Abstract
Summary
The Taiwan FRAX® calculator was validated to predict incident fractures preliminarily. Cutoffs of FRAX probability for predicting major osteoporotic fracture and hip fracture were proposed as 9.5% and 4% in Taiwanese individuals.
Purpose
FRAX® is an algorithm used to calculate fracture probabilities based on clinical risk factors (CRFs) and bone mineral density (BMD). The country-specific Taiwan FRAX calculator has not been validated since its establishment in 2010. The aim of the present study is to evaluate the predictive performance of the Taiwan FRAX calculator using longitudinal fracture data.
Methods
A total of 1975 subjects, aged ≧ 40 years old, from Yunlin and Tianliao cohorts in Taiwan during the period 2009–2010, were identified and completely connected with the 2008–2016 National Health Insurance Research Database.
Results
During the average 6.8 ± 1.1 years of follow-up, 160 incident major osteoporotic fractures (MOFs) were identified. The predictive ability assessing based on the observed to expected fractures (O/E) ratio calculated with the FRAX probability adjusted for 6.8 years were 1.19 (95%CI 1.02–1.39) for MOF, and 1.07 (95%CI 0.82–1.39) for hip fractures. In the discriminative statistics, the AUC for prediction of major osteoporotic fractures using FRAX was 0.75 without and 0.77 with BMD (AUC for hip fracture was 0.75 without and 0.77 with BMD). The optimal cutoff value was 9.5% of the FRAX score with BMD for all major osteoporotic fractures, with good sensitivity (76.9%) and specificity (65.3%). For hip fractures, the optimal cutoff point for the FRAX probability with BMD was 4.0%, and the sensitivity and specificity were 74.4% and 68.3%, respectively.
Conclusion
The Taiwan FRAX® calculator was validated to predict incident fractures preliminarily. Cutoffs are proposed for predicting fracture risk in Taiwanese individuals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approximately 10 million US adults aged 50 or more have osteoporosis, and an additional 33 million have low bone mass based on femoral neck bone mineral density [1]. The prevalence of osteoporosis-related fractures during the lifetime is 15–30% in white Caucasian males and 30–50% in white females [2]. In Taiwan, an analysis from Nationwide Health Insurance Research Database (NHIRD) revealed the average prevalence of osteoporosis in those aged ≧50 years was underestimated to be 1.63% for men and 11.35% for women [3]. Another study recruiting adults undergoing health examination showed the prevalence of osteoporosis was 18.5% [4]. However, in Asia–Pacific regions, osteoporotic hip fractures are projected to increase 2- to threefold between 2018 and 2050 [5], and Taiwan leads the Asia–Pacific region in the incidence of osteoporotic hip fractures [6].
FRAX® (fracture risk assessment tool) is an algorithm that can be used to calculate age- and gender-specific fracture probabilities from obtained clinical risk factors (CRFs) and bone mineral density (BMD) [7]. In fact, the CRFs for fracture, including age, sex, body mass index, history of fragility fracture, family history of fracture, smoking status, alcohol intake, use of oral glucocorticoid, rheumatoid arthritis, and other causes of secondary osteoporosis, were identified based on serial meta-analyses of substantial population-based cohorts [8, 9]. The country-specific Taiwanese FRAX model was derived from incorporating the National mortality data and hip fracture incidence in 1996–2002 with the backbone FRAX model of 12 cohorts and launched since 2010 [10]; however, large prospective cohort studies are needed to validate this country-specific model. The aim of this study is to evaluate the predictive performance of the Taiwan FRAX calculator using longitudinal fracture data.
Methods
Participants
After excluding one subject with incomplete follow-up data, we studied 1975 subjects (M/F = 932/1043), aged 40 years old and over, from 2 concomitant cohorts established in different regions of Taiwan during the period 2009–2010 [11]. One cohort recruited subjects aged 40 and above from Yunlin County in middle Taiwan [12]. Another cohort in Tianliao District of southern Taiwan recruited men and woman aged 65 or more [13,14,15,16,17]. The inclusion criteria are as follows: subjects who (1) aged 40 or more at baseline BMD assessment; (2) had complete data of FRAX CRFs and probability estimates (with and without BMD); (3) had medical coverage from Taiwan’s National Health Insurance Research Database (NHIRD) during the observation period from 2008 to 2016.
Among the 1200 subjects in the Yunlin cohort (males = 524; females = 676, average age = 59.6 ± 11.4 years old), the prevalences of osteoporosis diagnosed using DXA (dual-energy X-ray absorptiometry) in men and women were 40.2% and 41.0%, respectively [12]. In another elderly cohort, the Tianliao cohort recruiting 775 subjects (male = 408; female = 367, average age = 74.2 ± 6.1 years old), the prevalences of osteoporosis were found to be 18.1% in men and 60.4% in women [13, 14]. This study was approved by the Institutional Review Board of the National Cheng Kung University Hospital.
Measures and questionnaires
During enrollment, the lumbar and hip BMD of the study participants were measured using dual-energy X-ray absorptiometry (DXA, Prodigy, GE Lunar, USA, in Yunlin and Explorer, Hologic, USA, in Tianliao) [11]. Structured questionnaires were administered at the baseline to collect information on CRFs [15, 16]. Habitual smoking and high consumption of alcohol were defined as stipulated by the FRAX [17]. Information on rheumatoid arthritis and secondary osteoporosis were obtained by taking histories. Glucocorticoid exposure was documented according to the FRAX definitions [7].
The National Health Insurance (NHI) of Taiwan, a globally unique program in force since 1995, manages more than 99.9% of the medical claims data of all citizens, keeping records in the National Health Insurance Research Database (NHIRD) [18]. This database currently provided by Health and Welfare Data Science Center, Ministry of Health and Welfare (HWDC, MOHW), has been used as an important source of data for evidence-based studies in Taiwan. All of the participants in the present study were included in Taiwan’s NHIRD at some point during our observation period (2008 to 2016). We merged the basic demographic data of the study participants enrolled in the Yunlin and Tianliao cohorts, and subsequently confirmed the fracture rates using Taiwan’s NHIRD. The fracture outcomes observed up to December 31, 2016, were documented according to the ICD codes from Taiwan’s NHIRD. We identified all claims records of hospital admissions of patients from 2009 to 2016 in the NHIRD data after exclusion of trauma-relevant events (ICD-9-CM E800-E879 and E890-E99). Specific ICD-9 codes between 2009 and 2015 and ICD-10 codes after 2016 were used to identify osteoporosis-related fractures, including hip, distal radius, humerus, spine and osteoporotic fractures [11]. The accuracy of diagnosis of fracture had been endorsed [19]. The cumulative incidences of osteoporotic hip fracture and other major osteoporotic fractures (MOFs) at the end of follow-up were obtained. Patients were followed from the examination date in 2009 ~ 2010 until the fracture or until December 31, 2016.
Statistical methods
Data were analyzed using SAS 9.4 software. Intergroup comparisons of basic demographic data for the two cohorts were carried out using a Pearson’s chi-square analysis for categorical variables and Student’s t-test for continuous variables. The primary outcome was the first diagnosis of an osteoporotic hip fracture or other major osteoporotic fractures (including hip, vertebral, upper arm, or wrist). In an attempt to redefine the high-risk group for osteoporotic fracture prediction, the predictive ability of FRAX was assessed by analyzing calibration and discrimination. Predictive ability was assessed by comparing estimated risk fractures with incidence fractures (observed to expected fracture ratios, O/E). Expected fractures were estimated as the sum of the 10-year probability of fracture, referred from a validation study of the Spanish FRAX model conducted on a retrospective cohort of 1231 women aged 40–90 years [20]. Observed fractures were defined as the total number of fractures observed at the end of follow-up (until December 31, 2016). Subjects with recurred fracture at same site were analyzed at the first event. The cumulative incidence and incidence rates of osteoporotic fracture were calculated accordingly [21,22,23,24]. An AUC-ROC (area under the curve of the receiver operating characteristic) analysis was carried out to compare fracture discrimination based on the FRAX score with and without BMD and at different cutoff points. The Youden Index will be used for the suggestion of the optimal cutoff [25].
Results
Basic demographic analysis
In Table 1, compared with the subjects without incident fractures, those with incident fractures were older, shorter, and leaner, and comprised more women. Rationally, subjects with incident fractures had a lower bone mineral density but higher FRAX MOF and hip fracture risk scores and higher T-scores.
Osteoporotic fracture rates
Of the 1975 subjects followed up for an average 6.8 ± 1.1 years, 160 incident MOFs were identified (including 36% hip, 17% distal radius, 7.5% humerus, 45% clinical vertebra and osteoporotic fracture). A total of 18 and 142 fractures occurred in participants aged < 65 and ≥ 65 years, respectively. There were 58 incident hip fractures observed, most of which occurred in elderly individuals 65 years old and above. In this study, the cumulative incidence of all osteoporotic fractures was 8.1%. The incident osteoporotic fracture rates (per 100,000) were 921.2 for men and 1503.5 for women. The incidence rates of hip fracture for Taiwanese men and women (per 100,000) were 403.1 and 466.4, respectively.
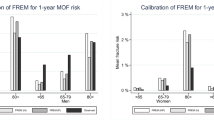
The calibration and discrimination statistics
Table 2 shows the calibration statistics for the Taiwan FRAX model. In terms of major osteoporotic fractures, the predictive ability assessed using the O/E ratio calculated with FRAX with BMD was 0.81 (95% CI 0.69–0.94), and for hip fractures, it was 0.70 (95% CI 0.52–0.88). However, the 10-year FRAX model seemed to overestimate the risk of osteoporotic fracture when utilizing the fracture data with incomplete follow-up time. We further assumed that fracture rates are relatively stable over time, and the estimated hip fractures and MOFs of 6.8 years follow-up time would be 54.02 and 133.95 by interpolation. Consequently, at 6.8 years, the adjusted calibration ratio for hip fracture and MOF would be 1.07 (95%CI 0.82–1.39) and 1.19 (95%CI 1.02–1.39), respectively. Therefore, the calibration performance was improved and even better when referring to hip fracture (Supplementary Table 1). However, in the younger subgroup aged 40–65 years, the FRAX model tended to overestimate the risk of osteoporotic fracture (unadjusted O/E 0.42, 95%CI 0.22–0.61; adjusted O/E 0.61, 95%CI 0.36–0.97) (Table 3 and Supplementary Table 2).
In the ROC analysis, the AUC for the prediction of major osteoporotic fractures using FRAX without BMD was 0.75 (95%CI 0.71–0.79), and using FRAX with BMD was 0.77 (95%CI 0.74–0.80). The results were similar in terms of hip fracture prediction (AUC 0.75 without BMD and 0.77 with BMD). Adding the BMD information in the FRAX model improved the AUC for fracture prediction. Table 4 shows the sensitivity and the specificity of the FRAX score with BMD at different cutoff points for identifying incident osteoporotic fractures. With the BMD information, the optimal cutoff value was 9.5% of the FRAX score for all major osteoporotic fractures, based on the Youden Index, where good sensitivity (76.9%) and specificity (65.3%) were obtained. For hip fractures, the optimal cutoff point for the FRAX probability with BMD was 4.0% based on the Youden Index, and the sensitivity and specificity were 74.4% and 68.3%, respectively. Our study further showed that for the FRAX scored with BMD, the sensitivity/specificity for estimating the risk of MOFs were 76.9%/65.3%, 73.8%/67.3%, 50.0%/82.4%, and 33.1%/91.4%, with cutoffs of 9.5%, 10%, 15%, and 20%, respectively. The sensitivity/specificity for estimating the risk of hip fracture with cutoffs of 1.0%, 1.5%, 3.0%, and 4.0% were 95.6%/27.7%, 91.9%/38.3%, 83.1%/58.5%, and 74.4%/68.3%, respectively. However, when the BMD was not included, the optimal cutoff values were 8.0% for the FRAX score for all major osteoporotic fractures and 4.0% for hip fractures using the Youden Index (Supplementary Table 3).
Discussion
The present study is the first large Taiwanese cohort study to validate the Taiwan FRAX model. The cumulative incidence of all osteoporotic fractures is similar with that of Japan (5.8%), Korea (11.2%), and Hongkong (9.4%) [21,22,23]. The incidence rates of hip fracture for Taiwanese men and women are also consistent with those of Asian populations [24].
The transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD) initiative developed a set of recommendations for the reporting of studies developing, validating, or updating a prediction model. The present report is a prognostic prediction model study regarding prognosis following the rules set forth in the TRIPOD statement [26]. Our results showed that the Taiwan FRAX tool has good discriminatory/predictive ability for detecting both osteoporotic fractures and hip fractures in a Taiwanese population, but may have overestimated in individuals younger than 65 years of age. This phenomenon is contradictory to the Spanish FRAX validation studies, which showed underestimation of fracture probability in younger Spanish subgroups [20, 27]. In addition to validating the present prognostic model, investigations of the impact on clinical practice were also considered under the PROGRESS framework [28].
The majority of publications have identified an intervention threshold probability of 20% for major osteoporotic fracture and 3% for hip fracture [29]. A cross-country meta-analysis including 7 longitudinal cohorts was conducted to assess the diagnostic accuracy of FRAX in predicting incident osteoporotic fractures. When using 20% as the fixed intervention probability for major osteoporotic fractures, the sensitivity and specificity were 10.25% (95%CI 3.76–25.06) and 97.02% (95%CI 91.17–99.03), respectively. For hip fracture prediction, using 3% as the fixed probability threshold, the sensitivity and specificity were 45.70% (95%CI 24.88–68.13) and 84.70% (95%CI 76.41–90.44), respectively [30]. The Osteoporosis Society of Hong Kong documented the NOF (National Osteoporosis Foundation) 20% intervention threshold stated in its current guideline, but no practical instruction on the use of FRAX was given [31]. A Hong Kong Osteoporosis Study applied the NOF (National Osteoporosis Foundation, USA), NOGG (National Osteoporosis Guideline Group, UK), and Taiwanese guidelines to a cohort of 2266 postmenopausal women. During the mean follow-up of 4.5 years, a total of 106 incident osteoporotic fractures were observed, of which 21 were hip fractures. The optimal cutoff point of the 10-year probability of a major fracture was identified as 9.95%, with a sensitivity of 62.3% and a specificity of 73.5% [32]. In China, it was proposed that the intervention thresholds may be 4% for the 10-year probability of major osteoporotic fracture and 1.3% for hip fracture. According to the 37.5% prevalence of osteoporosis found in an epidemiology study of 778 postmenopausal women, the 62.5th percentiles of major osteoporotic fracture and hip fracture probability were 4.0% and 1.3%, respectively [33]. The Japanese guideline adopted 15% as a treatment probability threshold, considering that the 10-year probability of major osteoporotic fracture in the patients receiving pharmacological treatment in clinical settings was observed to be approximately 15% [34]. According to the aforementioned literature, the fixed probability thresholds have ranged from 4 to 20% for a major fracture and from 1.3 to 5% for a hip fracture [35], which is consistent with this report.
When cost-effectiveness was taken into consideration, a Taiwanese study revealed the cutoff of FRAX probability for intervention should be determined as 7% for women and 6% for men for hip fractures and 15% for women and 12.5% for men for MOFs, respectively [36]. In this study, the MOF and hip fracture intervention thresholds were estimated using the Markov model, in which willingness to pay was set at twice the gross domestic product per capita of Taiwan [36]. The relatively higher threshold than in the present study may be a reflection of low medical costs under Taiwan’s NHI reimbursement. Medical costs after fracture are relatively cheap in the consideration of GDP. Thus, the treatment thresholds were elevated concerning cost-effectiveness. This discrepancy may also result from the limitation of the Markov model due to not considering the BMD. On the other hand, discrimination statistic refers to the ability of the risk prediction model to distinguish between patients who experience a fracture and those who do not. The proposed cutoffs in our study were 9.5% and 4.0% for predicting major osteoporotic fracture and hip fracture determined by sensitivity/specificity of AUC-ROC analysis. Our results also revealed that adding the BMD into the FRAX model can improve the predictive performance related to incident fractures. In addition, the present report is the first large Taiwanese prospective cohort study recruiting a target population with fracture outcomes from the national databank after nearly 7 years of follow-up and was intended to validate the Taiwan FRAX model more reliably. There are 215 participants who received anti-osteoporosis treatment during the observation period. The results were proven to be consistent even after adjustment of anti-osteoporotic treatment and physical therapy during the follow-up period [11].
This study still has several limitations. First, all study participants were Taiwanese, which limits generalizability. However, the findings reconfirmed the usefulness of country-specific FRAX model for predicting incident fracture. Second, due to the fact that ICD-10-CM just has been implemented instead of ICD-9 in Taiwan since 2016, ICD-9-CM diagnosis codes were mainly utilized in the present study, which are relatively unspecified in terms of disease classification stakeholders [37]. Therefore, the mechanism of fractures in our study remained unclear using the ICD-9-CM code. Finally, a 6.8-year follow-up may not be able to adequately reflect the 10-year fracture risk precisely. However, a trend in fracture risk was proven and can be reconfirmed in the near future. In addition to validating the Taiwan FRAX model with the data used in the present cohort study, further reconstruction of the Taiwan FRAX model could be considered by either incorporating other important risk factors, such as a history of falls [11, 38, 39], the trabecular bone score [40], spine–hip discordance [41], or reducing the number of existing CRFs.
Conclusions
Our data revealed that the Taiwan FRAX® calculator was validated to predict incident fractures preliminarily. Cutoffs of FRAX probability were proposed as 9.5% and 4.0% for predicting major osteoporotic fracture and hip fracture in Taiwanese individuals, respectively.
Abbreviations
- FRAX:
-
Fracture risk assessment
- BMD:
-
Bone mineral density
- MOF:
-
Major osteoporotic fracture
- CRF:
-
Clinical risk factor
- NHI:
-
National Health Insurance
- NHIRD:
-
National Health Insurance Research Database
References
America’s Bone Health (2002) The state of osteoporosis and low bone mass in our nation. National Osteoporosis Foundation, Washington, DC
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res 22(3):465–475
Yang NP, Deng CY, Chou YJ, Chen PQ, Lin CH, Chou P, Chang HJ (2006) Estimated prevalence of osteoporosis from a Nationwide Health Insurance database in Taiwan. Health Policy 75(3):329–337. https://doi.org/10.1016/j.healthpol.2005.04.009 (Epub 2005 Jun 8)
Yeh C-H, Yeh S-C (2007) Prevalence and risk factors of osteoporosis among adults undergoing health examinations in Southern Taiwan. Taiwan J Public Health 26(6):462–471
Cheung CL, Ang SB, Chadha M, Chow ES, Chung YS, Hew FL, Jaisamrarn U, Ng H, Takeuchi Y, Wu CH, Xia W, Yu J, Fujiwara S (2018) An updated hip fracture projection in Asia: the Asian Federation of Osteoporosis Societies study. Osteoporos Sarcopenia 4(1):16–21. https://doi.org/10.1016/j.afos.2018.03.003
Wu CH, McCloskey EV, Lee JK, Itabashi A, Prince R, Yu W, Li-Yu J, Chionh SB, Zhao Y, Shin CS, Gunawan T, Tsai KS, Chieng PU, Changlai SP, Chan DC, Chen JF, Tanner SB, Hans DB, Kanis JA, Chang YF, Sun ZJ, Yang RS (2014) Consensus of Official Position of IOF/ISCD FRAX Initiatives in Asia-Pacific Region. J Clin Densitom 17(1):150–155. https://doi.org/10.1016/j.jocd.2013.06.002
Kanis JA on behalf of the World Health Organization Scientific Group (2008) Assessment of osteoporosis at the primary healthcare level. Technical report. WHO Collaborating Centre, University of Sheffield, UK.
Kanis JA, Borgstrom F, De Laet C, Johansson H, Johnell O, Jonsson B, Oden A, Zethraeus N, Pfleger B, Khaltaev N (2005) Assessment of fracture risk. Osteoporos Int 16(6):581–589. https://doi.org/10.1007/s00198-004-1780-5
Kanis JA, Johnell O, Oden A, Johansson H, McCloskey E (2008) FRAX™ and the assessment of fracture probability in men and women from the UK. Osteoporos Int 19(4):385–397
Liu IT, Liang FW, Wang ST, Chang CM, Lu TH, Wu CH (2021) The effects of falls on the prediction of osteoporotic fractures: epidemiological cohort study. Arch Osteoporos 16(1):110. https://doi.org/10.1007/s11657-021-00977-8
Ou LC, Sun ZJ, Chang YF, Chang CS, Chao TH, Kuo PH, Lin RM, Wu CH (2013) Epidemiological survey of quantitative ultrasound in risk assessment of falls in middle-aged and elderly people. PLoS ONE 8(8):e71053. https://doi.org/10.1371/journal.pone.0071053
Chao YJ, Chen CY, Wu CF, Chang CS, Kuo PH, Chang HJ, Tu CW, Chang YF, Wu CH (2010) The prevalence of osteoporosis and associated risk factors in elderly females living in a rural community in Taiwan. Taiwan J Fam Med 20(2):64–73
Chen HY, Chang YF, Chang CS, Chen CY, Yang YC, Chen JF, Wu CH (2011) Osteoporosis and status of management in old males lived in rural community. Tw Geriatrics Gerontol 6(2):116–129
Chang CS, Chang YF, Wang MW, Chen CY, Chao YJ, Chang HJ, Kuo PH, Yang YC, Wu CH (2013) Inverse relationship between central obesity and osteoporosis in osteoporotic drug naïve elderly females: the Tianliao Old People (TOP) Study. J Clin Densitom 16(2):204–211. https://doi.org/10.1016/j.jocd.2012.03.008
Chang YF, Chang CS, Wang MW, Wu CF, Chen CY, Chang HJ, Kuo PH, Wu CH (2016) Effects of age and body mass index on thoracolumbar spine X-ray for diagnosing osteoporosis in elderly women: Tianliao Old People (TOP) Study 07. PLoS ONE 11(9):e0161773. https://doi.org/10.1371/journal.pone.0161773
Chang CS, Chang YF, Liu PY, Chen CY, Tsai YS, Wu CH (2012) Smoking, habitual tea drinking and metabolic syndrome in elderly men living in rural community: the Tianliao Old People (TOP) Study 02. PLoS ONE 7(6):e38874. https://doi.org/10.1371/journal.pone.0038874
National Health Insurance Administration, Ministry of Health and Welfare, Taiwan, R.O.C. (2014) National Health Insurance Annual Report 2014–2015.
Fu SH, Wang CY, Hung CC, Lee CC, Yang RS, Huang CC, Farn CJ, Lin WH, Chen HM, Hsiao FY, Lin JW, Li CY (2021) Increased fracture risk after discontinuation of anti-osteoporosis medications among hip fracture patients: a population-based cohort study. J Intern Med 290(6):1194–1205. https://doi.org/10.1111/joim.13354 (Epub 2021 Aug 2)
Tebé Cordomí C, Del Río LM, Di Gregorio S, Casas L, Estrada MD, Kotzeva A, Espallargues M (2013) Validation of the FRAX predictive model for major osteoporotic fracture in a historical cohort of Spanish women. J Clin Densitom 16(2):231–237. https://doi.org/10.1016/j.jocd.2012.05.007 (Epub 2012 Jun 29)
Tamaki J, Iki M, Kadowaki E, Sato Y, Kajita E, Kagamimori S, Kagawa Y, Yoneshima H (2011) Fracture risk prediction using FRAX(R): a 10-year follow-up survey of the Japanese Population-Based Osteoporosis (JPOS) Cohort Study. Osteoporos Int 22:3037–3045
Jang EJ, Lee YK, Choi HJ, Ha YC, Jang S, Shin CS, Cho NH (2016) Osteoporotic fracture risk assessment using bone mineral density in Korean: a community-based cohort study. J Bone Metab 23:34–39
Su Y, Leung J, Kwok T (2018) The role of previous falls in major osteoporotic fracture prediction in conjunction with FRAX in older Chinese men and women: the Mr. OS and Ms. OS cohort study in Hong Kong. Osteoporos Int 29:355–363
Lau EM, Lee JK, Suriwongpaisal P, Saw SM, De Das S, Khir A, Sambrook P (2001) The incidence of hip fracture in four Asian countries: the Asian Osteoporosis Study (AOS). Osteoporos Int 12(3):239–243. https://doi.org/10.1007/s001980170135
Youden WJ (1950) Index for rating diagnostic tests. Cancer 3(1):32–35. https://doi.org/10.1002/1097-0142(1950)3:1%3c32::aid-cncr2820030106%3e3.0.co;2-3
Collins GS, Reitsma JB, Altman DG, Moons KG (2015) Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMJ 350:g7594. https://doi.org/10.1136/bmj.g7594
Azagra R, Zwart M, Encabo G, Aguyé A, Martin-Sánchez JC, Puchol-Ruiz N, Gabriel-Escoda P, Ortiz-Alinque S, Gené E, Iglesias M, Moriña D, Diaz-Herrera MA, Utzet M, Manresa JM (2016) Rationale of the Spanish FRAX model in decision-making for predicting osteoporotic fractures: an update of FRIDEX cohort of Spanish women. BMC Musculoskelet Disord 17:262. https://doi.org/10.1186/s12891-016-1096-6
Steyerberg EW, Moons KG, Hayden JA, Perel P, Schroter S, Riley RD, Hemingway H, Altman DG, PROGRESS Group (2013) Prognosis Research Strategy (PROGRESS) 3: prognostic model research. PLoS Med 10(2):e1001381. https://doi.org/10.1371/journal.pmed.1001381 (Epub 2013 Feb 5)
Dawson-Hughes B (2008) National Osteoporosis Foundation Guide Committee. A revised clinician’s guide to the prevention and treatment of osteoporosis. J Clin Endocrinol Metab 93:2463–2465
Jiang X, Gruner M, Trémollieres F, Pluskiewicz W, Sornay-Rendu E, Adamczyk P (2017) Diagnostic accuracy of FRAX in predicting the 10-year risk of osteoporotic fractures using the USA treatment thresholds: a systematic review and meta-analysis. Bone 99:20–25. https://doi.org/10.1016/j.bone.2017.02.008 (Epub 2017 Mar 6)
Ip TP, Cheung SK, Cheung TC, Choi TC, Chow SL, Ho YY, Kan SY, Kung WC, Lee KK, Leung KL, Leung YY, Lo ST, Sy CT, Wong YW; Osteoporosis Society of Hong Kong (2013) The Osteoporosis Society of Hong Kong (OSHK): 2013 OSHK guideline for clinical management of postmenopausal osteoporosis in Hong Kong. Hong Kong Med J 19(Suppl 2):1–40
Cheung E, Kung AWC, Tan KCB (2014) Outcomes of applying the NOF, NOGG and Taiwanese guidelines to a cohort of Chinese early postmenopausal women. Clinl Endocrinol 80:200–207
Zhang Z, Ou Y, Sheng Z, Liao E (2014) How to decide intervention thresholds based on FRAX in central south Chinese postmenopausal women. Endocrine 45:195–197
Orimo H, Nakamura T, Hosoi T, Iki M, Uenishi K, Endo N, Ohta H, Shiraki M, Sugimoto T, Suzuki T, Soen S, Nishizawa Y, Hagino H, Fukunaga M, Fujiwara S (2012) Japanese 2011 guidelines for prevention and treatment of osteoporosis—executive summary. Arch Osteoporos 7(1):3–20. https://doi.org/10.1007/s11657-012-0109-9
Kanis JA, Harvey NC, Cooper C, Johansson H, Odén A, McCloskey EV; Advisory Board of the National Osteoporosis Guideline Group (2016) A systematic review of intervention thresholds based on FRAX: a report prepared for the National Osteoporosis Guideline Group and the International Osteoporosis Foundation. Arch Osteoporos 11(1):25. https://doi.org/10.1007/s11657-016-0278-z (Epub 2016 Jul 27)
Chan DC, McCloskey EV, Chang CB, Lin KP, Lim LC, Tsai KS, Yang RS (2107) Establishing and evaluating FRAX(®) probability thresholds in Taiwan. J Formos Med Assoc 116(3):161–168. https://doi.org/10.1016/j.jfma.2016.03.006
World Health Organization. Classification of Disease (ICD). 2016. Available at: http://www.who.int/classifications/icd/en/
Masud T, Binkley N, Boonen S, Hannan MT, Members FPDC (2011) Official positions for FRAX(R) clinical regarding falls and frailty: can falls and frailty be used in FRAX(R)? From Joint Official Positions Development Conference of the International Society for Clinical Densitometry and International Osteoporosis Foundation on FRAX(R). J Clin Densitom 14:194–204
Ou LC, Chang YF, Chang CS, Chiu CJ, Chao TH, Sun ZJ, Lin RM, Wu CH (2017) Epidemiological survey of the feasibility of broadband ultrasound attenuation measured using calcaneal quantitative ultrasound to predict the incidence of falls in the middle-aged and elderly. BMJ Open 7(1):e013420. https://doi.org/10.1136/bmjopen-2016-013420
Briot K, Paternotte S, Kolta S, Eastell R, Reid DM, Felsenberg D, Glüer CC, Roux C (2013) Added value of trabecular bone score to bone mineral density for prediction of osteoporotic fractures in postmenopausal women: the OPUS study. Bone 57(1):232–236. https://doi.org/10.1016/j.bone.2013.07.040
Leslie WD, Lix LM, Johansson H, Oden A, McCloskey E, Kanis JA (2011) Spine-hip discordance and fracture risk assessment: a physician-friendly FRAX enhancement. Osteoporos Int 22(3):839–847
Acknowledgements
The authors wish to acknowledge the administrative and technical support received from the National Cheng Kung University Hospital Dou-Liou Branch, Yun-Lin county; Tian Liao District Public Health Center, Kaohsiung City; the National Health Insurance Research Database, the Center for Medical Informatics and Statistics, Kaohsiung Medical University, and National Cheng Kung University Hospital. Finally, we are grateful to the Health Data Science Center, the National Cheng Kung University Hospital, for providing administrative and technical support.
Funding
This research was funded by research grants MOST106-2314-B-006–064-MY2 and MOST 108–2314-B-006–043-MY2 from the Ministry of Science and Technology and grants from NCKUH-10909042. This work was also partially supported by research grant DOH-98HP-A9802-6, from the Bureau of Health Promotion, Taiwan.
Author information
Authors and Affiliations
Contributions
Conception and design of the study: ITL, FWL, YFC, CSC, CHW. Statistical analyses: ITL, CHW, CCL, FWL. Research data interpretation: all coauthors. Acquisition of data: YFC, CSC, ZJS, CHW. Suggestions and discussion: THL, CSC. Drafting of the article: ITL, CHW. Critical revision of the manuscript: all coauthors. Final approval of the manuscript: all coauthors.
Corresponding authors
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liu, IT., Liang, FW., Li, CC. et al. Validation of the Taiwan FRAX® calculator for the prediction of fracture risk. Arch Osteoporos 17, 27 (2022). https://doi.org/10.1007/s11657-022-01068-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-022-01068-y