Abstract
Summary
In this study, the risk of fatality after hip fracture but not the risk of subsequent hip fractures was higher among men.
Introduction
The purpose of this study was to analyze the risk factors for subsequent hip fractures and fatality after an initial hip fracture among Koreans older than 50 years of age using information in the national claims database.
Methods
Our study was conducted using data from the Korean National Health Insurance Service database from 2007 to 2016. A total of 16,915 Korean patients aged ≥ 50 years with a first hip fracture in 2012 were followed for 4 years. Data on fracture, comorbidity, and prescription variables were retrieved from the national registry. The Cox proportional hazards model was used to identify the risk factors affecting subsequent hip fractures and fatality after the initial hip fracture.
Results
A total of 952 patients had subsequent hip fractures, and 6793 patients died. The cumulative incidence rates were 1.3% after 1 year and 5.6% after 4 years. Old age, renal disease, dementia, and Parkinson’s disease were associated with a higher risk of subsequent hip fractures. The fatality rate after the initial hip fracture was 1.6 times higher among men than among women. Certain risk factors for fatality, such as pneumonia after fracture, cerebrovascular disease, mild liver disease, renal disease, and malignancy, were more prevalent among men.
Conclusion
During the study period, the risk of fatality after hip fracture but not the risk of subsequent hip fractures was higher among men. The gender difference in fatality might be explained by the larger burden of comorbid diseases among men.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The global population is aging, and the increased life expectancy of the elderly population is considered the most important reason underlying the increased incidence of osteoporotic fractures [1,2,3,4]. Osteoporotic fractures in the elderly population result in high mortality and morbidity, greatly reducing the quality of life for the remaining years [5, 6].
Subsequent osteoporotic fractures have increased concerns among patients who failed to manage their osteoporosis after an initial fracture [7, 8]. Among cases of osteoporotic fractures, hip fractures have the worst prognosis because of high mortality and the loss of independence. However, studies on the incidence and risk factors for subsequent hip fractures are limited by the lower incidence of subsequent hip fractures compared with that of the initial hip fracture and the need for a large sample size.
The purpose of this study was to analyze the risk factors for subsequent hip fractures and fatality after an initial hip fracture among Koreans older than 50 years of age using information in the national claims database of the Korean National Health Insurance Service (KNHIS) from 2007 to 2016.
Materials and methods
Ethics statement
The study protocol was approved by the institutional review board (IRB) of Wonkwang University Sanbon Hospital (IRB No. WMCSB 201706-64). The requirement for informed consent was waived because the study was based on routinely collected administrative and claims data.
Data source
This study used data derived from the Korean National Health Insurance (KNHI) claims database from 1 January 2007 to 31 December 2016. The KNHIS guarantees health services to the Korean population, except for cosmetic surgery and services related to traffic or industrial accidents. All clinics and hospitals submit patient information, such as patient diagnoses (International Classification of Diseases, 10th Revision [ICD-10]), prescriptions, and procedures, to the KNHIS for claims. Therefore, the database comprises complete paid claims data including patient diagnoses, prescriptions, procedures, surgeries, outpatient physician encounters, and hospitalizations. All personal identification numbers were converted to anonymous codes so that they could not be tracked. The KNHIS claims database has the medical information of every Korean (~ 50 million) who has used medical services [9]. The database includes information pertaining to the reimbursement for each medical service, such as basic patient demographics, clinic or hospital identifiers, disease codes, costs incurred, the results of health screening, individual/family health history, health behavior, and information related to the cause of death [10].
Study population and follow-up
To analyze the incidence and risk factors for subsequent hip fractures, we conducted a population-based, retrospective cohort study. First, we identified subjects who experienced hip fractures in a cohort of Koreans aged 50 or older between 1 January and 31 December 2012 (n = 30,313). We excluded subjects who experienced any osteoporotic fracture including fractures of the hip, vertebra, distal radius, and humerus between 2007 and 2011 (n = 22,254). In addition, we excluded subjects with conditions resulting from high-impact traumas (multiple fractures) (n = 16,971). Ultimately, 16,915 participants were selected in the initial hip fracture group. Follow-up lasted from the date of the initial hip fracture diagnosis (index date) to the subsequent hip fracture, death, or 4 years.
Operational definition of hip fractures
Hip fractures were identified by using an algorithm based on selected ICD-10 codes and procedure codes used to search the claims database (Supplementary Table 1). First, fracture codes with procedure codes, including open reduction of a fractured extremity (femur), closed pinning (femur), external fixation (pelvis/femur), closed reduction of a fractured extremity (pelvis/femur), bone traction, skin traction, hemiarthroplasty, and total hip arthroplasty (hip), were regarded as hip fractures. Second, based on the last claim date, subsequent hip fractures were defined as fractures for which recurrent inpatient or outpatient treatment claims were made with a hip fracture diagnosis after the index date and an interval of at least 6 months between the claims [11].
Statistical analysis
Statistical comparison between groups was performed by using the t test or chi-square test. When appropriate, the Kaplan–Meier method was used to illustrate the estimated cumulative incidence of subsequent hip fractures and fatality after an initial hip fracture. The log-rank test was used to compare the incidence and fatality rate according to sex and age. The Cox proportional hazards model was used to evaluate the effect of clinical characteristics on the risk of subsequent hip fractures and fatality after the initial hip fracture. To eliminate the risk of immortal time bias, we performed the landmark analyses at 1, 2, and 3 years after the initial hip fracture. In the landmark method, a fixed time point during the follow-up period was selected as a landmark for conducting the analysis of survival. Only those subjects who had survived until the landmark time were included in the analysis [12].
Covariates included age, sex, fracture subtype, comorbidities before or after the index date, and the use of bisphosphonate (BP) and anticoagulants after the index date. Among the comorbidities, pneumonia, sepsis, and venous thromboembolism were evaluated for 6 months after the index date, and other comorbidities were evaluated for 1 year before the index date. The use of BP and anticoagulants was assessed from the index date to the end of the study. The use of BP is presented as the proportion of the follow-up period in which BP was used.
Effect sizes are presented as hazard ratios (HRs) and 95% confidence intervals (CIs). Database management and all analyses were performed using the SAS statistical package version 9.3 (SAS Institute, Cary, NC, USA).
Results
Incidence of subsequent hip fractures
Of the 30,313 subjects with hip fractures in 2012, 16,915 subjects with an initial hip fracture were followed for 4 years. Among them, women accounted for 68.5%. Men were significantly younger than women (73.7 versus 78.9 years). At the time of the initial fracture, the rates of congestive heart failure, dementia, rheumatic disease, and diabetes mellitus (DM) without complications were significantly higher among women than among men. However, the rates of myocardial infarction, peripheral vascular disease, cerebrovascular disease, chronic obstructive pulmonary disease (COPD), mild liver disease, hemiplegia, renal disease, and any malignancy were significantly higher among men. After initial hip fracture, the rate of pneumonia was significantly higher among men, and that of venous thromboembolism was significantly higher among women. The use of BP was significantly higher among women (Table 1).
Over 4 years, 952 patients had subsequent hip fractures, including 710 (74.6%) women and 242 (25.4%) men. Supplementary Table 2 shows the age- and gender-stratified incidence of subsequent hip fractures. The incidence rates of subsequent hip fractures were 1.5%, 2.1%, 2.2%, and 2.0% in the first, second, third, and fourth year, respectively. The cumulative incidence of subsequent hip fractures was higher among women (Fig. 1a) and was increased with age (Fig. 1b).
To identify the risk factors for subsequent hip fractures, Cox proportional hazards regression analyses were performed (Table 2). According to the results of multivariate analysis, there were no significant differences between men and women in the occurrence of subsequent fractures. Age was a significant risk factor; the adjusted HRs for subsequent fractures were 1.25 (95% CI 1.0–1.57) for patients aged 65–80 years and 1.38 (95% CI, 1.09–1.74) for patients older than 80 years compared with patients aged 50–65 years. In comparison with femur neck fracture, intertrochanteric fracture had a lower risk of subsequent fractures (HR 0.88, 95% CI 0.77–1.0). Dementia (HR 2.13, 95% CI 1.82–2.5), renal disease (HR 2.33, 95% CI 1.7–3.2), metastatic solid cancer (HR 3.15, 95% CI 1.0–9.99), and Parkinson’s disease (HR 1.58, 95% CI 1.14–2.17) were identified as significant risk factors for subsequent hip fractures. Interestingly, cerebrovascular disease (HR 0.76, 95% CI 0.62–0.93) was associated with a reduced risk of subsequent fractures. The use of BP (≥ 50%) after the initial fracture was not associated with subsequent fracture reduction.
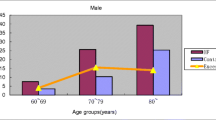
Fatality rate after an initial hip fracture
A total of 6793 patients died after an initial hip fracture by the end of the follow-up period. Women accounted for 63.9% (n = 4343) of the deaths and were older than men at death (82.6 versus 77.8 years). The fatality rate of men was significantly higher than that of women during the follow-up period after the initial hip fracture (P < 0.001, Fig. 2a). The fatality rate was also significantly increased with increasing age (P < 0.001, Fig 2b).
We further examined the risk factors for fatality after an initial hip fracture. The results of multivariate analysis showed that male gender, old age, intertrochanteric fracture type, congestive heart failure, cerebrovascular disease, dementia, mild liver disease, DM with chronic complications, renal disease, any malignancy, moderate to severe liver disease, metastatic solid tumor, Parkinson’s disease, pneumonia, and sepsis were statistically significant risk factors (Table 3). The risk of death among women was decreased compared with that among men during the follow-up period (HR 0.63, 95% CI 059–0.66, P < 0.001). Age was a significant risk factor for death; the adjusted HRs for death were 2.07 (95% CI 1.83–2.34) for patients aged 65–80 years and 4.4 (95% CI, 3.91–4.97) for patients older than 80 years compared with patients aged 50–65 years. Intertrochanteric fracture, cerebrovascular disease, mild liver disease, renal disease, any malignancy, and pneumonia were significantly more prevalent among men than among women (Table 1). In the subgroup analysis according to gender, cerebrovascular disease and moderate to severe liver disease were significant risk factors for fatality only among men, and mild liver disease was a significant risk factor for fatality only among women. The use of BP (≥ 50%) was associated with a significant decrease in fatality after hip fracture only among women. Supplementary Table 3 shows the results of the landmark analysis. The adjusted HRs of pneumonia were 2.12 (95% CI, 1.97–2.27) at 1 year but gradually decreased to 1.61(95% CI, 1.43–1.8) at 2 years and 1.52 (95% CI, 1.3–1.77) at 3 years. At 3 years, sepsis was not significantly associated with fatality. The adjusted HRs of BP use (≥ 50%) were similar at all landmark points.
Discussion
The present study examined the incidence of subsequent hip fractures in a population-based cohort of subjects aged ≥ 50 years who sustained an initial hip fracture in 2012. The incidence of subsequent hip fractures was lower in our study than in other studies using claims data. Ryg et al. reported that the cumulative incidence rates of subsequent hip fractures were 9% after 1 year and 20% after 5 years in a cohort study in Denmark (1977–2001) [13]. In a study in Austria (2008–2010), the cumulative incidence rates of subsequent hip fractures after 1, 2, and 3 years were reported as 2.97%, 5.28%, and 7.19%, respectively [14]. In Taiwan, the incidence of subsequent hip fractures was determined by analyzing information in the Taiwan National Health Insurance Research Database (2001–2011) for 95,484 hip fracture patients [15]. The cumulative incidence rates of subsequent hip fractures within 1 year and 4 years were 2.2% and 6.3%, respectively, for women and 1.8% and 4.7%, respectively, for men. In particular, subsequent fractures occurred most frequently in the first year. Hip fracture rates are higher in Denmark, Austria, and Taiwan than in Korea; thus, the incidence of subsequent fractures may also be higher [16]. However, as we did not include fractures that occurred in the 6 months after the initial fracture, the 1-year incidence rates in this study might be underestimated. In addition, we excluded subjects who experienced osteoporotic fractures (hip, spine, distal radius, and humerus) before the initial hip fracture; thus, the incidence of subsequent hip fractures may be lower than that in other studies. Nevertheless, in a previous study in Korea, Lee et al. reported that the cumulative 1-year, 2-year, and 3-year incidence rates of subsequent hip fractures were 1.0%, 1.9%, and 2.2%, respectively, using claims data between 2007 and 2011 [17]. In Korea, the number of hip fractures has increased until recently; thus, it is thought that the incidence of subsequent fractures has also increased.
In this study, old age, renal disease, dementia, and Parkinson’s disease were significant predictors for subsequent hip fractures. The results are in agreement with the findings of a previous study [18]. Dementia and Parkinson’s disease may be related to the risk of second hip fractures through possible falls associated with cognitive impairment or medication [19, 20]. In univariate analysis, the incidence of subsequent hip fractures was higher among women than among men; however, there was no significant gender difference in multivariate analysis. Several previous studies reported that women gender was a strong predictor for subsequent hip fractures [14, 15]. However, a study of a UK population by Sheikh et al. reported results similar to our findings [19]. The use of BP after fractures has been proven beneficial in reducing the risk of subsequent fractures [17, 18]. However, in this study, the use of BP after the initial fracture was not meaningful for the prevention of subsequent fractures, which may be explained by the use of BP in a high-risk group. Importantly, the number of people who have been prescribed with BP for 50% or more of the follow-up period after hip fracture was too small (10.2%); thus, further strategies need to be developed to improve drug persistence for subsequent fracture prevention.
Hip fractures occur frequently among women; however, the fatality rate after hip fracture has been reported to be higher among men than among women [15, 21]. Similar results were obtained in this study; the fatality rate after hip fracture was 1.6 times higher among men than among women, and this difference persisted for 4 years. In a previous study that analyzed the cause of death among men and women after hip fracture, Wehren et al. found that deaths caused by infection were more common among men than among women [22]. In addition, baseline comorbidities, fracture type, and postoperative complications did not explain the gender difference. They estimated that the increased rate of deaths caused by infection could be responsible for the gender difference [22]. However, in our study, individual comorbidities such as congestive heart failure, cerebrovascular disease, dementia, renal disease, any malignancy, metastatic solid cancer, Parkinson’s disease, pneumonia, and sepsis after fracture were independent predictors for fatality after hip fracture. In agreement with previous findings, pneumonia after fracture was more common among men in our study. Moreover, several baseline comorbidities identified as risk factors were more prevalent among men. In addition, the use of BP, a protective factor against fatality, was significantly lower among men. Therefore, the burden of baseline comorbid diseases and post-fracture pneumonia may be responsible for the gender difference.
This study had several limitations. First, due to database limitations, we could not consider bone mineral density (BMD), laboratory data such as vitamin D and calcium, body mass index, and smoking or alcohol status. Second, although the operative definition of the study excluded pathologic fractures or high-energy trauma, it was not possible to clinically diagnose disease-associated fractures. Therefore, the data on fracture incidence may have been overestimated. Nevertheless, to distinguish it as much as possible, we only included patients older than 50 years who fulfilled specific inclusion criteria that had been used in previous studies. Third, as there was no information on the direct cause of death after hip fracture, only the accompanying diseases were analyzed to explain gender differences. Finally, we did not have information on postoperative functional recovery. Previously, Berry et al. reported that age and functional status were the most significant risk factors for subsequent hip fractures in a US population [23]. In the future, if a database of hospital records linked to claims data is established, more in-depth research may be conducted.
In conclusion, the risk of subsequent hip fracture was increased continuously in 4 years from the initial hip fracture. The factors affecting the occurrence of subsequent fractures were old age, renal disease, dementia, and Parkinson’s disease. There was no gender difference in the risk of subsequent hip fractures. The fatality rate after hip fracture was 1.6 times higher among men than among women. Several risk factors for fatality including pneumonia after fracture, cerebrovascular disease, mild liver disease, renal disease, and malignancy were more prevalent among men. Therefore, the gender difference in fatality might be explained by the larger burden of comorbid diseases among men.
References
Lems WF, Raterman HG (2017) Critical issues and current challenges in osteoporosis and fracture prevention. An overview of unmet needs. Ther Adv Musculoskelet Dis 9(12):299–316
Kontis V, Bennett JE, Mathers CD, Li G, Foreman K, Ezzati M (2017) Future life expectancy in 35 industrialised countries: projections with a Bayesian model ensemble. Lancet 389(10076):1323–1335
Doherty DA, Sanders KM, Kotowicz MA, Prince RL (2001) Lifetime and five-year age-specific risks of first and subsequent osteoporotic fractures in postmenopausal women. Osteoporos Int 12(1):16–23
Dennison E, Mohamed MA, Cooper C (2006) Epidemiology of osteoporosis. Rheum Dis Clin N Am 32(4):617–629
Teng GG, Curtis JR, Saag KG (2008) Mortality and osteoporotic fractures: is the link causal, and is it modifiable? Clin Exp Rheumatol 26(5 Suppl 51):S125–S137
Nazrun AS, Tzar MN, Mokhtar SA, Mohamed IN (2014) A systematic review of the outcomes of osteoporotic fracture patients after hospital discharge: morbidity, subsequent fractures, and mortality. Ther Clin Risk Manag 10:937–948
van den Berg P, Schweitzer DH, van Haard PMM, van den Bergh JP, Geusens PP (2015) Meeting international standards of secondary fracture prevention: a survey on Fracture Liaison Services in the Netherlands. Osteoporos Int 26(9):2257–2263
Akesson K et al (2013) Capture the fracture: a best practice framework and global campaign to break the fragility fracture cycle. Osteoporos Int 24(8):2135–2152
Kwon S (2003) Payment system reform for health care providers in Korea. Health Policy Plan 18(1):84–92
Kim L, Kim JA, Kim S (2014) A guide for the utilization of health insurance review and assessment service national patient samples. Epidemiol Health 36:e2014008
Kang HY, Yang KH, Kim YN, Moon SH, Choi WJ, Kang DR, Park SE (2010) Incidence and mortality of hip fracture among the elderly population in South Korea: a population-based study using the national health insurance claims data. BMC Public Health 10:230
Dafni U (2011) Landmark analysis at the 25-year landmark point. Circ Cardiovasc Qual Outcomes 5(3):363–371
Ryg J, Rejnmark L, Overgaard S, Brixen K, Vestergaard P (2009) Hip fracture patients at risk of second hip fracture: a nationwide population-based cohort study of 169,145 cases during 1977-2001. J Bone Miner Res 24(7):1299–1307
Brozek W, Reichardt B, Zwerina J, Dimai HP, Klaushofer K, Zwettler E (2016) Antiresorptive therapy and risk of mortality and refracture in osteoporosis-related hip fracture: a nationwide study. Osteoporos Int 27(1):387–396
Lee SH, Chen IJ, Li YH, Fan Chiang CY, Chang CH, Hsieh PH (2016) Incidence of second hip fractures and associated mortality in Taiwan: a nationwide population-based study of 95,484 patients during 2006-2010. Acta Orthop Traumatol Turc 50(4):437–442
Kanis JA et al (2012) A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 23(9):2239–2256
Lee YK, Ha YC, Choi HJ, Jang S, Park C, Lim YT, Shin CS (2013) Bisphosphonate use and subsequent hip fracture in South Korea. Osteoporos Int 24(11):2887–2892
Egan M, Jaglal S, Byrne K, Wells J, Stolee P (2008) Factors associated with a second hip fracture: a systematic review. Clin Rehabil 22(3):272–282
Sheikh HQ, Hossain FS, Khan S, Usman M, Kapoor H, Aqil A (2019) Short-term risk factors for a second hip fracture in a UK population. Eur J Orthop Surg Traumatol 29(5):1055–1060
Critchley RJ, Khan SK, Yarnall AJ, Parker MJ, Deehan DJ (2015) Occurrence, management and outcomes of hip fractures in patients with Parkinson’s disease. Br Med Bull 115(1):135–142
Katsoulis M, Benetou V, Karapetyan T, Feskanich D, Grodstein F, Pettersson-Kymmer U, Eriksson S, Wilsgaard T, Jørgensen L, Ahmed LA, Schöttker B, Brenner H, Bellavia A, Wolk A, Kubinova R, Stegeman B, Bobak M, Boffetta P, Trichopoulou A (2017) Excess mortality after hip fracture in elderly persons from Europe and the USA: the CHANCES project. J Intern Med 281(3):300–310
Wehren LE, Hawkes WG, Orwig DL, Hebel JR, Zimmerman SI, Magaziner J (2003) Gender differences in mortality after hip fracture: the role of infection. J Bone Miner Res 18(12):2231–2237
Berry SD, Samelson EJ, Hannan MT, McLean RR, Lu M, Cupples LA, Shaffer ML, Beiser AL, Kelly-Hayes M, Kiel DP (2007) Second hip fracture in older men and women: the Framingham Study. Arch Intern Med 167(18):1971–1976
Acknowledgments
This study was supported by the Korean Society for Bone and Mineral Research. This study used the National Health Insurance Database (NHIS-2019-1-169) of the National Health Insurance Service (NHIS).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study protocol was approved by the institutional review board (IRB) of Wonkwang University Sanbon Hospital (IRB No. WMCSB 201706-64). The requirement for informed consent was waived because the study was based on routinely collected administrative and claims data.
Conflict of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yoo, JI., Kim, HY., Jang, S. et al. Risk factors for subsequent hip fractures and fatality after an initial hip fracture in Korea: using nationwide claims data. Arch Osteoporos 15, 165 (2020). https://doi.org/10.1007/s11657-020-00820-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-020-00820-6