Abstract
Summary
Our results revealed that the decrease in isometric knee extension muscle strength on the operated and nonoperated sides in patients with hip fractures was associated with not only a decrease in skeletal muscle mass but also a decrease in muscle quality, characterized by a decreased PhA.
Purpose
This study aimed to assess the relationship between isometric knee extension muscle strength on the operated or nonoperated sides and PhA in patients with hip fractures at approximately 6 months postoperatively.
Methods
This study was a cross-sectional study. Skeletal muscle index (SMI), PhA, knee extension muscle strength on the operated and nonoperated sides, and other physical function variables were assessed at approximately 6 months postoperatively. To identify predictors of knee extension muscle strength on the operated and nonoperated sides, hierarchical multiple regression analysis was performed.
Results
A total of 90 patients with hip fractures were included (mean age, 80.1 ± 6.9 years). SMI (0.45) and PhA on the operated side (0.27) were the significant associated factors extracted for isometric knee extension muscle strength on the operated side (standardized partial regression coefficients), independent of age, sex, and body mass index (BMI). Movement control during one-leg standing on the nonoperated side (0.26), SMI (0.32), and PhA on the nonoperated side (0.40) were the significant associated factors extracted for isometric knee extension muscle strength on the nonoperated side, independent of age, sex and BMI.
Conclusions
Our results revealed that the decrease in isometric knee extension muscle strength on the operated and nonoperated sides in patients with hip fractures at approximately 6 months postoperatively was associated with not only a decrease in skeletal muscle mass but also a decrease in muscle quality, characterized by a decreased PhA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with hip fractures following surgery experience problems, including loss of motor functions. A previous study reported that 40%–60% of patients with hip fractures at 6 months postoperatively had reduced gait function compared with pre-fracture levels [1]. Furthermore, it is well known that patients with hip fractures often have decreased knee extension strength [2], which is associated with higher mortality in several diseases, such as musculoskeletal diseases, including patients with hip fractures [3]; cardiovascular diseases [4]; and respiratory diseases [5]. Therefore, recovery of knee extension strength is one of the most significant targets of rehabilitation [6, 7]. For effective rehabilitation, it may be useful to determine factors that cause and predict low knee extension strength [8, 9].
Decreased knee extension muscle strength in patients with hip fractures is associated with fracture type [10], low balance [10], low gait speed [10], and severe pain [11]. Furthermore, it is well known that muscle cross-sectional area is correlated with muscle strength [12], and low knee extension muscle strength in patients with hip fractures in the early 1970s has been observed to be associated with low muscle mass [11]. However, decreased muscle strength occurring in older adults, including those with diseases, is frequently not explained solely by low muscle mass. For example, in patients with heart failure, although the muscle mass was comparable, muscle strength was significantly reduced compared with healthy participants [13], indicating the contribution of other factors other than muscle mass. Moreover, decreased muscle quality is believed to contribute to a decrease in muscle strength. A previous study reported that maintaining or increasing skeletal muscle mass could not prevent decreased strength when muscle quality was decreased [14]. Based on these findings, we speculate that a decrease in muscle quality, as well as muscle mass, contributes to the decreased knee extension muscle strength observed in patients with hip fractures.
The phase angle (PhA) can be calculated simultaneously with muscle mass by bioelectrical impedance analysis and is a useful muscle quality parameter [15]. PhA can be calculated by bioelectrical impedance using the following two indices: reactance (cell membrane intrinsic resistance [Xc]) and resistance (intracellular and extracellular resistance [R]). Theoretically, Xc is a measure of the capacitance volume of the cell membrane, and its resistance to current is determined by body fat, total body water, and extracellular water [16]. Therefore, PhA is considered a cell membrane integrity marker [17]. Previous studies showed that disease and dysfunction could cause a secondary decrease in the PhA by disrupting the electrical properties of tissues [18]. Lower PhA was shown to be associated with lower muscle strength and higher mortality in community-dwelling older adults [19]. Similarly, low PhA in patients with cardiac disease was noted to be significantly associated with low knee extension strength, independent of age and body mass index (BMI) [20]. Additionally, PhA was reported to be positively correlated with lower limb muscle strength in patients with knee or hip osteoarthritis [21, 22]. However, although muscle weakness on the operated and nonoperated sides occurs after hip fracture, the association between the PhA and knee extension strength on the operated and nonoperated sides in patients with hip fractures has not been investigated.
Therefore, this study aimed to assess the relationship between isometric knee extension muscle strength on the operated or nonoperated side and PhAs in patients with hip fractures at approximately 6 months postoperatively.
Materials and methods
Study design and setting
This study was a cross-sectional study and was performed in a hospital from April 2019 to February 2022. Recruitment, follow-up, and data collection were performed by the rehabilitation staff of the cooperating hospital. All patients provided written informed consent after a detailed explanation of the protocol. This study was conducted with the approval of the Ethics Committee in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology statement according to the Declaration of Helsinki.
Patients
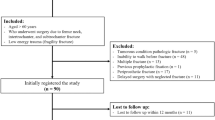
The study included patients with hip fractures, and measurements were taken at approximately 6 months postoperatively. The inclusion criteria included patients with hip fractures aged 65 years or older who were able to walk independently. The exclusion criteria included those who had a pacemaker or had severe dementia. Severe dementia was defined as a revised Hasegawa’s dementia scale (HDS-R) score of 9 or less. The required sample size was calculated using G × power 3.1.9.6. A sample size analysis with an alpha value of 0.05, power of 0.8, and effect size f2 of 0.15 determined a sample size of 92 patients.
Intervention
Patients with hip fractures underwent surgery, pharmacotherapy, and exercise therapy interventions. The surgical options were osteosynthesis or artificial femoral head replacement, depending on the fracture type. Pharmacotherapy was performed in all patients to reduce pain pre- and postoperatively. The contents of exercise therapy were determined by the therapist following the physician’s orders. The intervention period was from the first day after the surgery until hospital discharge. The interventions included functional exercises (neuromuscular exercises, range of motion exercises, and resistance training), gait exercises, activities of daily living exercises, and psychological support for the patient and family. Following hospital discharge, the physician explained to the patients and their families that rehabilitation should be continued.
Bioelectrical impedance analysis
We assessed body composition via multiple-frequency bioelectrical impedance analysis (InBody S10, InBody, Tokyo, Japan) using six different frequencies (1, 5, 50, 250, 500, and 1000 kHz). Patients remained supine on the bed with their arms and legs abducted, and reusable contact electrodes were placed on the first and third fingers of both hands and the medial and lateral sides of both ankles. We calculated the skeletal muscle index (SMI) by dividing the limb skeletal muscle mass (kg) by the square of the height (m2). Based on bioelectrical impedance measurements, we calculated the PhA from the relationship between the resistance and reactance vectors. To calculate the PhA, we used a resistance and reactance of 50 kHz; the PhAs in the right and left lower limbs were used for analysis.
Isometric knee extension muscle strength
According to the methods described in a previous study [23], isometric knee extension muscle strength on the operated and nonoperated sides was measured using a hand-held dynamometer (HHD) (Anima Corp., Tokyo, Japan). Patients sat on a chair with their trunks kept straight and perpendicular using both hands on the bench beside the body. An HHD sensor was fixed to the anterior side of the lower leg using a traction belt placed between the level of the lateral malleolus of the lower leg and the main pillar behind the chair. Using the HHD, isometric knee muscle extension strength was measured for 5 s at a flexion angle of 90°, taking care to keep the traction belt parallel to the floor. Measurements were repeated two times with at least 30-s intervals between measurements. Corrected muscle strength was calculated using the following equation: muscle strength measured by HHD × lower leg length (nearly the moment arm)/body weight. Lower leg length was measured as the distance between the lateral femoral epicondyle and the lateral malleolus.
Other physical function variables
Walking form and speed, pain, movement control during one-leg standing, one-leg standing time, and hand grip strength were the other physical function variables. Walking form was determined to be a form of independent walking, including walking without support, walking with a cane, or walking with a walker. Walking speed was measured as the time taken to walk a distance of 10 m at a comfortable speed. Two measurements were taken, and the maximum value (m/min) was used as the representative value. Pain intensities at rest and during activity of the hip joint on the operated side were assessed using the numerical rating scale (NRS). The NRS is divided into 11 stages from 0 to 10, with 0 indicating no pain at all and 10 indicating the worst possible pain. According to the methods of a previous study, we measured the movement control during one-leg standing [24], one-leg standing time [25], and hand grip strength [26]. The following were the three criteria for movement control during one-leg standing: criterion 1 states that the hip joint should remain stable in the extension and intermediate positions during rotation and abduction–adduction movements. The pelvis and upper body should not move from their initial position: criterion 2 states that the vertical axis of the leg should remain straight, and varus or valgus should not occur. The patella should be directed to the third metatarsal: criterion 3 states that a component was considered incorrect when intermittent support by the hand against the wall or the contralateral foot on the floor was necessary. The component was considered to have > 1 incorrect component if additional support was needed throughout the exercise. A three-point Likert scale was used for evaluation, where 2 points indicated that all criteria were correct, 1 point indicated that 1 criterion was incorrect, and 0 points indicated that > 1 criterion was incorrect or false.
Other measurement variables
Age, sex, BMI, presence of family living together, HDS-R score, fracture type and side, operative type, previous medical history (chronic obstructive pulmonary disease, cardiovascular disease, cerebrovascular disease, cancer, hypertension, diabetes, chronic kidney disease, and other fractures), geriatric nutritional risk index (GNRI), and degree of sarcopenia were the other measurements included. Sarcopenia was determined using the Asian Working Group for Sarcopenia 2019 methods [27]. The degree of sarcopenia was evaluated using the presence of low muscle mass, low muscle function, and low physical function. Low muscle mass was defined as a skeletal muscle mass index of less than 7.0 and 5.7 kg/m2 for male and female patients, respectively. Low muscle strength was defined as a hand grip strength of less than 28 and 18 kg for male and female patients, respectively. Low physical function was defined as a gait speed of > 1.0 m/s. Severe sarcopenia was defined as having all of the following parameters: low skeletal muscle mass index, low muscle strength, and low physical function [27]. Sarcopenia was defined as low skeletal muscle mass index and low muscle strength or low physical function [27].
Statistical analysis
All statistical analyses were performed using Statistical Package for the Social Sciences version 29 version Windows (IBM SPSS Japan, Tokyo, Japan).
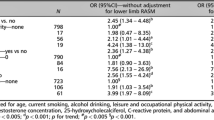
To identify factors associated with isometric knee extension muscle strength on the operated and nonoperated sides, hierarchical multiple regression analysis was performed. When the knee extension muscle strength on the operated side was the dependent variable, the independent variables were SMI, PhA on the operated side, walking form and speed, pain, movement control during one-leg standing on the operated side, and other measurement variables. When the knee extension muscle strength on the nonoperated side was the dependent variable, the independent variables were SMI, PhA on the nonoperated side, walking form and speed, pain and movement control during one-leg standing on the nonoperated side, and other measurement variables. First, age, sex, and BMI were forced in as block 1. Using a stepwise method, the other independent variables were entered in block 2. Factors related to knee extension muscle strength on the operated and nonoperated sides were separately extracted from the confounding factors (age, sex, and BMI). The threshold of the correlation coefficient between independent factors was set to 0.8 to account for multicollinearity, selecting those with a high correlation with the dependent variable. The significance level was set at 5%.
Results
A total of 101 patients with hip fractures met the inclusion criteria. Of these, 4 and 7 had pacemakers inserted and severe dementia, respectively; therefore, 11 patients were excluded from the analyses. Finally, a total of 90 patients were included in the analyses (mean age, 80.1 ± 6.9 years). The patient characteristics are presented in Table 1.
Correlation analysis revealed relationships between independent variables and age, sex, BMI, dwelling place, presence of family living together, HDS-R score, fracture type and side, presence or absence of medical history, GNRI, degree of sarcopenia, walking form, 10-m gait speed, pain movement control during one-leg standing, one-leg standing time, hand grip strength, SMI, and PhA in the hierarchical multiple regression model. The results of the hierarchical multiple regression analysis are shown in Table 2. The SMI and PhA on the operated side were the significant associated factors extracted for isometric knee extension muscle strength on the operated side, independent of age, sex, and BMI. Standardized partial regression coefficients representing the magnitude of involvement of each independent variable were 0.45 and 0.27 for the SMI and PhA, respectively. The coefficient of determination adjusted for degrees of freedom (R2), representing the contribution rate of the regression equation, was 0.256. Movement control during one-leg standing on the nonoperated side, SMI, and PhA on the nonoperated side were the significant associated factors extracted for isometric knee extension muscle strength on the nonoperated side, independent of age, sex, and BMI. Standardized partial regression coefficients representing the magnitude of involvement of each independent variable were 0.26, 0.32, and 0.40 for movement control during one-leg standing, SMI, and PhA, respectively. The coefficient of determination adjusted for degrees of freedom (R2), representing the contribution rate of the regression equation, was 0.384.
Discussion
This study aimed to assess the relationship between isometric knee extension muscle strength on the operated or nonoperated side and PhA in patients with hip fractures at approximately 6 months postoperatively. Our hierarchical multiple regression analysis showed that the significant associated factors extracted for isometric knee extension muscle strength on the operated side were SMI and PhA on the operated side, independent of age, sex, and BMI. The significant associated factors extracted for isometric knee extension muscle strength on the nonoperated side were movement control during one-leg standing on the nonoperated side, SMI, and PhA on the nonoperated side, independent of age, sex, and BMI. We revealed that the decrease in isometric knee extension muscle strength on the operated and nonoperated sides in patients with hip fractures at approximately 6 months postoperatively is associated with not only a decrease in skeletal muscle mass but also a decrease in muscle quality, characterized by a decreased PhA. Therefore, it is necessary to improve not only muscle mass but also muscle quality to improve muscle strength in patients with hip fractures at approximately 6 months postoperatively.
The decrease in the SMI was significantly associated with a decrease in isometric knee extension muscle strength on the operated and nonoperated sides. In a previous study [28], SMI was observed to be associated with muscle strength. In our study, the SMI was related to muscle strength, and our result is consistent with the results of the previous study. The poor movement control during one-leg standing on the nonoperated side was significantly associated with a decrease in isometric knee extension muscle strength on the nonoperated side. Because muscle strength is assumed to be involved in movement control during one-leg standing [29], this association is not surprising. However, this association was not observed on the operated side. The operated side (80%) had a higher percentage of patients grasping something during one-leg standing, which is one of the subtractive items, than the nonoperated side (65%). Therefore, it is possible that the association between muscle strength and movement control during one-leg standing was masked by providing support with the upper extremity on the operated side.
The decreases in the PhAs were significantly associated with a decrease in isometric knee extension muscle strength on the operated and nonoperated sides. Previous studies reported that the PhA decreased with age and was positively correlated with lower limb muscle strength in community-dwelling older adults or patients with knee or hip osteoarthritis [19, 21, 22]. Moreover, the PhA was significantly associated with knee extensor strength, independent of age and BMI, in inpatients with cardiovascular disease [20]. Therefore, a decrease in the PhA as a biomarker of a decrease in muscle quality is becoming increasingly recognized [15, 30]. From our results, the decrease in the PhA in patients with hip fractures will also contribute to muscle weakness owing to low muscle quality. The PhA may be increased by short-term resistance training [31, 32]. Therefore, resistance training may improve the PhA, thereby resulting in improved knee extension strength in patients with hip fractures. Furthermore, a significant implication of this study is that the PhA is lower than the previously reported PhAs with higher mortality in community-dwelling older adults and patients with knee or hip osteoarthritis. Lower PhA is associated with higher mortality [33, 34]. Specifically, previous studies reported that the mortality of patients with cardiorenal diseases who had PhAs of 3.6°–4.2° was higher than that of patients who had PhAs of 4.3° or higher [35]. Similarly, the mortality of community-dwelling older adults who had PhAs of 3.5° or less was higher than that of older adults who had PhAs of 3.6° or higher [35]. In our study, the average PhAs was 3.3° and 3.6° on the operated and nonoperated sides, respectively. The PhA in this study was similar to or lower than the values associated with higher mortality in previous studies [36]. Patients with hip fractures have a high mortality rate of approximately 10% and 25% at 1 and 10 years postoperatively, respectively [36]. Therefore, patients with hip fractures should continue resistance training after hospital discharge, and a period may be necessary even after at least 6 months postoperatively. Continued exercise therapy, including resistance training, may increase the PhA and decrease mortality. However, these possibilities were not investigated in this study, and further study is needed.
This study had some limitations. First, we could not measure the PhA of a specific muscle. In this study, the PhA of the lower limbs was measured. While this method is simple, it cannot target specific muscles. Specific muscle quality assessments include intramuscular fat content. In the future, it is necessary to include the amount of intramuscular fat in the quadriceps muscles. Lastly, we could not measure the swelling after a fracture. This study may overestimate muscle mass because of postoperative swelling, which may introduce some bias in this result. However, this study included patients with hip fractures at approximately 6 months postoperatively, and it is likely that several patients would not have swelling.
In conclusions, the results of our study revealed that the decrease in isometric knee extension muscle strength on the operated and nonoperated sides in patients with hip fractures at approximately 6 months postoperatively was associated with not only a decrease in skeletal muscle mass but also a decrease in muscle quality, characterized by a decreased PhA. Therefore, to improve muscle strength in patients with hip fractures at approximately 6 months postoperatively, it is necessary to improve not only muscle mass but also muscle quality.
Data availability
None.
Code availability
None.
References
Dyer SM, Crotty M, Fairhall N, Magaziner J, Beaupre LA, Cameron ID, Sherrington C, Fragility Fracture Network Rehabilitation Research Special Interest G (2016) A critical review of the long-term disability outcomes following hip fracture. BMC Geriatr 16:158
Madsen OR, Lauridsen UB, Sorensen OH (2000) Quadriceps strength in women with a previous hip fracture: relationships to physical ability and bone mass. Scand J Rehabil Med 32:37–40
Kristensen MT, Hulsbæk S, Faber LL, Kronborg L (2021) Knee extension strength measures indicating probable sarcopenia is associated with health-related outcomes and a strong predictor of 1-year mortality in patients following hip fracture surgery. Geriatrics (Basel) 6:8
Nakamura T, Kamiya K, Hamazaki N et al (2021) Quadriceps strength and mortality in older patients with heart failure. Can J Cardiol 37:476–483
Lee J, Han D (2018) Association between knee extensor strength and pulmonary function in the female elderly. J Phys Ther Sci 30:234–237
Pua YH, Clark RA, Bryant AL (2010) Physical function in hip osteoarthritis: relationship to isometric knee extensor steadiness. Arch Phys Med Rehabil 91:1110–1116
Pua YH, Wrigley TV, Collins M, Cowan SM, Bennell KL (2009) Self-report and physical performance measures of physical function in hip osteoarthritis: relationship to isometric quadriceps torque development. Arthritis Rheum 61:201–208
Chen L, Nelson DR, Zhao Y, Cui Z, Johnston JA (2013) Relationship between muscle mass and muscle strength, and the impact of comorbidities: a population-based, cross-sectional study of older adults in the United States. BMC Geriatr 13:74
Wada O, Kurita N, Kamitani T, Nakano N, Mizuno K (2019) Influence of the severity of knee osteoarthritis on the association between leg muscle mass and quadriceps strength: the SPSS-OK study. Clin Rheumatol 38:719–725
Kristensen MT, Bandholm T, Bencke J, Ekdahl C, Kehlet H (2009) Knee-extension strength, postural control and function are related to fracture type and thigh edema in patients with hip fracture. Clin Biomech (Bristol, Avon) 24:218–224
Portegijs E, Rantanen T, Kallinen M, Heinonen A, Alen M, Kiviranta I, Sipilä S (2009) Lower-limb pain, disease, and injury burden as determinants of muscle strength deficit after hip fracture. J Bone Joint Surg Am 91:1720–1728
Mateos-Angulo A, Galán-Mercant A, Cuesta-Vargas AI (2021) Muscle thickness and echo intensity by ultrasonography and cognitive and physical dimensions in older adults. Diagnostics (Basel) 11:1471
Umehara T, Kaneguchi A, Yamasaki T, Katayama N, Kawakami W, Kuwahara D, Kito N (2023) Reduced upper and lower limb muscle strengths without reduced skeletal muscle in elderly patients with heart failure. J Rural Med 18: 8–14
Goodpaster BH, Park SW, Harris TB, Kritchevsky SB, Nevitt M, Schwartz AV, Simonsick EM, Tylavsky FA, Visser M, Newman AB (2006) The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontol A Biol Sci Med Sci 61:1059–1064
Akamatsu Y, Kusakabe T, Arai H et al (2022) Phase angle from bioelectrical impedance analysis is a useful indicator of muscle quality. J Cachexia Sarcopenia Muscle 13:180–189
Kumar S, Dutt A, Hemraj S, Bhat S, Manipadybhima B (2012) Phase angle measurement in healthy human subjects through bio-impedance analysis. Iran J Basic Med Sci 15:1180–1184
Lukaski HC, Kyle UG, Kondrup J (2017) Assessment of adult malnutrition and prognosis with bioelectrical impedance analysis: phase angle and impedance ratio. Curr Opin Clin Nutr Metab Care 20:330–339
Norman K, Stobaus N, Pirlich M, Bosy-Westphal A (2012) Bioelectrical phase angle and impedance vector analysis–clinical relevance and applicability of impedance parameters. Clin Nutr 31:854–861
Yamada Y, Buehring B, Krueger D, Anderson RM, Schoeller DA, Binkley N (2017) Electrical properties assessed by bioelectrical impedance spectroscopy as biomarkers of age-related loss of skeletal muscle quantity and quality. J Gerontol A Biol Sci Med Sci 72:1180–1186
Hirose S, Nakajima T, Nozawa N et al (2020) Phase angle as an indicator of sarcopenia, malnutrition, and cachexia in inpatients with cardiovascular diseases. J Clin Med 9
Wada O, Kurita N, Yamada M, Mizuno K (2020) Structural severity, phase angle, and quadriceps strength among patients with knee osteoarthritis: the SPSS-OK study. Clin Rheumatol 39:3049–3056
Wada O, Yamada M, Kamitani T, Mizuno K, Kurita N (2021) The associations of phase angle with the structural severity and quadriceps strength among patients with hip osteoarthritis: the SPSS-OK study. Clin Rheumatol 40:1539–1546
Katoh M, Isozaki K (2014) Reliability of isometric knee extension muscle strength measurements of healthy elderly subjects made with a hand-held dynamometer and a belt. J Phys Ther Sci 26:1855–1859
Lenzlinger-Asprion R, Keller N, Meichtry A, Luomajoki H (2017) Intertester and intratester reliability of movement control tests on the hip for patients with hip osteoarthritis. BMC Musculoskelet Disord 18:55
Michikawa T, Nishiwaki Y, Takebayashi T, Toyama Y (2009) One-leg standing test for elderly populations. J Orthop Sci 14:675–685
Huang C, Niu K, Kobayashi Y et al (2013) An inverted J-shaped association of serum uric acid with muscle strength among Japanese adult men: a cross-sectional study. BMC Musculoskelet Disord 14:258
Chen LK, Woo J, Assantachai P et al (2020) Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J Am Med Dir Assoc 21(300–307):e302
Umehara T, Kaneguchi A, Kawakami W, Katayama N, Kito N (2022) Association of muscle mass and quality with hand grip strength in elderly patients with heart failure. Heart Vessels 37:1380–1386
Labanca L, Ghislieri M, Knaflitz M, Barone G, Bragonzoni L, Agostini V, Benedetti MG (2021) Muscle synergies for the control of single-limb stance with and without visual information in young individuals. BMC Sports Sci Med Rehabil 13:163
Yamada M, Kimura Y, Ishiyama D et al (2019) Phase angle is a useful indicator for muscle function in older adults. J Nutr Health Aging 23:251–255
Dos Santos L, Cyrino ES, Antunes M, Santos DA, Sardinha LB (2016) Changes in phase angle and body composition induced by resistance training in older women. Eur J Clin Nutr 70:1408–1413
Campa F, Silva AM, Toselli S (2018) Changes in Phase Angle and Handgrip Strength Induced by Suspension Training in Older Women. Int J Sports Med 39:442–449
Thibault R, Makhlouf AM, Mulliez A et al (2016) Fat-free mass at admission predicts 28-day mortality in intensive care unit patients: the international prospective observational study Phase Angle Project. Intensive Care Med 42:1445–1453
Wirth R, Volkert D, Rösler A, Sieber CC, Bauer JM (2010) Bioelectric impedance phase angle is associated with hospital mortality of geriatric patients. Arch Gerontol Geriatr 51:290–294
Garlini LM, Alves FD, Ceretta LB, Perry IS, Souza GC, Clausell NO (2019) Phase angle and mortality: a systematic review. Eur J Clin Nutr 73:495–508
Guzon-Illescas O, Perez Fernandez E, CrespíVillarias N, Quirós Donate FJ, Peña M, Alonso-Blas C, García-Vadillo A, Mazzucchelli R (2019) Mortality after osteoporotic hip fracture: incidence, trends, and associated factors. J Orthop Surg Res 14:203
Acknowledgements
We would like to thank the members of the Osteoporosis Team, Department of Rehabilitation, Kure Kyosai Hospital and Saiseikai Kure Hospital, for their support in data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study had been approved by the Kure Kyosai Hospital (approval number: 21–23) and Hiroshima International University (approval number: 21–043).
Consent to participate
All patients provided written informed consent.
Consent for publication
All patients provided written informed consent.
Conflicts of interest
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Umehara, T., Kaneguchi, A., Watanabe, K. et al. Not only muscle mass but also muscle quality is associated with knee extension muscle strength in patients with hip fractures. Arch Osteoporos 18, 54 (2023). https://doi.org/10.1007/s11657-023-01251-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-023-01251-9