Abstract
Summary
Between 1 and 2% of people aged 50 years and over living at home in France are likely to experience a fragility fracture each year. Three-quarters of these individuals are not diagnosed with osteoporosis and lose the opportunity for appropriate care.
Purpose
To estimate the incidence of fragility fractures in France and to describe the characteristics of individuals with such fractures and of their fractures.
Methods
In April–May 2018, a postal survey was performed in France targeting a representative panel of 15,000 individuals aged ≥ 50 years, who were invited to complete a questionnaire. If they reported experiencing a fracture in the previous 3 years, they were asked to provide information on demographics, fracture type, risk factors for fractures and osteoporosis diagnosis. Only fragility fractures were considered, and these were classified as major (associated with increased mortality) or minor, based on the fracture site.
Results
Around 13,914 panellists returned an exploitable questionnaire (92.8%). About 425 participants reported ≥ 1 fragility fracture (453 fractures), corresponding to a 12-month incidence rate of 1.4% [95%CI: 1.2, 1.6]. Incidence was higher in women (1.99% [1.87, 2.05]) than in men (0.69% [0.38, 0.86]) and increased with age. Around 157 fractures (34.6%) were classified as major. Participants reporting major fractures were older than those reporting minor fractures (mean age: 72.6 ± 11.3 vs 67.1 ± 10.6) and more likely to report previous corticosteroid use (odds ratio: 1.90 [95%CI: 1.13, 3.18]). No other patient characteristic was associated with fracture severity. About 117 participants with fractures (27.5%) had undergone bone densitometry, and 97 (22.8%) declared having received a diagnosis of osteoporosis.
Conclusions
Around 340,000 people aged ≥ 50 years living at home in France are estimated to experience osteoporotic fractures each year. However, > 75% of panellists reporting fractures were never diagnosed with osteoporosis and thus did not have the opportunity to receive appropriate care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Low-trauma fragility fractures due to osteoporosis are an important health issue in people aged 50 years and over, due to their impact on morbidity, mortality and quality of life. It has been estimated that around nine million fragility fractures occur each year worldwide and that approximately 200 million individuals have osteoporosis [1]. In the European Union, almost four million osteoporotic fractures were estimated to have occurred in 2010, at a cost of around €40 billion to the health services [2, 3]. Such fractures are associated with potential loss of autonomy and long-term disability [4,5,6]. Certain fracture types, identified as major or severe fractures, are associated with increased mortality [7], irrespective of the age or gender of the individual concerned. Such major fracture sites include the hip, vertebra, pelvis, distal femur, proximal tibia, three or more simultaneous ribs and proximal humerus [7].
Little data on the epidemiology of fragility fractures are available from France, and most of what is available is over 20 years old. The first such study, EPIDOS [8], was a prospective cohort study of hip fracture conducted between 1992 and 1995 in 7575 elderly women aged over 75 years, which provided an annual incidence rate of 2.0%. Around the same time (1992–1993), the OFELY study [9] followed prospectively a cohort of 1039 postmenopausal women and identified an annual incidence rate for any osteoporotic fracture of 2.1%. A subsequent analysis of data from the French national hospitalisation database (PMSI) in 2001 reported 118,839 fractures requiring hospitalisation, principally of the hip (61%), distal radius (28%) and proximal humerus (11%), with a gender ratio of one man to four women [10]. However, these studies were performed before 2006, when densitometry for diagnosis of osteoporosis and specific anti-osteoporotic treatments were reimbursed for the first time in France for individuals who were at risk for osteoporotic fractures. The first French guidelines on the prevention, diagnosis and treatment of osteoporosis were published the same year [11]. More recently, the number of incident fractures in France was estimated to be around 380,000 in 2017 [12], although it should be noted that this estimate was based on extrapolations from previous data on the incidence of hip fracture only.
It is thus important to acquire up-to-date information on the incidence of fragility fractures generally associated with osteoporosis and in particular of severe or major fractures which are associated with increased mortality and disability irrespective of demographic group [7]. The EPIFRACT study was implemented in order to contribute to filling this gap in knowledge.
The objectives of the EPIFRACT study were to estimate the number of individuals in France with fragility fractures in the previous 3 years, to describe the characteristics of participants with a recent history of fragility fractures, to assess the impact of fragility fractures on quality of life and to evaluate the extent of diagnosis of osteoporosis. In addition, the study aimed to compare the characteristics of participants with a recent history of major versus minor fractures.
Methods
The EPIFRACT study was performed as a postal survey in a representative sample of the French general population. The fieldwork lasted for 5 weeks in April–May 2018. The survey was implemented by Kantar Health (Paris, France), an international healthcare market research organisation. A Scientific Committee was appointed to oversee the design and implementation of the study and to advise on data handling and interpretation.
Participants
Study participants were members of the METASKOPE panel, a permanent sample of 20,000 households constituted on a voluntary basis to answer regular questionnaires related to health or other topics of interest. It is selected to be representative of the French population by quotas, based on the distributions of age class, gender, occupational class, region and population size of municipality of residence, according to the French national statistics office. Participation in the panel is limited to 10 years, and members who repeatedly fail to reply to questionnaires or no longer wish to participate are replaced on a regular basis. When individuals join the panel, extensive sociodemographic data are collected. Each month, members of the panel are sent a questionnaire to complete on one or more subjects. Members receive ‘fidelity points’ for completing questionnaires, which can be exchanged for gifts at the end of each year. This panel has been used widely in medical research to collect medical data, for example, in the regular ObEpi studies of the epidemiology of obesity in France [13], and has provided reliable information consistent with that obtained from other sources [14, 15].
In the EPIFRACT study, a questionnaire was sent to 15,000 panellists in households with at least one member aged ≥ 50 years. If more than one household member was aged ≥ 50 years, then each was invited to complete a questionnaire. The questionnaire only contained the questions about fragility fractures specifically developed for the EPIFRACT study. The study questionnaire was sent by post and addressed by name.
Data collection
The study questionnaire consisted of up to 62 questions (Supplementary Material on-line – Table 1). Responses were elicited in the form of multiple-choice replies in the majority of cases, although some questions provided the possibility of free-text replies. Participants were asked whether they had experienced a fracture in the previous 3 years. Participants responding that this was not the case terminated the questionnaire at this point. The remaining participants then answered a further series of questions on the nature of the fracture, fracture management, quality of life, risk factors and osteoporosis. For participants who had experienced more than one fracture, they were asked to document each, up to a maximum of three.
In order to distinguish fragility fractures from traumatic fractures, participants were asked in what circumstances the fracture had occurred. Four responses were possible, namely, (1) falling over, (2) spontaneous fracture without trauma, (3) result of an accident on a public highway or (4) another circumstance, which the participant was asked to provide in the form of free text. Participants responding (1) or (2) were considered to have fragility fractures, those responding (3) were considered not to have fragility fractures and participants responding (4) were adjudicated individually by the Scientific Committee of the study. Fractures of the feet, hands, head or neck were not considered to be fragility fractures. Fragility fractures were then subdivided into major and minor fractures. Fractures to the humerus, vertebrae, pelvis, hip or femur and concurrent fracture of three or more ribs were considered to be major fractures. It should be noted that in the classification of Bliuc et al. [7], fractures to the proximal tibia are considered to be major fractures and those to the shaft or distal tibia as minor ones. However, given that it was considered that respondents may not be able to distinguish the site of the fracture with sufficient precision, all fractures to the tibia were classified as minor. In cases where a respondent indicated having more than one fracture site for the same fracture event, the following rule was applied: if at least one fracture site was major, then the event is classified as major, if not the event is classified as minor.
Participants were asked if, at the time of the survey, they were suffering from any of a prespecified list of comorbid illnesses. Certain comorbidities on this list were considered by the Scientific Committee to be potentially related to osteoporosis (Supplementary Material on-line – Table 2). They also reported whether they presented any of a list of risk factors for osteoporosis established by the Scientific Committee (Supplementary Material on-line – Table 2).
Data on health-related quality of life (QoL) was collected with the five-level five-dimension EuroQoL quality of life profile (EQ-5D-5L) [16, 17]. Participants were asked to evaluate their quality of life as they recalled it at two previous time points: first, before the oldest fracture described during the 3-year study period and, second, 1 year after the most recent one (if the fracture had occurred less than 1 year prior to the survey, they were asked to rate their quality of life on the day of the survey). At the time that the survey was conducted, there was no valuation set for EQ-5D-5L. As recommended by NICE, utility values for the EQ-5D-5L were derived from the existing EQ-5D-3L valuation set with the crosswalk method using a validated mapping function [18]. This quality of life profile assesses five aspects of QoL (mobility, self-care, usual activities, pain or discomfort and depression or anxiety) on five-point Likert scales. The profile of responses can be used to generate a linear, continuous utility measure ranging from − 1 to 1. The EQ-5D also provides a measure of overall perception of QoL on a visual analogue scale, yielding a score ranging from 0 (worst health that the respondent can imagine) to 100 (best health that the respondent can imagine).
Statistical analysis
In order to ascertain the representativeness of the sample, sociodemographic variables were compared to the structure of the French general population aged ≥ 50 years in 2017. These reference data were obtained from the French national statistics office (INSEE) [19]. The structure of the study sample was adjusted by weighting using raking adjusted statistics [20] to ensure matching of the survey sample and the general population in terms of sociodemographic characteristics and in order to produce extrapolated figures for the country as a whole.
For the analysis of the characteristics of participants with a history of fractures and of the fractures themselves, participants reporting more than one fracture event in the 3 years preceding the survey were excluded. The rationale underlying this decision was to avoid ambiguity over which fracture event was being described for variables relating to before or after the fracture (such as diagnosis or quality of life). Missing data were not replaced. Categorical variables were compared with the χ2 test or Z-test, as appropriate. Quantitative variables were compared using student’s t test or analysis of variance (ANOVA). Associations between comorbidities or risk factors on the one hand and a recent history of major as opposed to minor fractures in the previous 3 years on the other were expressed as odds ratios (OR) with their 95% confidence interval (95% CI).
Data were controlled, validated and analysed centrally. Data were analysed using Daisie software Version 2.4.84 (ADN SAS, Paris, France) for descriptive and bivariate analyses. Multivariate analysis was performed using R for Windows version 3.0.1 i386 software (R Foundation for Statistical Computing, Vienna, Austria).
Ethics
The survey was conducted in accordance with the ESOMAR International Code on Market and Social Practice, the EphMRA Code of Conduct, relevant current French and European legislation and good epidemiological practice guidelines. Analyses performed using the Kantar Health panel have been approved by the Commission Nationale de l’Informatique et des Libertés (CNIL). In addition, before answering the questionnaire, panellists had to confirm their agreement for the collection and analysis of data about their health.
Results
Study sample
A total of 14,153 (94.4%) members of the panel returned a study questionnaire. Of these questionnaires, 239 were eliminated because they were not completed (N = 68), because the participant did not wish to participate (N = 135) or because the questionnaire was not exploitable (N = 36). The remaining 13,914 (92.8%) were retained and formed the study sample.
Characteristics of participants
The characteristics of all participants are presented in the Supplementary Material on-line – Table 3. Compared to the French general population of individuals, subjects in the extreme age groups (< 55 years and > 75 years) somewhat are under-represented. The structure of the study sample was adjusted as described in the Methods to match the structure of the general population, and all the data presented in the remainder of the Results section are presented with respect to the adjusted study sample. Participants with multiple fracture events were comparable to those with single fracture events in terms of age and gender (data not shown).
History of fragility fractures
Overall, 767 participants (5.5%) reported having experienced at least one fracture in the previous 3 years. In 342 participants (44.6%), the cause of the fracture excluded a low-trauma origin. In the remaining 425 participants (55.4%), the fractures were classified as fragility fractures, corresponding to a 12-month incidence rate of 1.4% [95% CI, 1.2–1.6] for April 2017 to March 2018, 0.8% [0.7–1.0] for April 2016 to March 2017 and 0.9% [0.8–1.1] for April 2015 to March 2016. Four hundred of these respondents (94.1%) reported experiencing a single fracture only, and these constituted the analysis population for the characterisation of participants with fracture and their fractures.
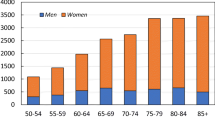
The 12-month incidence of fracture as a function of age and gender is presented for the period 2017–2018 in Fig. 1. Fracture rate increased with age and, for all age groups, was around threefold higher in women (1.99% [1.65–2.27]) than in men (0.69% [0.48–0.90]). No difference in fracture rate was observed as a function of present or previous occupational status or as a function of where the participants lived. The latter variable was dichotomised on the basis of the population size of the municipality of residence as rural (< 2000 inhabitants) or urban (> 2000 inhabitants).
Extrapolation of this frequency of fracture history of 1.4% to the total French population would suggest that around 344,000 individuals aged ≥ 50 years would experience a fragility fracture each year.
Characterisation of fragility fractures
Overall, 453 fragility fractures, as defined in the Methods, were reported by 425 participants. Fracture sites are displayed in Fig. 2. The most frequently reported sites were the forearm/wrist (24.7% of all fractures), the ankle (17.7%), the proximal humerus (10.6%) and ribs (10.6%). About 157 fractures (34.6%) reported by 147 participants were considered major fractures, principally fractures of the proximal humerus, vertebral and hip. The remaining 296 fractures (67.4%) reported by 287 participants were minor fractures. Twenty-five participants reported more than one fracture (5.6%).
Most of the 453 fragility fractures (373, 82.4%) resulted from falling over, with no significant differences (p = 0.20) between major (124/157, 78.9%) and minor (249/297, 83.8%) fractures. However, 53 (11.7%) fractures were reported to have happened spontaneously without trauma. This was notably the case for 14 of the 37 vertebral fractures (37.8%), 11 of the 37 fractures of 1 or 2 ribs (29.7%) and 6 of the 14 knee/kneecap fractures (42.9%).
Comparison of participants with a history of major and minor fragility fractures
This analysis and all further analyses presented in the Results section were performed on the 400 participants who reported only 1 fracture event in the previous 3 years. Participants reporting a recent history of major fractures were older at the time of the survey than those reporting minor fractures (Table 1). Notably, 58.3% of hip (14/24) and 50.0% of femur fractures (6/12) were reported by participants aged over 80, who accounted for < 20% of the study population. On the other hand, the two fracture types were similarly distributed with respect to gender and body mass index (Table 1), as well as with respect to occupation, living status (alone, with spouse, with family or with friends), region of residence and size of municipality (data not shown). Fractures of the humerus (29 of 43 humerus fractures; 68.7%), lower leg (17/23, 72.5%) and ankle (54/76, 70.7%) were over-represented in participants who were overweight or obese. In the case of ankle fractures, the difference in fracture frequency between overweight/obese participants and underweight/normal weight participants was significant (p = 0.014). Overall, 193 participants reporting fractures (48.3%) declared that they had lost height since they were 20 years of age, with a mean height loss of 2.98 ± 2.17 cm. The extent of height loss was higher in participants reporting major fractures compared to minor ones (Table 1).
Comorbidities and osteoporosis risk factors
Overall, 227 participants (56.7%) reported at least one comorbidity, of which the most frequent were hypertension (115 participants; 28.8%), depression (N = 42, 10.5%), asthma (N = 37, 9.2%), diabetes (N = 36, 9.0%) and chronic obstructive pulmonary disease (COPD; N = 26, 6.4%). None of these comorbidities were individually associated with an increased probability of reporting a major rather than a minor fracture (Table 2), nor was any association observed for the presence of any osteoporosis-related comorbidity (as defined by the Scientific Committee and listed in Supplementary Material – Table 2).
About 74 participants (18.5%) reported use of corticosteroids for at least 3 months at any time during their lives. This was more frequent in patients reporting a history of major fracture (Table 2) and was associated with an increased probability of reporting major fractures rather than minor ones (OR, 1.90). No association was observed between the use of antidepressants, tobacco or alcohol and the probability of reporting major rather than minor fractures. Falls in the previous year were reported by 152 participants (38.0%) and a parental history of fragility fractures by 42 participants (10.5%). For neither of these variables was an association observed with an increased probability of reporting major rather than minor fractures (Table 2).
Most fractures were reported by women who were postmenopausal at the time of the survey (97 women with major fractures and 187 with minor fractures). Hormonal replacement therapy was more frequent in patients reporting a history of major fracture (Table 2), although this difference was not statistically significant (p = 0.06; χ2 test).
Osteoporosis diagnosis and treatment
Overall, 90 participants who reported a single fracture (22.5%) declared that they had osteoporosis and 89 (22.2%) that they had received a diagnosis of osteoporosis from a physician. This diagnosis had been made on average 6.0 ± 7.0 years before the survey and had been made by a rheumatologist in 43 cases (48.9%), by a general practitioner in 30 cases (33.7%) and by a gynaecologist in five cases (5.5%). In addition, 71 participants (17.8%) declared that they had undergone DXA following their fracture. About 42 participants (10.5%) reported taking a specific treatment for osteoporosis. Compared to men, women with a fracture history more frequently declared having received a diagnosis of osteoporosis (26.5% vs 8.6% respectively; p < 0.0001) and having undergone DXA (22.3% vs 5.1%; p = 0.0001). A diagnosis of osteoporosis was more frequently declared by participants reporting major versus minor fractures (31.1% vs 17.9%, respectively; p = 0.01), and participants with major fractures were also more likely to have undergone DXA (33.6% vs 22.6%; p < 0.001). The diagnosis was more often given by a rheumatologist in participants reporting major fractures than in those with minor ones (60.5% of those diagnosed vs 39.3%; p = 0.035).
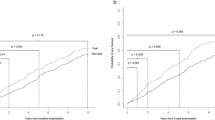
Quality of life
Mean scores on the EQ-5D utility score are presented in Table 3. Before the fracture, participants who would experience a major fracture rated their QoL somewhat lower than those who would experience a minor one (Table 3). After the fracture, this difference persisted and was even amplified. For all fractures combined, the mean change in EQ-5D score between before and after the fracture was − 0.14 ± 0.25. This change was significantly greater in participants reporting major versus minor fractures (p = 0.001). The EQ-5D items which were the most deteriorated by the occurrence of a fracture were the pain/discomfort item and the usual activity item (Fig. 3).
Discussion
In this survey of people living at home in France aged at least 50 years, the reported annual frequency of incident fragility fractures was 1.4% in 2017. Extrapolated to the total French population, this would suggest that around 344,000 individuals aged ≥ 50 years would experience a fragility fracture each year. The reported frequency of fragility fractures in the previous 2 years was somewhat lower, and the reason for this unanticipated finding may be related to the relatively high 1-year mortality associated with certain fractures, such as hip fractures [21], or the possibility that participants may move to sheltered accommodation such as a nursing home after the occurrence of a fracture and thus no longer be in the study panel. In addition, the possibility of recall bias cannot be excluded. Only 5.6% of the sample reported having experienced multiple fragility fracture events, which seems low compared to published reports of a refracture rate of around 3% of patients per year [22]. However, this is likely to be an underestimate, since fractures were only documented over a 3-year period, and earlier antecedents of fracture will not have been captured.
This incidence rate is somewhat lower than that reported in the EPIDOS study, where the annual incidence of hip fracture alone was 2.0% [8]. However, in EPIDOS, the population was considerably older (minimum age, 75; mean, 80.5) than in EPIFRACT, which could have contributed to this discrepancy, particularly as 58% of the observed hip fractures occurred in participants over 80 years old in the EPIFRACT study. In OFELY [9], the reported incidence rate for any osteoporotic fracture in postmenopausal women was 2.1%, which is consistent with the value obtained for women in EPIFRACT (2.0%). In addition, the current estimation of the number of fractures occurring each year in France is very similar to that of the extrapolated value of 380,000 for 2017 published in the International Osteoporosis Foundation (IOF) report [12].
In 2010, the French Public Health Surveillance agency (InVS) conducted an exhaustive nationwide survey of individuals aged 55–85 years who had experienced a fall in the previous 12 months, using a range of data sources [23]. This study reported that 7.8% of the survey population had experienced a fall, of which 37% resulted in fractures (prevalence of fracture: 2.9%). The findings of the EPIFRACT study are again somewhat lower than this estimation.
With respect to the characteristics of the sample reporting fragility fractures in EPIFRACT, one in four individuals were men, an identical gender ratio to that reported for hospitalisations due to hip fracture in the InVS study [23]. The proportion of individuals reporting any of the more frequent comorbidities was no higher than would be expected in individuals of this age range in the general population [24,25,26,27,28], except perhaps for asthma [29].
Around one in five participants reporting a fracture had a history of corticosteroid use, which is a major risk factor for osteoporotic fractures [30]. This proportion is twice as high as the proportion of previous corticosteroid users among all postmenopausal women aged over 45 (10.5%) identified using an identical definition in the INSTANT study [31]. Such findings highlight the importance of corticosteroid use as a risk factor for osteoporosis and emphasise the need for elderly people with such a history to undergo DXA and receive an appropriate preventive treatment should osteoporosis be diagnosed, as recommended in current French guidelines [32, 33].
Around one-third of reported fragility fractures were considered major fractures. Extrapolated to the total French population, this would indicate that around 119,000 people over 50 would be expected to have a major fracture each year. Major fractures would be expected to carry the highest burden of disability and are associated with the highest mortality [7]. For this reason, the proportion of major fractures may be underestimated if a significant number of these participants die or move to nursing homes. Similarly, subjects who are disabled due to a major fracture (or for any other reason) may be less likely to participate in the METASKOPE panel.
The most frequent major fractures were shoulder, vertebra and hip fractures, and the most frequent minor fractures were those of the forearm/wrist and ankle. Major fractures were more frequently reported in the older age groups, with over half the hip and femur fractures being reported by participants aged over 80. The only variable that was significantly associated with a history of major fractures, compared with minor fractures, was previous corticosteroid use. It could be speculated that this association is due to a reduction in bone density as a direct result of the corticosteroid treatment.
In this study population of individuals reporting at least one fragility fracture in the previous 3 years, only 29.3% declared having their bone mineral density evaluated by DXA. Since 2006, French national guidelines for DXA have recommended that this be reimbursed for people with fragility fractures so that osteoporosis can be diagnosed and treated if necessary [33]. This shows that 10 years after these guidelines were issued and since DXA has been fully reimbursed by public health insurance, these recommendations are not followed in two-thirds of cases. The unmet need is particularly striking for men, since only one in ten men with fragility fractures declared that they had been diagnosed with osteoporosis.
The change in the mean EQ-5D utility index following a fall in participants reporting a major fracture at least 10 years previously was − 0.23 points, which would be considered well above the minimally important clinical difference on this scale determined in the majority of studies that have assessed this [34]. Other studies have reported that the reduction in quality of life following hip and vertebral fractures persists for at least 18 months [35].
The EPIFRACT study has several strengths and limitations. The strengths include the large number of individuals sampled, the very comprehensive nature of the questionnaire, the high response rate (> 95%) and the general population context of the study. Limitations include the unknown reliability of self-report for medical variables in this elderly population and the lack of clinical ascertainment of the information collected. Also, information of risk factors and comorbidities was collected at the time of the survey and not at the time of fracture. In addition, the study sample was limited to people living at home, and individuals who may have died or moved into residential care after experiencing a fracture will not have been captured. Nonetheless, the findings obtained have good face validity (e.g. the relationship between fracture rate and age or gender and the relationship between lower leg fractures and obesity). Elderly people living in residential homes or nursing homes may present a different fracture risk to independent individuals living at home, and for this reason, the above extrapolations should be considered as approximations to the expected number of fractures in the general population. In addition, in the absence of a control group, it is not possible to evaluate the relative importance of any possible fracture risk factors. Finally, the data obtained on quality of life should be interpreted with caution, since these were collected retrospectively. The ED-5Q was developed and validated to assess current quality of life [16, 17] and has not been explicitly validated for recalled quality of life. However, the EQ-5D has previously been usefully employed in the ICUROS study [36] for determining recalled quality of life prior to a fracture.
In conclusion, between 1 and 2 % of all individuals over the age of 50 living at home in France may expect to experience a fragility fracture in any year. In spite of their fracture history and the presence of other osteoporosis risk factors such as corticosteroid exposure, individuals evaluated in this study are frequently neither diagnosed with osteoporosis nor treated and thus miss the opportunity to receive appropriate care. General practitioners need to consider a diagnosis of osteoporosis systematically in individuals experiencing fragility fractures, to assess and take into account osteoporosis risk factors and to ensure adequate anti-osteoporotic treatment.
References
Pisani P, Renna MD, Conversano F, Casciaro E, Di Paola M, Quarta E, Muratore M, Casciaro S (2016) Major osteoporotic fragility fractures: risk factor updates and societal impact. World J Orthop 7(3):171–181. https://doi.org/10.5312/wjo.v7.i3.171
Hernlund E, Svedbom A, Ivergard M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jonsson B, Kanis JA (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8:136. https://doi.org/10.1007/s11657-013-0136-1
International Osteoporosis Foundation (2018) Broken bones, broken lives: the fragility fracture crisis in six European countries. http://share.iofbonehealth.org/EU-6-Material/Reports/IOF%20Report_EU.pdf
Dyer SM, Crotty M, Fairhall N, Magaziner J, Beaupre LA, Cameron ID, Sherrington C (2016) A critical review of the long-term disability outcomes following hip fracture. BMC Geriatr 16:158. https://doi.org/10.1186/s12877-016-0332-0
Al-Sari UA, Tobias J, Clark E (2016) Health-related quality of life in older people with osteoporotic vertebral fractures: a systematic review and meta-analysis. Osteoporos Int 27(10):2891–2900. https://doi.org/10.1007/s00198-016-3648-x
Martin AR, Sornay-Rendu E, Chandler JM, Duboeuf F, Girman CJ, Delmas PD (2002) The impact of osteoporosis on quality-of-life: the OFELY cohort. Bone 31(1):32–36
Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR (2009) Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. Jama 301(5):513–521. https://doi.org/10.1001/jama.2009.50
Dargent-Molina P, Favier F, Grandjean H, Baudoin C, Schott AM, Hausherr E, Meunier PJ, Breart G (1996) Fall-related factors and risk of hip fracture: the EPIDOS prospective study. Lancet 348(9021):145–149
Albrand G, Munoz F, Sornay-Rendu E, DuBoeuf F, Delmas PD (2003) Independent predictors of all osteoporosis-related fractures in healthy postmenopausal women: the OFELY study. Bone 32(1):78–85
Maravic M, Le Bihan C, Landais P, Fardellone P (2005) Incidence and cost of osteoporotic fractures in France during 2001. A methodological approach by the national hospital database. Osteoporos Int 16(12):1475–1480
Haute Autorité de Santé (2003) Prévention, diagnostic et traitement de l’ostéoporose
International Osteoporosis Foundation (2018) Os brisés, vies brisés: une feuille de route pour résoudre la crise des fractures de fragilité en France. http://share.iofbonehealth.org/EU-6-Material/Reports/IOF%20Report_EU.pdf
Charles MA, Eschwege E, Basdevant A (2008) Monitoring the obesity epidemic in France: the Obepi surveys 1997-2006. Obesity (Silver Spring, Md) 16(9):2182–2186. https://doi.org/10.1038/oby.2008.285
Reach G, Pellan M, Crine A, Touboul C, Ciocca A, Djoudi Y (2018) Holistic psychosocial determinants of adherence to medication in people with type 2 diabetes. Diabetes Metab 44(6):500–507. https://doi.org/10.1016/j.diabet.2018.06.001
Mosnier-Pudar H, Hochberg G, Eschwege E, Halimi S, Virally ML, Guillausseau PJ, Touboul C, Dejager S (2010) How patients’ attitudes and opinions influence self-care behaviours in type 2 diabetes. Insights from the French DIABASIS survey. Diabetes Metab 36(6 Pt 1):476–483. https://doi.org/10.1016/j.diabet.2010.08.004
EuroQol – a new facility for the measurement of health-related quality of life (1990). Health policy (Amsterdam) 16 (3):199–208
Devlin NJ, Brooks R (2017) EQ-5D and the EuroQol group: past, present and future. Applied health economics and health policy 15(2):127–137. https://doi.org/10.1007/s40258-017-0310-5
van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D, Lloyd A, Scalone L, Kind P, Pickard AS (2012) Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health 15(5):708–715. https://doi.org/10.1016/j.jval.2012.02.008
Institut National de la Statistique et des Etudes Economiques (2018) Bilan démographique:2017
Deville J-C, Sarndal C-E, Sautory O (1993) Generalized raking procedures in survey sampling. J Am Stat Assoc 88(423):1013–1020
Oberlin P, Mouquet M-C (2016) Quel risque de décès un an après une fracture du col du fémur ? Etudes et Résultats 0948:1–6
Center JR, Bliuc D, Nguyen TV, Eisman JA (2007) Risk of subsequent fracture after low-trauma fracture in men and women. Jama 297(4):387–394. https://doi.org/10.1001/jama.297.4.387
Thélot B, Lasbeur L, Pédrono G (2017) La surveillance épidémiologique des chutes chez les personnes âgées. Bull Epidemiol Hebd 16-17:328–335
Bringer J, Fontaine P, Detournay B, Nachit-Ouinekh F, Brami G, Eschwege E (2009) Prevalence of diagnosed type 2 diabetes mellitus in the French general population: the INSTANT study. Diabetes Metab 35(1):25–31. https://doi.org/10.1016/j.diabet.2008.06.004
Fagot-Campagna A, Romon I, Fosse S, Roudie C (2010) Prévalence et incidence du diabète, et mortalité liée au diabète en France – Synthèse épidémiologique. Institut de veille sanitaire, St Maurice
Lepine JP, Gasquet I, Kovess V, Arbabzadeh-Bouchez S, Negre-Pages L, Nachbaur G, Gaudin AF (2005) Prevalence and comorbidity of psychiatric disorders in the French general population. L'Encephale 31(2):182–194
Bénard E, Detournay B, Neukirch F, Pribil C, El Hasnaoui A (2005) Prévalence de la bronchopneumopathie chronique obstructive (BPCO) : estimation pour la France. Lett Pneumol 8(4):158–163
Perrine AL, Lecoffre C, Blacher J, Olié V (2018) L’hypertension artérielle en France : prévalence, traitement et contrôle en 2015 et évolutions depuis 2006. Bull Epidémiol Hebd 10:170–179
Delmas MC, Leynaert B, Com-Ruelle L, Annesi-Maesano I, Fuhrman C (2008) Asthme : prévalence et impact sur la vie quotidienne. Analyse des données de l’enquête décennale santé 2003 de l’Insee. Institut National de veille sanitaire, St Maurice
Briot K (2018) Bone and glucocorticoids. Ann Endocrinol 79(3):115–118. https://doi.org/10.1016/j.ando.2018.04.016
Roux C, Fardellone P, Lespessailles E, Cotte FE, Mercier F, Gaudin AF (2008) Prevalence of risk factors for referring post-menopausal women for bone densitometry. The INSTANT study. Joint Bone Spine 75(6):702–707
Briot K, Paccou J, Beuzeboc P, Bonneterre J, Bouvard B, Confavreux CB, Cormier C, Cortet B, Hannoun-Levi JM, Hennequin C, Javier RM, Lespessailles E, Mayeur D, Artus PM, Vieillard MH, Debiais F (2018) French recommendations for osteoporosis prevention and treatment in patients with prostate Cancer treated by androgen deprivation. Joint Bone Spine. https://doi.org/10.1016/j.jbspin.2018.09.017
Haute Autorité de Santé (2006) Ostéodensitométrie [absorbimétrie osseuse] sur 2 sites par methode biphotonique. HAS, Paris
Coretti S, Ruggeri M, McNamee P (2014) The minimum clinically important difference for EQ-5D index: a critical review. Expert Rev Pharmacoecon Outcomes Res 14(2):221–233. https://doi.org/10.1586/14737167.2014.894462
Svedbom A, Borgstom F, Hernlund E, Strom O, Alekna V, Bianchi ML, Clark P, Curiel MD, Dimai HP, Jurisson M, Kallikorm R, Lember M, Lesnyak O, McCloskey E, Sanders KM, Silverman S, Solodovnikov A, Tamulaitiene M, Thomas T, Toroptsova N, Uuskula A, Tosteson ANA, Jonsson B, Kanis JA (2018) Quality of life for up to 18 months after low-energy hip, vertebral, and distal forearm fractures-results from the ICUROS. Osteoporos Int 29(3):557–566. https://doi.org/10.1007/s00198-017-4317-4
Svedbom A, Borgstrom F, Hernlund E, Strom O, Alekna V, Bianchi ML, Clark P, Curiel MD, Dimai HP, Jurisson M, Uuskula A, Lember M, Kallikorm R, Lesnyak O, McCloskey E, Ershova O, Sanders KM, Silverman S, Tamulaitiene M, Thomas T, Tosteson ANA, Jonsson B, Kanis JA (2018) Quality of life after hip, vertebral, and distal forearm fragility fractures measured using the EQ-5D-3L, EQ-VAS, and time-trade-off: results from the ICUROS. Qual Life Res 27(3):707–716. https://doi.org/10.1007/s11136-017-1748-5
Funding
The study was jointly conducted and funded by the AFLAR, Amgen and UCB Pharma S.A., France, who initiated the study and supervised its implementation and the exploitation of the findings, including the preparation of this manuscript. Editorial support was provided by Foxymed, funded by UCB Pharma S.A.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
JMJ and BV are employees of UCB Pharma S.A., France. BC has received consultancy honoraria of speaker’s fees from Amgen, Expanscience, Ferring, Lilly, Medtronic, MSD, Novartis, Roche diagnostics, Théramex and UCB Pharma S.A. JMF has received consultancy honoraria and conference fees from UCB Pharma S.A., Amgen and Lilly. LG has received honoraria from Amgen, Lilly and UCB Pharma S.A. and research support from Lilly, Amgen, UCB Pharma, Expanscience, Mylan, Roche diagnostics and TEVA. KB has received consultancy honoraria and conference fees from UCB Pharma S.A., Amgen, Lilly and MSD. No other authors report conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 22 kb)
Rights and permissions
About this article
Cite this article
Cortet, B., Chauvin, P., Feron, JM. et al. Fragility fractures in France: epidemiology, characteristics and quality of life (the EPIFRACT study). Arch Osteoporos 15, 46 (2020). https://doi.org/10.1007/s11657-019-0674-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-019-0674-2