Abstract
Summary
Despite the establishment of Fracture Liaison Services (FLS) worldwide, no study has evaluated their impact on the Portuguese population. Our work has shown that the implementation of an FLS is associated with a significant increase in OP treatment and a lower risk of secondary fracture.
Purpose
Fracture Liaison Services (FLS) have been established worldwide, with positive effects on treatment, secondary fracture, mortality, and economic burden. However, no study has evaluated their impact on the Portuguese population. Therefore, we purposed to evaluate the effect of an FLS model in a Portuguese center on osteoporosis (OP) treatment, secondary fracture, and mortality rates, 3 years after a fragility fracture.
Methods
Patients over 50 years old, admitted with a fragility fracture, between January 2017 and December 2020, were included in this retrospective study. Patients evaluated after FLS implementation (2019–2020) were compared with those evaluated before (2017–2018) and followed for 36 months. Predictors of secondary fracture and mortality were assessed using a multivariate Cox regression model, adjusted to potential confounders.
Results
A total of 551 patients were included (346 before and 205 after FLS). The FLS significantly increased the rate of OP treatment, when compared with standard clinical practice (8.1% vs 77.6%). During follow-up, the secondary fracture rate was 14.7% and 7.3%, before and after FLS, respectively. FLS was associated with a lower risk of secondary fracture (HR 0.39, C.I. 0.16–0.92). Although we observed a lower mortality rate (25.1% vs 13.7%), FLS was not a significant predictor of survival.
Conclusion
Implementing the FLS model in a Portuguese center has increased OP treatment and reduced the risk of secondary fracture. We believe that our work supports adopting FLS models in national programs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fragility fractures are the major outcomes of osteoporosis (OP) [1]. Besides pain and disability, there is an increased risk of subsequent fragility fractures and premature death, mainly within 2 years after the fracture [2]. It is estimated that 4.3 million fragility fractures occurred in Europe in 2019, which comes out to an average of 487 fractures per hour [3]. In Portugal, there were 70.730 fractures per 1000 habitants aged over 50 years in the same period [3]. The annual number of incident fragility fractures among Portuguese women older than 50 years old is 9.440 hip, 4.847 wrist, 3.491 vertebral, and 38.881 other fractures [4, 5]. An estimated prevalence of fragility fractures of 20.7% was shown in a large population database, the EpiReumaPt study, with only 7.1% of the senior women reporting being under OP treatment [6]. These numbers are expected to grow, due to increased life expectancy. It is estimated that the annual number of fragility fractures in Europe will increase by 1.06 million from 4.28 million in 2019 to 5.05 million in 2034 [3]. Despite successful treatment and national/international guidelines, there still is an alarming number of patients with fragility fractures who are not treated for OP in the setting of standard hospital care [3, 7, 8].
To address this public health problem, the International Osteoporosis Foundation (IOF) launched the Capture the Fracture campaign. This campaign promoted the establishment of Fracture Liaison Services (FLS) [8, 9] to reduce secondary fractures, by identifying patients with fragility fractures and initiating appropriate treatment. Since then, many FLS have been established in hospitals worldwide, with different models and organizations, that have demonstrated positive effects on fracture incidence and economic burden [10, 11]. Studies have shown that more intensive models might be the most effective to prevent fractures and lower morbidity rates [12,13,14]. Currently, nine FLS have been created in Portugal [15], but their impact on Portugal’s population has yet to be assessed. Our FLS (Unidade Coordenadora Funcional da Osteoporose) was implemented in January 2019 with the primary objective to reduce the risk of secondary fracture. Therefore, this study aimed to evaluate the effect of a FLS model in a Portuguese center, on OP treatment, secondary fracture, and mortality rates, 3 years after a fragility fracture, compared with the previous standard of care in a homologous time.
Methods
Study design and participants
A retrospective cohort study was conducted on patients over 50 years old, who suffered a fragility fracture and were treated in our institution, between January 2017 and December 2020. Fragility fractures included hip, vertebral, wrist, and other fractures, such as the humerus, elbow, and lower leg. The same fracture locations used in the scorecard for osteoporosis in Europe (SCOPE 2021) were included [3]. Patients with pathological and traumatic fractures, who died in the orthopaedic ward after surgery or cognitive dysfunction, or dementia cases were excluded. Socio-demographic, such as age and gender, and clinical data, such as body mass index (BMI), functional status, number of previous fractures, secondary fractures, chronic non-communicable diseases, type of fracture, hospitalization, mortality, and initiation of OP drugs, were collected from our local computerized and national databases (PDS-Health Data Platform). Chronic non-communicable diseases were collected according to the registries: hypertension, diabetes mellitus, dyslipidaemia, thyroid or parathyroid disorders (hypo or hyperthyroidism and hypo or hyperparathyroidism), cardiovascular diseases (coronary disease, arrhythmia, heart valves problems, heart failure, or cardiomyopathy), respiratory diseases (chronic bronchitis, asthma, or pulmonary fibrosis), chronic kidney diseases, rheumatic inflammatory diseases (rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, gout, rheumatic polymyalgia, or systemic erythematosus lupus), neurological diseases (stroke, migraines, multiple sclerosis, Parkinson’s disease, peripheral polyneuropathy, or myopathy), depression, and cancer; lifestyle behaviors: smoke and alcohol abuse. The number of chronic non-communicable diseases was determined for each respondent, with multimorbidity defined as the presence of two or more of these disorders [16]. Secondary fragility fractures, hospitalizations, and mortality were assessed 36 months from the date of the index fracture. Patients evaluated from January 2019 to March 2020 (during FLS) were compared with patients hospitalized between January 2017 and December 2018 (before FLS). Before the implementation of the FLS protocol, patients received standard fracture care during hospitalization and OP was managed mainly by primary care.
FLS protocol
The protocol described here is based on the cooperation between Orthopaedic/Traumatology and Rheumatology Departments. When the patient presents at the emergency department of our hospital, following a low-energy fracture, an X-ray of the fracture site is taken, and two situations may occur: (A) the patient may undergo Orthopaedic/Traumatology surgery to treat the fracture and then be admitted to the Orthopaedic/Traumatology ward or (B) the patient will be admitted to the Orthopaedic/Traumatology ward to wait for surgery. At this point, FLS is activated in eligible patients. All the patients are evaluated through a questionnaire collecting sociodemographic (age at fracture and gender) and clinical data (body mass index, lifestyle behaviors: current smoking and alcohol use, chronic non-communicable diseases, previous fractures, dependence status (Katz index), previous OP treatments, type of fracture). They undergo laboratory tests (including renal and hepatic function, phosphocalcium metabolism, and protein electrophoresis) and thoracolumbar spine X-rays to exclude asymptomatic fractures. During the in-patient period, physical therapy for functional recovery and OP treatment is started, at the osteoporotic clinic, according to the Portuguese recommendations, where alendronic acid is the first-line therapy [17]. Treatment is prescribed in patients with one fragility fracture of the hip or two or more fragility fractures, independently of the site of the fracture, or with estimates of FRAX®Portugal ≥ 11% for major osteoporotic fracture or ≥ 3% for hip fracture [17]. OP treatment is not prescribed to patients with cognitive dysfunction, dementia, on dialysis or who are bedridden. Information is sent directly to the primary care physician (Fig. 1). Since the protocol had no experimental design, ethical approval, and informed consent were not required.
Statistical analysis
A general descriptive analysis of data was performed. Categorical variables were presented as absolute values and percentages, and continuous variables as means and their corresponding standard deviations. The chi-square test and t-test student were used to determine differences between before and after FLS groups by comparing categorical and continuous variables. Patients who suffered fractures before and after FLS were only included in the after FLS group.
The patient’s survival was determined using Kaplan–Meier analysis. First, an analysis was done to estimate the risk of a secondary fragility fracture at the end of the 36-month follow-up period; in this analysis, deaths and patients lost to follow-up were censored to avoid possible bias. A second analysis was performed to estimate mortality risk where the outcomes were either death or end of the 36-month follow-up; in this analysis, patients lost to follow-up were censored.
Mortality and secondary fragility fracture rates were compared between the two groups using a multivariate Cox proportional hazard model adjusted to potential confounders such as age, gender, the status of dependence, multimorbidity, previous fractures, fractures, and OP treatment.
SPSS software© version 27 was used and a p-value ≤ 0.05 was considered statistically significant.
Results
A total of 551 patients with fragility fracture were included the following: 346 before and 205 after FLS implementation. Socio-demographic and clinical characteristics are presented in Table 1. Most patients were women (83.5%) with a mean age of 80.83 ± 8.86 years old [82.08 ± 7.66 years before FLS and 78.72 ± 10.26 years after FLS (p < 0.001)]. No statistically significant differences between groups regarding gender and BMI were found. More previous fractures were observed in the group after FLS implementation (34.1% vs 15.4%, p < 0.001); however, we did not find differences in previous OP treatment (10.4% vs 14.1%, p = 0.188). There were no statistically significant differences in chronic non-communicable diseases between the two groups, except for neurological diseases (21.6% vs 12.5%, p = 0.008). The most frequent fracture in both groups was hip fractures (80.3% vs 65.4%, p = < 0.001). OP treatment was given in 28 cases (8.1%) before FLS, compared to 159 patients (77.6%) observed after FLS (p = 0.001). In both groups, the most prescribed drug was oral alendronic acid, while parental treatment (zoledronic acid intravenous and denosumab subcutaneous) was only prescribed after FLS implementation.
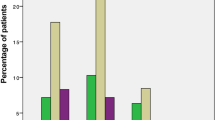
The mean follow-up time was 41.40 ± 14.73 months (before FLS 41.79 ± 16.67 months and after FLS 40.72 ± 10.67 months, p = 0.414). A total of 58 patients (10.5%) suffered a secondary fracture: 46 (13.3%) compared with 12 (5.9%) patients, before and after FLS implementation, respectively (p = 0.006). The most common secondary fracture types were hip (53.03%), followed by wrist (16.67%), and vertebral (12.12%). Overall, 32 (55.17%) secondary fractures were observed in the first year, 9 (15.52%) in the second year, and 17 (29.31%) in the third year. The Cox proportional hazards model showed a significantly lower refracture rate in FLS patients before and after adjusting for age, gender, previous fracture, multimorbidity, dependence status (Katz < 3), and OP treatment (HR 0.39, C.I. 0.16–0.92) (Fig. 2; Table 2). We did not find other predictors of secondary fracture.
During the follow-up period, 95 patients (17.2%) died: 47 patients (49.47%) in the first year, 26 patients (27.37%) in the second year, and 22 patients (23.16%) in the third year. A higher number of deaths were observed before FLS implementation (20.5% vs 11.7%, p = 0.008) (Table 1). Survival was higher in FLS patients (HR 0.56, C.I. 0.35–0.89). However, this finding was not found after adjusting for age, gender, dependence status, fracture site, multimorbidity, and beginning of OP treatment (Fig. 3; Table 3). Male gender (HR 1.78, C.I. 1.11–2.86), older age at time of fracture (HR 1.04, C.I. 1.01–1.07), and a more dependent functional status (Katz < 3) (HR 2.38, C.I. 1.49–3.81), were found to increase mortality risk independently (Table 3).
Discussion
This study was performed to evaluate the impact of the implementation of a Portuguese FLS on OP treatment, secondary fracture, and mortality rates three years after a fragility fracture. As expected, in our study, senior female patients were predominant, before and after FLS implementation, with multiple chronic non-communicable diseases and previous fractures but a lower prevalence of previous OP treatment.
Our FLS increased the rate of OP treatment prescription (77.6%) when compared with standard clinical care (8.1%). The percentage of patients who initiated their OP treatment in our FLS (77.6%) is in line with other FLS studies published in the literature (77% [18] and 78.4% [19]). In a study conducted in 2013 in a Portuguese tertiary hospital center, the authors found that 12.1% of the patients who suffered a hip fracture had initiated OP treatment in the setting of standard clinical care [20]. This percentage is higher compared to what we found in our study (8.1%), during the period before FLS implementation. In a systematic review published in 2018, was reported an increase of at least 20% in OP treatment, compared with standard management [21]. In our cohort, oral alendronic acid was the most prescribed treatment. This is in balance with national treatment recommendations, where alendronic acid is the first-line therapy since it is cost-effective [17, 22]. Parental treatments were reserved for patients with higher-risk fractures and/or chronic renal disease and patients with poor oral treatment adherence. In Portugal, OP treatment is supported mostly by the National Health System and in a small part by the patient. In the case of denosumab, teriparatide, and zoledronic acid, the amount of money charged to the patients is higher than for alendronic acid [22]. This may explain why the most prescribed treatment was oral alendronic acid. Regarding secondary fractures, we observed a significantly lower incidence after the implementation of our FLS, in line with other studies [23, 24]. Our adjusted model showed that FLS reduced the probability of secondary fracture (HR 0.39, C.I. 0.16–0.92), which was also reported by a recent systematic review and meta-analysis (HR 0.70, C.I. 0.52–0.93) [25]. Although FLS increased the prescription rate of OP treatment, the present study did not show an association between OP treatment and secondary fracture risk. Nevertheless, OP treatment consists not only of pharmacological treatment but also of non-pharmacological treatment such as healthy lifestyle behaviors and avoidance of falls, which were not evaluated in our study. This suggests that non-pharmacological treatment can be extremely important in the first years after a fracture [26].
Patients who suffered a fragility fracture have a lower life expectancy compared to the general population and FLS can improve patient’s survival [18, 27, 28]. Two systematic reviews and meta-analyses observed a lower mortality risk in patients managed by FLS models when compared with standard clinical care [21, 25]. Patients treated in FLS had a lower mortality rate when compared with patients managed before FLS. However, in our study, the FLS implementation was not associated with a lower risk of mortality, after model adjustment to age, gender, the status of dependence, multimorbidity, previous fractures, and OP treatment. We observed that an older age at fracture time, male gender, and worse functional status (Katz < 3) were found to increase mortality risk. Since the FLS group had younger patients than those observed before FLS, this could have influenced mortality rates. However, after model adjustment, we observed that a higher age when suffering a fragility fracture will increase mortality risk, which is expected since the elderly are associated with higher morbidity and lower recovery capacity [29]. Some studies have reported worse fracture outcomes in male patients [30]. Differences in hip fractures were considered and did not influence secondary fractures or mortality risk, after model adjustment. Little is known about the impact of multimorbidity in OP. Multimorbidity was found to be a predictor of fragility fractures in Portuguese women ≥ 50 years old, and their combination was associated with worse quality of life and disability [31]. Moreover, a recent Australian study observed a lower treatment rate in patients with hip fractures and multimorbidity [32]. Since most patients with OP are old, frail, and have multimorbidity, FLS models must have a multidisciplinary approach to better evaluate and treat these patients [33].
The FLS model has gained more importance as an effective approach to OP treatment and secondary fracture prevention. More evidence has emerged and is important to promote the implementation and funding of this model by national governments. In Portugal, there is no data regarding the efficacy of FLS implementation. The present study is the first to report the benefits of the FLS model in OP treatment initiation, secondary fracture prevention, and mortality in the Portuguese population. Moreover, is the first study to report the real-world effectiveness of the FLS itself from a clinical perspective. However, this study has limitations, mainly concerning its retrospective design and the data being from a single center. Although implemented, we did not evaluate non-pharmacological therapy and fall prevention. Concerning our reality, the FLS implementation allowed the identification and treatment of risk patients, and better communication with primary care, who manage most of the patients with OP in Portugal. Follow-up and treatment adherence were not specifically addressed in this study. Future work with more patients, multicenter and longer follow-up periods will provide further extrapolations about the socioeconomic impact on the hospital system and patient care quality, in Portugal.
Conclusion
The implementation of the FLS model in a Portuguese center has increased OP treatment and reduced the risk of secondary fracture. This is the first study evaluating the impact of an FLS in the Portuguese population, supporting its efficacy, as described previously worldwide. We believe that our work supports the establishment of national programs, with the adoption of the FLS model, which could lead to better OP outcomes regarding fractures and mortality, and promote quality of life.
References
Pisani P, Renna MD, Conversano F et al (2016) Major osteoporotic fragility fractures: risk factor updates and societal impact. World J Orthop 7(3):171–181. https://doi.org/10.5312/wjo.v7.i3.171
Branco JC, Rodrigues AM, Gouveia N et al (2016) Prevalence of rheumatic and musculoskeletal diseases and their impact on health-related quality of life, physical function and mental health in Portugal: results from EpiReumaPt- a national health survey. RMD Open 2(1):e000166. https://doi.org/10.1136/rmdopen-2015-000166
Kanis JA, Norton N, Harvey NC et al (2021) SCOPE 2021: a new scorecard for osteoporosis in Europe. Arch Osteoporos 16(1):82. https://doi.org/10.1007/s11657-020-00871-9
Barcelos A, Gonçalves J, Mateus C, Canhão H, Rodrigues AM (2023) Costs of incident non-hip osteoporosis-related fractures in postmenopausal women from a payer perspective. Osteoporos Int. https://doi.org/10.1007/s00198-023-06881-w
Barcelos A, Gonçalves J, Mateus C, Canhão H, Rodrigues AM (2023) Costs of hip fractures in postmenopausal women in Portugal: a study from the payer’s perspective. Acta Med Port 36(12):848–849. https://doi.org/10.20344/amp.20481
Rodrigues AM, Eusébio M, Santos MJ et al (2018) The burden and undertreatment of fragility fractures among senior women. Arch Osteoporos 13(1):22. https://doi.org/10.1007/s11657-018-0430-z
Costa R, Romano J, Moreira A et al (2021) The aftermath of hip fragility fractures - are we missing out on osteoporosis treatment? Acta Reumatol Port 46(4):328–332
Hiligsmann M, Cornelissen D, Vrijens B et al (2019) Determinants, consequences and potential solutions to poor adherence to anti-osteoporosis treatment: results of an expert group meeting organized by the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO) and the International Osteoporosis Foundation (IOF). Osteoporos Int 30(11):2155–2165. https://doi.org/10.1007/s00198-019-05104-5
Akesson K, Marsh D, Mitchell PJ et al (2013) Capture the fracture: a Best Practice Framework and global campaign to break the fragility fracture cycle. Osteoporos Int 24(8):2135–2152. https://doi.org/10.1007/s00198-013-2348-z
Walters S, Khan T, Ong T, Sahota O (2017) Fracture liaison services: improving outcomes for patients with osteoporosis. Clin Interv Aging 12:117–127. https://doi.org/10.2147/CIA.S85551
Briot K (2017) Fracture liaison services. Curr Opin Rheumatol 29(4):416–421. https://doi.org/10.1097/BOR.0000000000000401
Ganda K, Puech M, Chen JS et al (2013) Models of care for the secondary prevention of osteoporotic fractures: a systematic review and meta-analysis. Osteoporos Int 24(2):393–406. https://doi.org/10.1007/s00198-012-2090-y
Paccou J, Philippoteaux C, Cortet B, Fardellone P (2023) Effectiveness of fracture liaison services in osteoporosis. Joint Bone Spine 90(5):105574. https://doi.org/10.1016/j.jbspin.2023.105574
Pflimlin A, Gournay A, Delabrière I et al (2019) Secondary prevention of osteoporotic fractures: evaluation of the Lille University Hospital’s Fracture Liaison Service between January 2016 and January 2018. Osteoporos Int 30(9):1779–1788. https://doi.org/10.1007/s00198-019-05036-0
– Capture the Fracture® map of best practice. https://www.capturethefracture.org/map-of-best-practice. Accessed 15 October 2023
Mercer M, Salisbury S, Fortin C (2014) ABC of multimorbidity. BMJ Publishing Group Limited, London
Rodrigues AM, Canhão H, Marques A et al (2018) Portuguese recommendations for the prevention, diagnosis and management of primary osteoporosis - 2018 update. Acta Reumatol Port 43(1):10–31
Scholten DJ, Bray JK, Wang KY, Lake AF, Emory CL (2020) Implementation of a fracture liaison service and its effects on osteoporosis treatment adherence and secondary fracture at a tertiary care academic health system. Arch Osteoporos 15(1):80. https://doi.org/10.1007/s11657-020-00736-1
González-Quevedo D, Pérez-Del-Río V, Moriel-Garceso D et al (2022) A 2-year follow-up of a novel Fracture Liaison Service: can we reduce the mortality in elderly hip fracture patients? A prospect Cohort Study Osteoporos Int 33(8):1695–1702. https://doi.org/10.1007/s00198-022-06298-x
Daniel A, Marques ML, Brites L, Torres C, Marques A, Pereira da Silva JA (2018) Adherence to the recommended prevention strategies before and after a hip fragility fracture: what makes us go blind? Acta Reumatologica Port 43(2):93–101
Wu CH, Tu ST, Chang YF et al (2018) Fracture liaison services improve outcomes of patients with osteoporosis-related fractures: a systematic literature review and meta-analysis. Bone 111:92–100. https://doi.org/10.1016/j.bone.2018.03.018
Marques A, Lourenço Ó, Ortsäter G, Borgström F, Kanis JÁ, da Silva JA (2016) Cost-effectiveness of intervention thresholds for the treatment of osteoporosis based on FRAX(®) in Portugal. Calcif Tissue Int 99(2):131–141. https://doi.org/10.1007/s00223-016-0132-8
Nakayama A, Major G, Holliday E, Attia J, Bogduk N (2016) Evidence of effectiveness of a fracture liaison service to reduce the re-fracture rate. Osteoporos Int 27(3):873–879. https://doi.org/10.1007/s00198-015-3443-0
Axelsson KF, Johansson H, Lundh D, Möller M, Lorentzon M (2020) Association between recurrent fracture risk and implementation of fracture liaison services in four Swedish hospitals: a cohort study. J Bone Miner Res 35(7):1216–1223. https://doi.org/10.1002/jbmr.3990
Li N, Hiligsmann M, Boonen A et al (2021) The impact of fracture liaison services on subsequent fractures and mortality: a systematic literature review and meta-analysis. Osteoporos Int 32(8):1517–1530. https://doi.org/10.1007/s00198-021-05911-9
Morfeld JC, Vennedey V, Müller D, Pieper D, Stock S (2017) Patient education in osteoporosis prevention: a systematic review focusing on methodological quality of randomised controlled trials. Osteoporos Int 28(6):1779–1803. https://doi.org/10.1007/s00198-017-3946-y
Barahona M, Barrientos C, Cavada G, Brañes J, Martinez Á, Catalan J (2020) Survival analysis after hip fracture: higher mortality than the general population and delayed surgery increases the risk at any time. Hip Int 30(1):54–58. https://doi.org/10.1177/1120700020938029
Hawley S, Javaid MK, Prieto-Alhambra D et al (2016) Clinical effectiveness of orthogeriatric and fracture liaison service models of care for hip fracture patients: population-based longitudinal study. Age and ageing 45(2):236–242. https://doi.org/10.1093/ageing/afv204
Dyer SM, Crotty M, Fairhall N et al (2016) Fragility Fracture Network (FFN) Rehabilitation Research Special Interest Group. A critical review of the long-term disability outcomes following hip fracture. BMC Geriatr 16(1):158. https://doi.org/10.1186/s12877-016-0332-0
Bliuc D, Alarkawi D, Nguyen TV, Eisman JA, Center JR (2015) Risk of subsequent fractures and mortality in elderly women and men with fragility fractures with and without osteoporotic bone density: the Dubbo Osteoporosis Epidemiology Study. J Bone Miner Res 30(4):637–646. https://doi.org/10.1002/jbmr.2393
Barcelos A, Lopes DG, Canhão H, da Cunha BJ, Rodrigues AM (2021) Multimorbidity is associated with fragility fractures in women 50 years and older: a nationwide cross-sectional study. Bone reports 15:101139. https://doi.org/10.1016/j.bonr.2021.101139
Bliuc D, Tran T, Chen W et al (2023) The association between multimorbidity and osteoporosis investigation and treatment in high-risk fracture patients in Australia: a prospective cohort study. PLoS medicine 20(1):e1004142. https://doi.org/10.1371/journal.pmed.1004142
Magalhães P, Gonçalves M, Silva F, Fernandes T, Oliveira A, Veríssimo R (2023) Implementation of orthogeriatrics in Portugal. Cureus 15(2):e35361. https://doi.org/10.7759/cureus.35361
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Silva, S.P., Mazeda, C., Vilas-Boas, P. et al. The impact of a Fracture Liaison Service after 3 years on secondary fracture prevention and mortality in a Portuguese tertiary center. Arch Osteoporos 19, 4 (2024). https://doi.org/10.1007/s11657-023-01363-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-023-01363-2