Abstract
Summary
The current study explored the possible utilization in dual-X-ray-absorptiometry scanning (DXA) of the ultra-distal radius (UDR). This region of interest is currently unused and mostly unstudied in this context. The study findings suggest UDR as potential useful region of interest in DXA scanning and warrant further study of the site.
Purpose
Bone mineral density (BMD) measurement of a non-dominant arm is not routinely performed during dual-X-ray-absorptiometry (DXA) test, and the possible utility of ultra-distal (UDR) radius BMD is not well-studied. We evaluated in women, correlations of UDR BMD with fracture prevalence, fracture risk prediction by the fracture risk assessment tool (FRAX), and osteoporosis diagnosed by traditional sites.
Methods
Women who underwent a routine DXA (including their non-dominant forearm and including UDR BMD) in a tertiary medical center were included. Risk factors relevant to FRAX calculation were assessed via a self-administered questionnaire. Spearman correlations of UDR BMD to 10-year risks of major osteoporotic and hip fractures (assessed by FRAX) were explored. The possible added value of UDR BMD in explaining prevalent osteoporotic fractures was assessed using a multivariable regression model incorporating age and traditional osteoporosis diagnosis.
Results
The study included 1245 women with a median age of 66 years (interquartile range: 59–73), of whom 298 (24%) had UDR T-score ≤ − 2.5 and 154 (12%) reported prior fractures. UDR BMD was significantly negatively correlated with FRAX risk score for hip and major osteoporotic fractures (R = − 0.5 and R = − 0.41, respectively; P < 0.001). UDR T-score ≤ − 2.5 was associated with higher fracture prevalence (19% vs 10%; P < 0.001) and remained significant after adjusting for traditional BMD and age (OR 1.49, 1.01–2.19; P = 0.043).
Conclusion
UDR BMD correlates both with prior fractures and with predicted fracture risks and might pose added value over traditional DXA sites.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a significant and growing public health concern, with vast impact on quality and quantity of life, as well as medical, social, and economic implications [1]. Current estimates suggest that at least one in three women and one in six men will have osteoporotic fractures during their lifetime [2]. Bone mineral density (BMD) testing by dual-energy X-ray absorptiometry (DXA) is a major tool in osteoporosis diagnosis and fracture risk assessment in a variety of clinical conditions [3]. The major regions of interest (ROI) for osteoporosis diagnosis include the lumbar spine, the total hip, and the femoral neck. Under certain circumstances, forearm measurement is recommended, and 1/3 radius is the ROI assessed, while the ultra-distal radius (UDR) is not utilized even when available [3]. Osteoporosis is diagnosed if the T-score is − 2.5 or less [3]. However, as more than half of fractures occur in individuals with T-scores above the threshold of − 2.5, additional diagnostic methods are needed [4, 5]. The UDR ROI is centered at a distance of 4–5% of the ulnar length and is composed of 66% trabecular bone [6]. The latter is similar to the spine, although the UDR possesses a higher content of fatty marrow than does the axial skeleton [7]. Only a few studies evaluated the utility of the UDR compared to traditional ROIs for osteoporosis diagnosis. The UDR was shown to yield a significantly higher proportion of persons diagnosed with osteoporosis [8] and greater sensitivity in detecting osteoporosis among women with a recent radius fracture [9]. UDR BMD was found to correlate better than femoral neck BMD to peripheral indices of bone health such as volumetric BMD and microstructure of the radius and the tibia, as measured by high-resolution peripheral quantitative computed tomography (HRpQCT) [5]. In addition, areal UDR BMD explained more than 50% of the variability in strain measurements as assessed by finite element models derived from HRpQCT [10]. Furthermore, the addition of UDR areal BMD to a multivariable model that included peripheral indices of bone health attenuated the ability of these indices in predicting fractures [5].
The aim of the current study was to evaluate correlations of UDR BMD with fracture prevalence, fracture risk prediction by the fracture risk assessment tool (FRAX), and diagnosis of osteoporosis by traditional sites in an unbiased sample of women.
Methods
This retrospective cross-sectional study included women who underwent routine DXA during 2016–2017 in Sheba Medical Center, a tertiary center. The DXA scans were obtained using Lunar Prodigy Advance (1RPA + 130,752; GE healthcare) in concordance with guidelines of the International Society of Clinical Densitometry [3]. Lumbar spine, right and left femoral neck, mean total hip, and forearm measurements were retrieved. The non-dominant forearm scan is routinely measured in our center. Osteoporosis was diagnosed as a T-score ≤ − 2.5 in traditional central sites (spine, femoral neck, and total femur), compared to the women’s reference database for all sites (traditional osteoporosis), in accordance with the current guidelines [3]. For the purpose of statistical analysis, a cutoff of UDR T-score ≤ − 2.5 was predefined as a possible clinically meaningful low BMD of the UDR, in accordance with well-established norms from other ROIs [1, 3, 11]. The trabecular bone score (TBS) was calculated using the TBS iNsight software calibrated for the specific DXA device [12]. Risk factors for FRAX calculation were assessed via a self-administered questionnaire before the test. FRAX scores for hip and major osteoporotic fracture (MOF) were calculated with and without TBS adjustment using the Israel-specific model for each patient.
Descriptive statistics were generated to compare women with and without osteoporotic BMD based on the UDR. The mean UDR T-scores were compared using T-test between women with higher and lower TBS scores. The exact binomial test was used to derive confidence intervals for the proportions of reclassified women by using ultra-distal measurements. The relationship between ultra-radius T-score and various FRAX scores (hip and major osteoporotic fractures, TBS-adjusted and unadjusted) was summarized numerically by Spearman’s correlation coefficient and visually via locally weighted scatterplot smoothing curves (LOWESS). Logistic regression was used to estimate unadjusted OR of previous fractures. Multivariable logistic regression models were used to detect the added value of UDR BMD after adjusting for additional correlates of prior fractures.
The analysis was conducted using R version 4.1.0 (R Foundation for Statistical Computing).
The study was approved by Sheba Medical Center Institutional Review Board.
Results
A total of 1245 women were included in the study; of them, 298 had UDR T-score ≤ − 2.5 Characteristics of the included women are presented in Table 1, according to UDR T-scores. Compared to women with higher UDR T-scores, those with lower scores were older (median age 71 vs 64 years; P < 0.001), had lower BMI (24.7 vs 27.0 kg/m2; P < 0.001), and had lower median TBS (1.265 vs 1.290; P < 0.001). The two groups did not differ significantly in rates of prior glucocorticoid treatment or current smoking, and none of the women reported significant alcohol consumption or had a former diagnosis of rheumatoid arthritis.
Women with TBS score < 1.3 (n = 666) had significantly lower mean UDR T-score compared with women (n = 589) with TBS score ≥ 1.3 − 1.38 vs − 0.96; P < 0.001.
A total of 440 (35%) women were diagnosed with osteoporosis according to traditional sites (spine, femoral neck, and total femur). The usage of the UDR T-score ≤ − 2.5 cutoff would have reclassified 117 more women with osteoporosis.
Overall, 154 (12%) women reported prevalent fractures; the prevalence was significantly higher among those with UDR T-score values ≤ − 2.5 than among those with higher scores (19% vs 10%; P < 0.001) (Table 1, Fig. 1). The prevalence of fractures in 440 patients with classic site osteoporosis (lumbar spine, femoral neck, total femur) was 17% (75 patients reported fractures). The prevalence of fractures in 117 patients with UDR-only osteoporosis was 15.3% (18 patients with prevalent fractures). Summing up, the prevalence of fractures in patients classified as osteoporotic by both the classic sites and UDR was 16.6% (93 fractures in 557 patients).
Among the 154 women with prevalent fractures, 75 (49%) were diagnosed with osteoporosis using traditional central BMD sites (Table 2). Considering a UDR T-score ≤ − 2.5 would have added 18 women, an increase of 24%.
According to measurements at the traditional central BMD sites, enhanced by measurement of the 1/3 radius (Table 2), 97 women (63%) met the criteria for osteoporosis. Considering UDR T-score ≤ − 2.5 would have added 8 diagnoses, an increase of 5% (P value < 0.001) so 105 (68%) of the 154 would have diagnosis of osteoporosis.
In a univariable analysis (Table 3), UDR-based osteoporotic BMD was associated with a significantly higher odds ratio (OR) for prevalent fractures (OR = 2.07, CI 1.44–2.95; P value < 0.001), while the OR for traditional BMD was 1.89 (1.34–2.65; P < 0.001). In a multivariable model (Table 2), both traditional and UDR-based BMD retained their significance (ORs: 1.61 and 1.77, respectively; P values: 0.01 and 0.003, respectively). This suggests added value of UDR BMD over traditional ROI sites of osteoporosis diagnosis. When examined in a multivariable model including age, the ORs were somewhat attenuated for both traditional BMD (OR = 1.53) and UDR-based BMD (OR = 1.49), although statistical significance was retained.
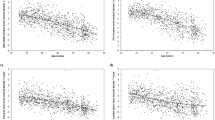
We further examined the correlation between UDR T-score and FRAX score as a surrogate marker for hip fracture and MOF risk. Correlation was examined for FRAX with and without adjustment for TBS in a nonlinear model. UDR T-score was significantly correlated with 10-year FRAX risk score for femoral fracture, with and without TBS adjustment (R = − 0.48 and − 0.5, respectively; P < 0.001 for both) (Fig. 2).
Correlation between ultra-distal radius T-score and the fracture risk assessment tool (FRAX) risk score for hip fractures, without adjustment for trabecular bone score (TBS) (A) and with TBS adjustment (B), and the FRAX risk score for major osteoporotic fractures, without TBS adjustment (C) and with TBS adjustment (D)
The UDR T-score was also significantly correlated with the 10-year FRAX risk score for MOF, with and without TBS adjustment (R = − 0.4 and − 0.4, respectively; P < 0.001 for both).
Discussion
The current study demonstrated a possible role for UDR BMD in bone health evaluation. Several considerations need to be mentioned while discussing forearm measurement as part of the DXA test. On the one hand, the assessment does not require special add-on equipment and can be performed in unique subgroups of patients, e.g., severely obese [3]. On the other hand, since forearm measurement is not considered routine in most centers, the know-how on acquisition and analysis might be suboptimal. This is especially troubling, since optimal adherence to DXA quality control in general is lacking and errors are common [13]. Adding forearm to a routine DXA protocol prolongs the duration of the examination with the extra costs that accompany it. Moreover, the movement artifacts are not uncommon in forearm BMD measurements. It is possible that those technical limitations have precluded a more widespread use of forearm BMD testing. It was though suggested as a cost-effective triage in developing countries with limited availability of central DXA [14]. A more accurate and available densitometric diagnosis of osteoporosis might increase the proportion of women receiving appropriate therapy [15, 16] and also reverse the declining rates of diagnosis and treatment [17].
Previously, our group has demonstrated an added value of 1/3 radius for the diagnosis of osteoporosis by spine and hip sites and its correlation with prevalent fractures and predicted fracture risk [18]. In the current analysis, we showed that accounting for UDR T-scores also led to a significantly higher proportion of women reclassified as having osteoporosis, which is in line with a former study combining data from three sites in the USA [8].
To examine the potential of UDR BMD to identify women with fractures, we evaluated correlations of UDR BMD with fracture prevalence and with FRAX as surrogate measures for fracture prediction. A higher prevalence of fracture was found among women with lower UDR T-scores, even after accounting for traditional ROIs in a multivariable model. This suggests a possible added value of UDR BMD in identifying bone fragility. Moreover, UDR BMD was significantly correlated with FRAX scores (both with and without TBS adjustment). These results are in accordance with a recently published study that demonstrated strong correlations between various radial segments (UDR included) and a diagnosis of osteoporosis according to central sites and especially between UDR BMD and TBS [19]. TBS represent a gray‐level textural score that can be extracted from the DXA lumbar spine image, a predominantly trabecular site, as is UDR.
The predictive value of UDR BMD and fractures was not extensively studied in the past. Case control studies that evaluated the usage of UDR BMD in individuals after Colles’ fracture hypothesized that direct evaluation of the fracture site might be more efficacious than traditional DXA in predicting fracture in the same site. One study demonstrated a uniformly lower UDR BMD in women after fracture in all age groups, while older patients with Colles’ fracture had similar BMD in the spine and hip as the control group of women without Colles’ fracture [20]. This finding was further strengthened by another case control study showing a significantly lower BMD only at radial sites, among women after Colles’ fracture compared with a control group of women without Colles’ fracture [9]. That study also demonstrated a correlation between volumetric bone mineral density and UDR DXA, perhaps explaining the findings. A large prospective study evaluated the predictive fracture value of volumetric BMD and peripheral microstructure elements. In that study, UDR BMD was found to be highly correlated with volumetric BMD and microstructure bone elements. Adjustment to UDR BMD attenuated the effect, suggesting the possibility that UDR BMD measured by DXA could substitute HRpQCT analysis [5].
Also of interest is the treatment effect of antifracture therapy on UDR DXA and thus the possible utility of UDR BMD in monitoring therapy. In a study comparing 1-year therapy with alendronate in women with Colles’ fracture, the UDR BMD showed significantly greater improvement compared with other ROI sites including the trabecular bone (spine) and the cortical bone (1/3 radius, total radius, and femoral neck) [21]. A treatment effect of anabolic drugs was examined in the ACTIVE and ACTIVExtend trials, in which treatment with abaloparatide showed greater improvement in UDR BMD than did teriparatide or placebo; the effect persisted with subsequent oral bisphosphonate therapy [22, 23]. Those studies raise a possible role of the highly metabolically active UDR to monitor the treatment effect of antifracture therapy. It should be emphasized that currently, the usage of UDR BMD is not recommended to establish a diagnosis of osteoporosis or to monitor treatment effect.
Our study has several limitations. First, its retrospective design did not enable follow-up of the women for incident fractures, while the main goal of measuring DXA is to identify persons at the highest risk for fracture incidence. To overcome this limitation, we used fracture prevalence and FRAX score as surrogate measures, yet their accuracy is imperfect. We did not exclude from the cohort women who received prior antifracture treatment, which may have a differential effect on the various ROIs. Lastly, as UDR microstructure differs between the sexes and is affected differentially by aging [24, 25], our findings are not applicable to men.
In summary, UDR DXA might pose a promising addition to bone health evaluation. Further studies in large prospective cohorts capturing fracture incidence are needed to establish the reliability and proper use of UDR in the diagnosis and monitoring of osteoporosis.
Data Availability
Data will be available upon request.
References
Camacho PM, Petak SM, Binkley N et al (2020) American Association of Clinical Endocrinologists/American College of Endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis- 2020 update executive summary. Endocr Pract 26:564–570. https://doi.org/10.4158/GL-2020-0524
Kanis JA, Norton N, Harvey NC et al (2021) SCOPE 2021: a new scorecard for osteoporosis in Europe. Arch Osteoporos. https://doi.org/10.1007/s11657-020-00871-9
ISCD (2019) 2019 ISCD Official Positions – Adult. https://iscd.org/wp-content/uploads/2021/09/2019-Official-Positions-Adult-1.pdf
Schuit SCE, Van Der Klift M, Weel AEAM et al (2004) Fracture incidence and association with bone mineral density in elderly men and women: the Rotterdam study. Bone. https://doi.org/10.1016/j.bone.2003.10.001
Biver E, Durosier-Izart C, Chevalley T et al (2018) Evaluation of radius microstructure and areal bone mineral density improves fracture prediction in postmenopausal women. J Bone Miner Res 33:328–337. https://doi.org/10.1002/jbmr.3299
Bonnick S Lou, Miller P (2013) Clinical use of bone densitometry. Osteoporos Fourth Ed. https://doi.org/10.1016/B978-0-12-415853-5.00066-2
Compston JE (2002) Bone marrow and bone: a functional unit. J Endocrinol. https://doi.org/10.1677/joe.0.1730387
Kiebzak GM, Lewiecki EM, Petak SM (2004) Impact of using the ultradistal radius region of interest on diagnostic classification. J Clin Densitom. https://doi.org/10.1385/JCD:7:2:143
Miyamura S, Kuriyama K, Ebina K et al (2020) Utility of distal forearm DXA as a screening tool for primary osteoporotic fragility fractures of the distal radius. JBJS Open Access. https://doi.org/10.2106/jbjs.oa.19.00036
Mancuso ME, Johnson JE, Ahmed SS et al (2018) Distal radius microstructure and finite element bone strain are related to site-specific mechanical loading and areal bone mineral density in premenopausal women. Bone Rep 8:187–194. https://doi.org/10.1016/j.bonr.2018.04.001
Eastell R, Rosen CJ, Black DM et al (2019) Pharmacological management of osteoporosis in postmenopausal women: an endocrine society* clinical practice guideline. J Clin Endocrinol Metab. https://doi.org/10.1210/jc.2019-00221
Martineau P, Silva BC, Leslie WD (2017) Utility of trabecular bone score in the evaluation of osteoporosis. Curr Opin Endocrinol Diabetes Obes 24:402–410. https://doi.org/10.1097/MED.0000000000000365
Jones A, Goh M, Milat F et al (2021) Dual energy X-ray absorptiometry reports fail to adhere to international guidelines. J Clin Densitom 24:453–459. https://doi.org/10.1016/J.JOCD.2020.10.002
Kruger IM, Kruger MC, Doak CM, Kruger A (2012) Cut-off values of distal forearm bone density for the diagnosis of central osteoporosis in black postmenopausal South African women. J Endocrinol Metab Diabetes S Afr. https://doi.org/10.1080/22201009.2012.10872281
Nayak S, Greenspan SL (2018) How can we improve osteoporosis care? A systematic review and meta-analysis of the efficacy of quality improvement strategies for osteoporosis. J Bone Miner Res. https://doi.org/10.1002/jbmr.3437
Fitt NS, Mitchell SL, Cranney A et al (2001) Influence of bone densitometry results on the treatment of osteoporosis. CMAJ 164:777–781
Miller PD (2016) Underdiagnoses and undertreatment of osteoporosis: the battle to be won. J Clin Endocrinol Metab. https://doi.org/10.1210/jc.2015-3156
Tripto-Shkolnik L, Vered I, Peltz-Sinvani N et al (2021) Bone mineral density of the 1/3 radius refines osteoporosis diagnosis, correlates with prevalent fractures, and enhances fracture risk estimates. Endocr Pract. https://doi.org/10.1016/j.eprac.2020.12.010
Gautam KP, Cherian KE, Kapoor N et al (2022) Utility and validation of bone mineral density measurements at forearm in predicting trabecular microarchitecture and central-site osteoporosis in aging Indian postmenopausal women—a promising surrogate? Aging Med. https://doi.org/10.1002/agm2.12191
Kanterewicz E, Yañez A, Pérez-Pons A et al (2002) Association between Colles’ fracture and low bone mass: age-based differences in postmenopausal women. Osteoporos Int. https://doi.org/10.1007/s001980200114
Van Der Poest Clement E, Patka P, Vandormael K et al (2000) The effect of alendronate on bone mass after distal forearm fracture. J Bone Miner Res. https://doi.org/10.1359/jbmr.2000.15.3.586
Watts NB, Dore RK, Baim S et al (2021) Forearm bone mineral density and fracture incidence in postmenopausal women with osteoporosis: results from the ACTIVExtend phase 3 trial. Osteoporos Int. https://doi.org/10.1007/s00198-020-05555-1
Watts NB, Hattersley G, Fitzpatrick LA et al (2019) Abaloparatide effect on forearm bone mineral density and wrist fracture risk in postmenopausal women with osteoporosis. Osteoporos Int. https://doi.org/10.1007/s00198-019-04890-2
Khosla S, Riggs BL, Atkinson EJ et al (2006) Effects of sex and age on bone microstructure at the ultradistal radius: a population-based noninvasive in vivo assessment. J Bone Miner Res. https://doi.org/10.1359/JBMR.050916
Choksi P, Jepsen KJ, Clines GA (2018) The challenges of diagnosing osteoporosis and the limitations of currently available tools. Clin Diabetes Endocrinol. https://doi.org/10.1186/s40842-018-0062-7
Acknowledgements
The researchers wish to thank Mr. Nimrod Tripto for his contribution to the data analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Schwarz, Y., Goldshtein, I., Friedman, Y.E. et al. Bone mineral density of the ultra-distal radius: are we ignoring valuable information?. Arch Osteoporos 18, 28 (2023). https://doi.org/10.1007/s11657-023-01218-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-023-01218-w