Abstract
Summary
Little is known about factors that lead to excess mortality post-fracture. This study demonstrated that 5-year mortality is lower in older adults who recovered to their pre-fracture health-related quality of life (HRQoL) at 12-months compared to those who did not recover. Our results highlight the importance of post-fracture interventions known to improve HRQoL.
Introduction
Fragility fractures lead to increased mortality and decreased health-related quality of life (HRQoL) in older adults, although whether an association exists between these outcomes remains uncertain. The aim of this study was to determine whether recovery of HRQoL 12-month post-fracture is associated with lower 5-year mortality.
Methods
This data linkage study included 524 adults (mean age: 70.2 years; 79.2% women) with fragility fracture (150 hip, 261 distal forearm, 61 vertebral, 52 humerus) from the Australian arm of the International Costs and Utilities Related to Osteoporotic fractures Study (AusICUROS). HRQoL was measured using the EQ-5D-3L and all-cause mortality post-fracture was ascertained from the Australian National Death Index (NDI). Cox proportional hazards models were used to assess the association between HRQoL recovery (vs. non-recovery) and all-cause mortality within 5 years.
Results
Overall, 279 participants (53.2%) recovered to their pre-fracture HRQoL at 12-month follow-up. There were 70 deaths (13.4%) during the 5-year post-fracture. Mortality rate was the highest in hip fracture participants (24.7%), followed by vertebral (16.4%), humeral (13.5%), and distal forearm fracture participants (6.1%). After adjustment for age, pre-fracture HRQoL, and fracture site, mortality risk was lower in participants who recovered to their pre-fracture HRQoL at 12-months compared to those who did not recover (HR = 0.56, 95% CI: 0.33–0.96, p = 0.034).
Conclusion
This study provides evidence that HRQoL recovery post-fracture is associated with improved 5-year survival in older adults. The extent to whether current interventions known to improve HRQoL post-fracture could prevent some of these deaths is unknown.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporotic fractures are a major and increasing cause of health and economic burden worldwide, with approximately 1 in 3 women and 1 in 5 men over the age of 50 years experiencing a fracture in their lifetime [1, 2]. Fractures at any skeletal site are associated with increased pain, impaired physical function, and reduced health-related quality of life (HRQoL) [3,4,5]. However, it is well-established that hip and vertebral fractures are associated with larger declines in HRQoL, greater limitations in physical function, and a higher risk of mortality compared to fractures at other skeletal sites [4, 6,7,8,9].
There is a 25% mortality rate in the first year following hip fracture for individuals ≥ 60 years of age, with an increased risk of mortality persisting for at least 5 years [10, 11]. A similar mortality rate has also been reported in older adults with vertebral fractures [6,7,8]. However, non-hip non-vertebral fractures—such as fractures at the distal forearm, ribs, humerus, and pelvis—have also been reported to have considerable 5-year mortality rates, ranging from approximately 10–18% in men and women aged ≥ 60 years [5, 6, 12]. The International Costs and Utilities Related to Osteoporotic fractures Study (ICUROS) provided trajectories of HRQoL and rates of recovery to pre-fracture HRQoL for individual fracture sites from 11 different countries, both combined [4, 13] and country-specific [14, 15]. This study showed that older adults with a major osteoporotic fracture—defined as a fracture of the hip, distal forearm, vertebrae, or humerus—incur substantial loss in HRQoL for at least 18 months following the fracture.
While there is evidence that supports an association between fractures and increased risk of mortality, as well as evidence that confirms an association between fractures and decreased HRQoL, the association between HRQoL and mortality following fracture remains uncertain. Lower HRQoL has been shown to be associated with higher mortality rates among older adults [16, 17], heart failure patients [18], people with arthritis [19], and cancer patients [20]. However, it is unknown whether different trajectories of HRQoL post-fracture are associated with decreased risk of mortality.
The primary aim of this study was to determine whether recovery of HRQoL 12-month post-fracture is associated with lower 5-year all-cause mortality. A secondary aim was to investigate this association across individual fracture sites. Based on results from previous studies [16,17,18,19,20], we hypothesized that participants who recover to pre-fracture HRQoL at 12 months will have fewer deaths within 5 years of the fracture compared to those who do not recover.
Material and methods
Study design
The AusICUROS study design has been described elsewhere [9], however in brief, AusICUROS represents the Australian arm of ICUROS [4]. ICUROS was a multinational observational study undertaken between 2009 and 2014 across 11 countries (Australia, Austria, Estonia, France, Italy, Lithuania, Mexico, Russia, Spain, the UK, and the USA) to determine the HRQoL impact and cost consequences of fragility fractures in older adults aged ≥ 50 years. AusICUROS included eight study sites representing five states in Australia: New South Wales, Queensland, Tasmania, Victoria, and Western Australia. AusICUROS was undertaken under the auspices of the International Osteoporosis Foundation.
Participants
Individuals were recruited between 2009 and 2012 through hospital emergency departments and orthopedic wards. The eligibility criteria for AusICUROS were older adults (≥ 50 years of age) who had sustained a low-energy fragility fracture (confirmed via imaging) that was not caused by a comorbidity (e.g., cancer) and were living in their own home prior to their fracture. Individuals not expected to survive 12-month post-fracture, living in long-term care prior to the fracture, or with cognitive impairment were excluded from participating in the study. Additionally, participants who sustained a new fracture during the follow-up period were withdrawn from the study.
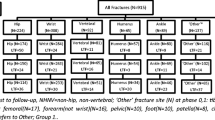
In total, 915 individuals were enrolled in AusICUROS. After exclusion of ineligible individuals (n = 12), those who sustained a fracture at a non-major osteoporotic site (n = 225), study drop-outs / lost-to-follow-up (n = 137), and participants who died during the first year of follow-up (n = 17), a total of 524 patients were included in this analysis (Fig. 1). Only participants with complete 12-month follow-up data were included in this analysis.
AusICUROS data
Participants were enrolled immediately after the fracture (0–2 weeks) and followed-up for 18 months. Data collection occurred at four time-points post-fracture: within 2 weeks, 4 months, 12 months, and 18 months.
Participant demographics
Participant demographic and fracture details were collected at the baseline interview (within 2 weeks of the study fracture) either in hospital by interview while the patient was receiving care for their fracture or over the phone for those who were not admitted to hospital. Patient demographic details including date of birth (age was calculated as the difference between date of birth and baseline interview date), sex, the highest level of educational attainment (primary, secondary, post-secondary, university), individual income (low, middle-high), living status at time of fracture (alone, with someone), and prior fracture in the previous 5 years (not including the study fracture) were collected via self-report surveys.
Health-related quality of life
Health-related quality of life (HRQoL) was assessed using the EuroQoL questionnaire (EQ-5D-3L) [21] at baseline (including recall of the patient’s HRQoL prior to fracture), and at 4- and 12-month post-fracture. We calculated utility index scores for the EQ-5D-3L using Australian time utility weights from general Australian population samples [22]. The utility index score provides an overall HRQoL composite score that encompasses the five dimensions of health measured by the EQ-5D-3L (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression). EQ-5D-3L utility index scores ranged from 1 (full health) to − 1 (a health state worse than dead) [22]. Recovery of HRQoL over 12 months was calculated as the difference between EQ-5D-3L utility scores at pre-fracture and 12-months, and then dichotomized (recovered/not recovered), where a HRQoL change score ≥ 0 was classified as “recovered” and a score < 0 was classified as “not recovered.”
Death ascertainment
Data on mortality were obtained from the National Death Index (NDI)—a database held by the Australian Institute of Health and Welfare (AIHW). The NDI is a Commonwealth database that contains records of deaths registered in Australia since 1980. Data comes from Registrars of Births, Deaths and Marriages in each jurisdiction, and the Australian Bureau of Statistics. The NDI is designed to facilitate the conduct of epidemiological or data linkage studies; and its use is strictly confined to medical research. Details of death variables available for data linkage include date of death; state or territory where death was registered; year of death registration; and underlying cause of death (labelled as ICD-10 codes since 1997).
Linkage between AusICUROS participant data and NDI mortality data was undertaken by members of the AIHW using probabilistic linkage software. The AusICUROS data custodian (KMS) sent an electronic, password-protected excel file to the AIHW, listing all AusICUROS participants with the following data linkage identifiers: given name, surname, date of birth, sex, postcode, and state of last known contact. When a possible match to the NDI was identified, the AIHW included the date of death and any recorded cause(s) of death for the corresponding AusICUROS participant. This linked dataset was then forwarded to the lead investigator (JT) in an electronic, encrypted file via Defigo (an online secure platform) with all identifiers removed, ensuring that the linking of databases did not subsequently result in any AusICUROS participants being identified.
Statistical analyses
Participants were divided by HRQoL status (recovered/not recovered). Demographic data and clinical characteristics were summarized as mean (SD) or frequency (percentage) and compared using Mann–Whitney U tests and independent t tests for continuous data, or chi-squared tests for categorical data. Overall survival was compared between the two HRQoL groups (recovered vs. not recovered) using a two-sided log-rank test. Survival curves were estimated using the Kaplan–Meier product-limit method (estimating all-cause mortality ratios by comparing the observed number of deaths and expected number of deaths). Cox proportional hazards models were constructed and Hazard ratios (HRs) and corresponding 95% confidence intervals (CIs) were calculated to assess the association between HRQoL recovery (vs. non-recovery) and all-cause mortality. For these analyses, time at risk began on the date of the study fracture and ended on the date of death, or 5-years post-fracture, whichever came first. We also assessed a pre-specified set of baseline characteristics for their relevance as prognostic factors for overall survival such as age, sex, pre-fracture HRQoL, study fracture site, education, income, employment status (pre-fracture), previous fracture, and osteoporosis-related treatment. For these univariate models, a p value of ≤ 0.10 was used for selection of potentially important covariates to be included in multivariable models [23]. In the multivariable model, a backward, stepwise elimination process with the more stringent p value of < 0.05 was implemented to identify the final model. The proportional hazards assumption was tested using Schonfeld residuals and met for all variables used in analysis. Sensitivity analyses were undertaken using the minimal important difference of 0.074 to calculate recovery of HRQoL [24], allowing for measurement error in the EQ-5D-3L score. This previously published minimal important difference has been widely used in studies that have used HRQoL across the health research sector. Analyses by fracture type were not undertaken due to insufficient sample size. All analyses were performed using the STATA (version 16) software.
Results
Participants
Participant baseline characteristics are shown in Table 1, for the total sample and by the two HRQoL groups (recovered/not recovered). The sample had a mean age of 70.2 years and consisted of mostly women (79.2%). There were 150 participants with a hip fracture, 261 participants with distal forearm fractures, 61 participants with vertebral fractures, and 52 participants with humeral fractures. Overall, 279 participants (53.2%) recovered to their pre-fracture HRQoL at the 12-month follow-up. The proportion of participants who recovered to their pre-fracture HRQoL was similar for hip, vertebral, and humeral fractures (40.7%, 45.9%, and 40.4%, respectively), and higher for distal forearm fractures (64.8%). Participants who recovered to their pre-fracture HRQoL were younger, more likely to have university-level education and have higher income compared with non-recovered participants. The groups did not differ in terms of sex, employment status, living alone, previous fractures within the last 5 years or pre-fracture HRQoL (Table 1).
Mortality
There was a total of 87 deaths (13.4%) during the 5-years following the study fracture: 17 deaths during year one, 13 deaths in year two, 19 deaths during year three, 12 deaths in year four, and 26 deaths during year five of follow-up. The mortality rate was the highest in hip fracture participants (24.7%), followed by vertebral (16.4%), humeral (13.5%), and distal forearm fracture participants (6.1%). Circulatory system disease was the most common cause of death (n = 23, 26.4%), followed by malignant neoplasms (n = 19, 21.8%), diseases of the respiratory system (n = 18, 20.7%), and endocrine, nutritional or metabolic diseases (n = 5, 5.7%) (Supplementary Table 1). Univariate analyses identified the following variables as significant predictors for mortality: age, sex, education, income level, living alone, employment status, pre-fracture HRQoL, osteoporosis-related medication use, allied health care, and fracture site (Table 2).
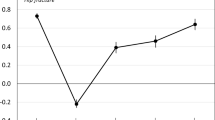
Participants who recovered to their pre-fracture HRQoL at 12-month follow-up had a lower mortality risk compared to those who did not recover (unadjusted HR = 0.45, 95% CI: 0.27–0.75, p = 0.01) (Table 2 and Fig. 2). This association was slightly attenuated after adjusting for age and sex (model 1) yet remained significant (HR = 0.54, 95% CI: 0.32–0.91, p = 0.02) (Table 3). After further adjustment for characteristics found to be significant in univariate analyses (model 2), mortality risk remained lower for participants who recovered to their pre-fracture HRQoL compared to those who did not recover (HR = 0.52, 95% CI: 0.30–0.89, p = 0.02) (Table 3). Similar results were found in model 3 when baseline characteristics that were not significant in model 2 were removed (HR = 0.56, 95% CI: 0.33–0.96, p = 0.03) (Table 3). There were no important differences in our sensitivity analysis results when recovery of HRQoL was calculated using the minimal important difference cut-off points.
Discussion
This large observational study demonstrated that older individuals who recover to their pre-fracture HRQoL at 12-months post-fracture have a significantly lower risk of mortality within 5-years of fracture compared to those who do not recover to their pre-fracture HRQoL. These associations remained statistically significant after adjustment for several predictors of death, such as age and pre-fracture HRQoL. To our knowledge, this is the first study evaluating an association between HRQoL recovery and mortality in older individuals post-fracture.
The detrimental health impact that fractures have on older people have been continually demonstrated in the literature. In the early 2000s, a number of observational studies revealed that older men and women with a fragility fracture experience substantial and prolonged impairments in HRQoL for most fracture sites [25,26,27,28,29]. More recent studies have confirmed these findings [30, 31], including the ICUROS study, which is the largest prospective observational study that aimed to identify the HRQoL consequences of fragility fractures across multiple countries [4]. It is also well-established that mortality rates are high post-fracture, more specifically for hip and vertebral fractures [32,33,34,35]. This was also seen in our study, with higher rates of deaths reported in hip and vertebral fracture participants compared to humeral and distal forearm fracture participants. While some studies have determined that fractures are associated with both decreased HRQoL and increased mortality in older adults [29, 36,37,38], it remained to be shown whether these two outcomes were correlated, more so, whether improved HRQoL translated into decreased long-term mortality post-fracture. Our study shows that recovery of pre-fracture HRQoL at 12-months is associated with 5-year mortality. Given that specific post-fracture interventions have been shown to improve HRQoL compared to standard care [39], our results provide indirect evidence that these interventions may have the potential to prevent deaths in older adults post-fracture. Future research evaluating current post-fracture interventions is encouraged to determine whether this association exists.
The specific causes of excess mortality after fracture are poorly understood and inconsistent in the literature. Increasing age conferred an additional mortality risk (8% rise in mortality risk per increased year in age) as per previous studies [6, 29, 32, 40, 41]. Risk of mortality did not significantly differ by sex, even though men are known to have higher mortality rates following fragility fracture compared to women [6, 33]. Participants with a university level of education had a lower mortality risk compared to individuals with high school/secondary education, as did participants with higher income levels and those who were employed before their fracture. Inequalities for mortality post-hip fracture have also been reported in a recent meta-analysis, which found that overall risk of 1-year mortality in individuals with low socioeconomic status was 24% higher than in individuals with high socioeconomic status (for both combined and individual-level socioeconomic measures) [42]. We also detected that previous fracture in the past 5 years was not a predictor for mortality at 5-years. Pre-fracture HRQoL was found to be a significant predictor of 5-year mortality, similar to a study by Pande et al. that reported that lower pre-fracture HRQoL in participants (measured by the physical component domain of the SF-36) showed a higher excess mortality rate compared with a non-fracture control group [29]. Using distal forearm fractures as the reference group, we found that hip, vertebral, and humeral fractures were associated with a 4.3-fold, 3.2-fold, and 2.3-fold increase in mortality risk, respectively. This is consistent with a number of previous large-scale, prospective observational studies [33,34,35]. Only age, pre-fracture HRQoL, and fracture site remained significant after adjusting for these baseline variables in the multivariable model, suggesting that these factors are partly correlated with the complex association between HRQoL recovery and mortality post-fracture.
Strengths and limitations
Our study has several strengths. The present study is the first that uses long-term, follow-up data of a large cohort across a range of low-trauma fractures to evaluate the association between HRQoL and mortality. Importantly, the AusICUROS study sample included the four major osteoporotic fracture sites—hip, distal forearm, vertebrae, and humerus—allowing for understanding of how fractures at different sites independently predict HRQoL recovery and mortality. Published data on mortality following non-hip, non-vertebral fractures are relatively scarce [42, 43], despite non-hip, non-vertebral fractures accounting for more than 50% of fractures [44]. Data linkage between AusICUROS participant data and the NDI national registry ensured complete ascertainment of deaths. Finally, AusICUROS provides a representative sample of fracture patients across Australian metropolitan and regional hospitals, increasing the generalizability of our findings.
There were however several limitations to this study. First, we were unable to adjust for all known covariates as AusICUROS did not investigate factors known to influence long-term health outcomes in older adults such as comorbidities or body mass index. However, previous studies in hip fracture patients have found that comorbidities only account for a small proportion of excess mortality after the fracture‐related mortality association itself [32, 40, 41]. Second, the original AusICUROS study was not designed to assess long-term mortality and there was insufficient power to detect a true association between HRQoL recovery and mortality by fracture site. Third, pre-fracture HRQoL was determined by patient recall at the baseline interview, subjecting this study to recall bias. Although given that mean pre-fracture EQ-5D utility scores were similar to previously reported population norms [45], it is unlikely recall bias is evident in this study. Fourth, even though the AusICUROS sample reflects the typical profile of the fracture population, exclusion of nursing home residents, those with cognitive impairment, and those who suffered a second fracture during follow-up may have introduced bias into analyses. Additionally, excluding patients who died within 12 months of their fracture may have subjected this analysis to survivor bias. Finally, as in all observational studies, unrecognized confounding is likely.
Conclusion
Better understanding of factors that lead to excess mortality is important to inform future health policies aimed at reducing the health and economic burden associated with fragility fractures. This study provides evidence that HRQoL recovery 12-months post-fracture is associated with improved 5-year survival in older adults who suffer a fragility fracture. Our findings also highlight the important contributions of a variety of demographic factors that predict long-term mortality post-fracture. Larger studies are needed to determine the associations between HRQoL and mortality risk according to fracture site. From a public health perspective, our study provides greater rationale for monitoring HRQoL in clinical practice.
Data availability
The data for these analyses was accessed from the AusICUROS central database. Access to this database should be discussed with the data custodian (KMS).
References
Kanis JA, Johnell O, Oden A, Sembo I, Redlund-Johnell I, Dawson A, De Laet C, Jonsson B (2000) Long-term risk of osteoporotic fracture in Malmo. Osteoporos Int 11:669–674
Curtis EM, van der Velde R, Moon RJ, van den Bergh JP, Geusens P, de Vries F, van Staa TP, Cooper C, Harvey NC (2016) Epidemiology of fractures in the United Kingdom 1988–2012: variation with age, sex, geography, ethnicity and socioeconomic status. Bone 87:19–26
Mears SC, Kates SL (2015) A guide to improving the care of patients with fragility fractures, Edition 2. Geriatr Orthop Surg Rehabil 6:58–120
Svedbom A, Borgstom F, Hernlund E et al (2018) Quality of life for up to 18 months after low-energy hip, vertebral, and distal forearm fractures-results from the ICUROS. Osteoporos Int 29:557–566
Gosch M, Druml T, Nicholas JA, Hoffmann-Weltin Y, Roth T, Zegg M, Blauth M, Kammerlander C (2015) Fragility non-hip fracture patients are at risk. Arch Orthop Trauma Surg 135:69–77
Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR (2009) Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA 301:513–521
Kanis JA, Johnell O, De Laet C et al (2004) A meta-analysis of previous fracture and subsequent fracture risk. Bone 35:375–382
Cauley JA, Hochberg MC, Lui LY, Palermo L, Ensrud KE, Hillier TA, Nevitt MC, Cummings SR (2007) Long-term risk of incident vertebral fractures. JAMA 298:2761–2767
Abimanyi-Ochom J, Watts JJ, Borgstrom F et al (2015) Changes in quality of life associated with fragility fractures: Australian arm of the International Cost and Utility Related to Osteoporotic Fractures Study (AusICUROS). Osteoporos Int 26:1781–1790
Nordstrom P, Gustafson Y, Michaelsson K, Nordstrom A (2015) Length of hospital stay after hip fracture and short term risk of death after discharge: a total cohort study in Sweden. BMJ 350:h696
Haentjens P, Magaziner J, Colón-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B, Boonen S (2010) Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med 152:380–390
Johnell O, Kanis JA, Oden A, Sernbo I, Redlund-Johnell I, Petterson C, De Laet C, Jonsson B (2004) Mortality after osteoporotic fractures. Osteoporos Int 15:38–42
Talevski J, Sanders KM, Busija L, Beauchamp A, Duque G, Borgstrom F, Kanis JA, Svedbom A, Stuart AL, Brennan-Olsen S (2021) Health service use pathways associated with recovery of quality of life at 12-months for individual fracture sites: Analyses of the International Costs and Utilities Related to Osteoporotic fractures Study (ICUROS). Bone 144:115805
Talevski J, Sanders KM, Busija L et al (2021) Health service use and quality of life recovery 12 months following major osteoporotic fracture: latent class analyses of the International Costs and Utilities Related to Osteoporotic Fractures Study (ICUROS). J Bone Miner Res 36:252–261
Borgstrom F, Lekander I, Ivergard M et al (2013) The International Costs and Utilities Related to Osteoporotic Fractures Study (ICUROS)–quality of life during the first 4 months after fracture. Osteoporos Int 24:811–823
Otero-Rodriguez A, Leon-Munoz LM, Balboa-Castillo T, Banegas JR, Rodriguez-Artalejo F, Guallar-Castillon P (2010) Change in health-related quality of life as a predictor of mortality in the older adults. Qual Life Res 19:15–23
Tsai S-Y, Chi L-Y, Lee C-h, Chou P (2007) Health-related quality of life as a predictor of mortality among community-dwelling older persons. Eur J Epidemiol 22:19
Zuluaga MC, Guallar-Castillón P, López-García E, Banegas JR, Conde-Herrera M, Olcoz-Chiva M, Rodríguez-Pascual C, Rodriguez-Artalejo F (2010) Generic and disease-specific quality of life as a predictor of long-term mortality in heart failure. Eur J Heart Fail 12:1372–1378
Singh JA, Nelson DB, Fink HA, Nichol KL (2005) Health-related quality of life predicts future health care utilization and mortality in veterans with self-reported physician-diagnosed arthritis: the veterans arthritis quality of life study. Semin Arthritis Rheum 34:755–765
De Aguiar SS, Bergmann A, Mattos IE (2014) Quality of life as a predictor of overall survival after breast cancer treatment. Qual Life Res 23:627–637
Rabin R, de Charro F (2001) EQ-5D: a measure of health status from the EuroQol Group. Ann Med 33:337–343
Viney R, Norman R, King MT, Cronin P, Street DJ, Knox S, Ratcliffe J (2011) Time trade-off derived EQ-5D weights for Australia. Value Health 14:928–936
Boomsma A (2000) Reporting analyses of covariance structures. Struct Equ Model 7:461–483
Walters SJ, Brazier JE (2005) Comparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6D. Qual Life Res 14:1523–1532
Borgstrom F, Zethraeus N, Johnell O et al (2006) Costs and quality of life associated with osteoporosis-related fractures in Sweden. Osteoporos Int 17:637–650
Brenneman SK, Barrett-Connor E, Sajjan S, Markson LE, Siris ES (2006) Impact of recent fracture on health-related quality of life in postmenopausal women. J Bone Miner Res 21:809–816
Hallberg I, Rosenqvist AM, Kartous L, Lofman O, Wahlstrom O, Toss G (2004) Health-related quality of life after osteoporotic fractures. Osteoporos Int 15:834–841
Adachi JD, Loannidis G, Berger C et al (2001) The influence of osteoporotic fractures on health-related quality of life in community-dwelling men and women across Canada. Osteoporos Int 12:903–908
Pande I, Scott DL, O’Neill TW, Pritchard C, Woolf AD, Davis MJ (2006) Quality of life, morbidity, and mortality after low trauma hip fracture in men. Ann Rheum Dis 65:87–92
Peeters CM, Visser E, Van de Ree CL, Gosens T, Den Oudsten BL, De Vries J (2016) Quality of life after hip fracture in the elderly: a systematic literature review. Injury 47:1369–1382
Si L, Winzenberg TM, de Graaff B, Palmer AJ (2014) A systematic review and meta-analysis of utility-based quality of life for osteoporosis-related conditions. Osteoporos Int 25:1987–1997
Chen W, Simpson JM, March LM, Blyth FM, Bliuc D, Tran T, Nguyen TV, Eisman JA, Center JR (2018) Comorbidities only account for a small proportion of excess mortality after fracture: a record linkage study of individual fracture types. J Bone Miner Res 33:795–802
Brown JP, Adachi JD, Schemitsch E et al (2021) Mortality in older adults following a fragility fracture: real-world retrospective matched-cohort study in Ontario. BMC Musculoskelet Disord 22:105
Tran T, Bliuc D, Hansen L et al (2018) Persistence of excess mortality following individual nonhip fractures: a relative survival analysis. J Clin Endocrinol Metab 103:3205–3214
Lee SB, Park Y, Kim DW et al (2021) Association between mortality risk and the number, location, and sequence of subsequent fractures in the elderly. Osteoporos Int 32:233–241
Caliri A, De Filippis L, Bagnato GL, Bagnato GF (2007) Osteoporotic fractures: mortality and quality of life. Panminerva Med 49:21–27
Makridis KG, Karachalios T, Kontogeorgakos VA, Badras LS, Malizos KN (2015) The effect of osteoporotic treatment on the functional outcome, re-fracture rate, quality of life and mortality in patients with hip fractures: a prospective functional and clinical outcome study on 520 patients. Injury 46:378–383
Marques A, Lourenco O, da Silva JA, Portuguese Working Group for the Study of the Burden of Hip Fractures in P (2015) The burden of osteoporotic hip fractures in Portugal: costs, health related quality of life and mortality. Osteoporos Int 26:2623–2630
Talevski J, Sanders KM, Duque G, Connaughton C, Beauchamp A, Green D, Millar L, Brennan-Olsen SL (2019) Effect of clinical care pathways on quality of life and physical function after fragility fracture: a meta-analysis. J Am Med Dir Assoc 20(7):926.e1-926.e11. https://doi.org/10.1016/j.jamda.2019.02.022
Vosoughi AR, Emami MJ, Pourabbas B, Mahdaviazad H (2017) Factors increasing mortality of the elderly following hip fracture surgery: role of body mass index, age, and smoking. Musculoskelet Surg 101:25–29
Vestergaard P, Rejnmark L, Mosekilde L (2007) Increased mortality in patients with a hip fracture-effect of pre-morbid conditions and post-fracture complications. Osteoporos Int 18:1583–1593
Valentin G, Pedersen SE, Christensen R, Friis K, Nielsen CP, Bhimjiyani A, Gregson CL, Langdahl BL (2020) Socio-economic inequalities in fragility fracture outcomes: a systematic review and meta-analysis of prognostic observational studies. Osteoporos Int 31:31–42
Holloway KL, Henry MJ, Brennan-Olsen SL, Bucki-Smith G, Nicholson GC, Korn S, Sanders KM, Pasco JA, Kotowicz MA (2016) Non-hip and non-vertebral fractures: the neglected fracture sites. Osteoporos Int 27:905–913
Borgstrom F, Karlsson L, Ortsater G et al (2020) Fragility fractures in Europe: burden, management and opportunities. Arch Osteoporos 15:59
Szende A, Janssen B, Cabases J (2014) Self-reported population health: an international perspective based on EQ-5D. Springer, Dordrecht
Acknowledgements
We are grateful to the quality of life and Epidemiology Working Group of the Committee of Scientific Advisors for the International Osteoporosis Foundation under whose supervision ICUROS was undertaken. We are also grateful the Australian Institute for Health and Welfare (AIHW) team for undertaking the data linkage.
Funding
JT is supported by an Australian National Health and Medical Research Council (NHMRC, of Australia) Postgraduate Scholarship (1151089). AusICUROS was supported by the NHMRC (Project Grant Number: 628422) with subsidiary funding support from Merck Australia Pty Ltd.
Author information
Authors and Affiliations
Contributions
JK, FB, and AS are integral to the ICUROS international study protocol and are Principal Investigators and members of the ICUROS Steering Committee. KMS (principal investigator), ES, SI, and GD are chief investigators of AusICUROS. JT, KMS, and SLB-O contributed to the conception and design of the study. KMS, SI, AS, and ALS provided additional participant data for the data linkage. JT designed and executed the statistical analyses with assistance from SV. JT drafted all sections of the manuscript and led the interpretation of findings. All authors provided critical input regarding interpretation of results and approved the final manuscript for publication.
Corresponding author
Ethics declarations
Ethics approval
AusICUROS was approved by the relevant human research ethics committees (HREC) in each of the eight participating study centers in Australia (lead site Barwon Health HREC: 09/49). Approval for the use of AusICUROS data in these post hoc analyses was obtained from Melbourne Health HREC (2020.182) and from the Australian Institute of Health and Welfare (AIHW) HREC (2020.4.1189).
Consent to participate
Informed consent was individually obtained from all participants included in the study and participants could withdraw from the study at any time.
Consent for publication
All authors approved the final manuscript for publication.
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Talevski, J., Sanders, K.M., Vogrin, S. et al. Recovery of quality of life is associated with lower mortality 5-year post-fracture: the Australian arm of the International Costs and Utilities Related to Osteoporotic Fractures Study (AusICUROS). Arch Osteoporos 16, 112 (2021). https://doi.org/10.1007/s11657-021-00981-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-021-00981-y