of Bioethics: AJOB 10(4): 25–26.
Green, R.C., J.S. Roberts, N.R. Relkin, et al 2009. Disclosure of APOE genotype for risk of Alzheimer’s disease. The New England Journal of Medicine 361(3): 245–254.
Grill, J.D., C.G. Cox, S. Kremen, et al. 2017. Patient and caregiver reactions to clinical amyloid imaging. Alzheimer’s & Dementia 13(8): 924–932.
Grill, J.D., D.K. Johnson, and J.M. Burns. 2013. Should we disclose amyloid imaging results to cognitively normal individuals? Neurodegenerative Disease Management 3(1): 43–51.
Herholz, K., and K. Ebmeier. 2011. Clinical amyloid imaging in Alzheimer’s disease. The Lancet Neurology 10(7): 667–70.
Hsieh, H.-F., and S.E. Shannon. 2005. Three approaches to qualitative content analysis. Qualitative Health Research 15(9): 1277–1288.
Johnson, K.A., S. Minoshima, N.I. Bohnen, et al. 2013. Appropriate use criteria for amyloid PET: A report of the amyloid imaging task force, the Society of Nuclear Medicine and Molecular Imaging, and the Alzheimer’s Association. Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association 9(1): e-1–16.
Kitzinger, J. 1995. Qualitative research. Introducing focus groups. BMJ (Clinical Research Ed.) 311(7000): 299–302.
Lawrence, V., J. Pickett, C. Ballard, and J. Murray. 2014. Patient and carer views on participating in clinical trials for prodromal Alzheimer’s disease and mild cognitive impairment. International Journal of Geriatric Psychiatry 29(1): 22–31.
Lerner, A.J. 2013. Amyloid imaging: The court of public opinion. Neurology 81(13): 1108–1109.
Levi, B.H, and M.J. Green. 2010. Too soon to give up: Re-examining the value of advance directives. The American Journal of Bioethics 10(4): 3–22.
Lingler, J.H., and W.E. Klunk. 2013. Disclosure of amyloid imaging results to research participants: Has the time come? Alzheimer’s & Dementia : The Journal of the Alzheimer’s Association 9(6): 741–744.e2.
Mortelmans, D. 2007. Handboek Kwalitatieve Onderzoeksmethoden. Vierde. Leuven & Den Haag: Acco.
Neumann, P.J, J.K. Hammitt, C. Mueller, et al. 2001. Public attitudes about genetic testing for Alzheimer’s disease. Health Affairs (Project Hope) 20(5): 252–264.
Petersen, R.C., R. Doody, A. Kurz, et al. 2001. Current concepts in mild cognitive impairment. Archives of Neurology 58: 1985–1992.
Porteri, C., and G.B. Frisoni. 2014. Biomarker-based diagnosis of mild cognitive impairment due to Alzheimer’s disease: How and what to tell. A kickstart to an ethical discussion. Frontiers in Aging Neuroscience 6(January): 41.
Porteri, C., S. Galluzzi, C. Geroldi, and G.B. Frisoni. 2010. Diagnosis disclosure of prodromal Alzheimer disease: Ethical analysis of two cases. The Canadian Journal of Neurological Sciences. Le Journal Canadien Des Sciences Neurologiques 37(1): 67–75.
Prvulovic, D., and H. Hampel. 2011. Ethical considerations of biomarker use in neurodegenerative diseases--a case study of Alzheimer’s disease. Progress in Neurobiology 95(4): 517–519.
Roberts, J.S., L.A. Cupples, N.R. Relkin, P.J. Whitehouse, and R.C. Green. 2005. Genetic risk assessment for adult children of people with Alzheimer’s disease: The risk evaluation and education for Alzheimer’s disease (REVEAL) study. Journal of Geriatric Psychiatry and Neurology 18(4): 250–255.
Roberts, J.S., L.B. Dunn, and G.D. Rabinovici. 2013. Amyloid imaging, risk disclosure and Alzheimer’s disease: Ethical and practical issues. Neurodegenerative Disease Management 3(3): 219–229.
Robinson, L., E. Tang, and J.P. Taylor. 2015. Dementia: Timely diagnosis and early intervention. BMJ 350 (jun15/14): h3029–h3029.
Turner, S., S. Iliffe, M. Downs, et al. 2004. General practitioners’ knowledge, confidence and attitudes in the diagnosis and management of dementia. Age and Ageing 33(5): 461–467.
van Hout, H., M. Vernooij-Dassen, K. Bakker, M. Blom, and R. Grol. 2000. General practitioners on dementia: Tasks, practices and obstacles. Patient Education and Counseling 39(2–3): 219–225.
Vandenberghe, R., K. Adamczuk, P. Dupont, K. Van Laere, and G. Chételat. 2013a. Amyloid PET in clinical practice: Its place in the multidimensional space of Alzheimer’s disease. NeuroImage. Clinical 2(January): 497–511.
Vandenberghe, R., K. Adamczuk, and K. Van Laere. 2013b. The interest of amyloid PET imaging in the diagnosis of Alzheimer’s disease. Current Opinion in Neurology 26(0): 646–655.
Vanderschaeghe, G., J. Schaeverbeke, R. Bruffaerts, R. Vandenberghe, and K. Dierickx. 2017a. Amnestic MCI patients’ experiences after the disclosure of their amyloid PET result in a research context. Alzheimer’s Research & Therapy 9(92).
Vanderschaeghe, G., J. Schaeverbeke, R. Vandenberghe, and K. Dierickx. 2017b. Amnestic MCI patients’ perspectives toward disclosure of amyloid PET results in a research context. Neuroethics 10(2): 281–297..
Vollmann, J. 2001. Advance directives in patients with Alzheimer’s disease. Ethical and clinical considerations. Medicine, Health Care, and Philosophy 4(2): 161–167.
Werner, P., and A.D. Korczyn. 2008. Mild cognitive impairment: Conceptual, assessment, ethical, and social issues. Clinical Interventions in Aging 3(3): 413–420.
Widdershoven, G., and R.L. Berghmans. 2001. Advance directives in dementia care: From instructions to instruments. Patient Education and Counseling 44(2): 179–186.
Witte, M.M., N.L. Foster, A.S. Fleisher, et al. 2015. Clinical use of amyloid-positron emission tomography neuroimaging: Practical and bioethical considerations. Alzheimer’s & Dementia: Diagnosis, Assessment & Disease Monitoring, July.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
ESM
(PDF 539 kb)
Rights and permissions
About this article
Cite this article
Vanderschaeghe, G., Vandenberghe, R. & Dierickx, K. Stakeholders’ Views on Early Diagnosis for Alzheimer’s Disease, Clinical Trial Participation and Amyloid PET Disclosure: A Focus Group Study. Bioethical Inquiry 16, 45–59 (2019). https://doi.org/10.1007/s11673-019-09901-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11673-019-09901-9