Abstract
Summary
Trabecular bone score (TBS) is a tool to improve evaluation of DXA scans, barely used in children. We proposed to evaluate TBS with bone age (BA) compared to chronological age (CA). In girls, TBS value using BA is constant until age 8, and in boys until age 10, and then starts to increase steadily. This data may help widen TBS use in pediatric populations.
Introduction
Trabecular bone score (TBS) is a software-based tool for the analysis of DXA images to assess bone microarchitecture in the lumbar region. It is used widely in adults to improve evaluation of fracture risk, yet it has been rarely studied in children and no normal curves have been developed for pediatrics. The purpose of this study was to evaluate bone (skeletal) age compared to chronological age to determine which is better in the pediatric population since both bone age (BA) and trabecular density are equally susceptible to change in response to similar factors.
Methods
Total body, lumbar region, and non-dominant hand scans were obtained with an iDXA device in all participants. DXA scans of lumbar region for TBS analysis and AP images of non-dominant hand-for-BA were obtained for 565 children (269 female) aged 4to 19.
Results
Simple correlation was calculated and r2 values for TBS and chronological age were obtained by linear regression, with low correlations (0.36 for boys and 0.38 for girls), and then we created Loess curves to show the change for consecutive ages. In girls, the curve forms a U shape with a nadir point at approximately age 10. We then replaced chronological age with BA, and significant change was seen in the girls’ curve, where a turning point is seen at age 8. In boys, a similar trend shows a turning point at age 10. Finally, BA-corrected TBS curves were constructed using LMS, obtaining curves with percentiles.
Conclusions
The use of BA in the analysis and interpretation of TBS may help widen its use in pediatric populations by enabling the appearance of normative data, but more information is needed to confirm this finding.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the last few decades, research in children with DXAhas greatly increased knowledge regarding bone physiology during growth and has led to the development of keystone concepts such as peak bone mass and peak bone mineral content increase during puberty [1]. The International Society for Clinical Densitometry (ISCD) 2014 pediatric position regarding interpretation and reporting of DXA [2, 3] recommends that, when possible, country-specific reference values should be used, and such values for children and adolescents have been reported for several countries. Puberty is of the greatest relevance in this age group; therefore, several methods for adjustment have been based on the child’s height, bone size, and Tanner stage. Besides Tanner stage, ISCD also suggests bone age (BA) adjustment as another method to be considered for interpretation of results in some clinical situations, especially when a significant BA delay is expected [3], but little information has been published using BA for adjustment and analysis.
Although DXA has been used extensively as a proxy of skeletal status, it has been also recognized that it does not account for all the parameters needed. Trabecular bone score (TBS) was developed to evaluate the trabecular bone: It is a software-based tool for the analysis of DXA images to assess bone microarchitecture in the lumbar region. It analyzes images directly from DXA raw data by evaluating pixel gray-level variations of the 2D projection image. By taking such variation and the pixels’ distance into account [4], DXA image texture is then linked to the texture of the projected bone as it has been shown on several steps of validation, including finite element analysis [5] and case-control studies [6].
Large cross-sectional and longitudinal studies have addressed TBS value in adult populations as an aid to improve fracture risk evaluation [7]. ISCD has issued a position statement in 2015 regarding the applicability and limitations of TBS in adult populations [8]. However, despite the rationale behind the benefits that TBS may add to bone density studies in young patients, few studies have been published or have presented data on pediatric populations. In some of them, the commercially available versions of TBS software (adjusted for adults) have been used to analyze particular groups of children [9, 10]; in others, small groups of patients were analyzed with a customized version of the TBS software [11,12,13,14,15]. In all of them, TBS values describe U-shaped curves when an LMS algorithm is applied to smoother the curve. Such a U shape appears in two studies in girls and in one study in boys. In a study designed to create normative data with a larger population, Del Rio et al. [16] again found U-shaped curves in both genders. The common feature in most of these studies is that data were not adjusted for puberty. The exception was Shawwa et al. [15], in which they grouped participants according to Tanner stage, and TBS scores seemed to increase from stage III in girls and IV in boys (Table 1). The purpose of this study is to determine whether such a U-shaped curve is an artifact related to TBS methodology or a novel biological phenomenon related to trabecular bone and detected by TBS.
According to ISCD recommendations, bone or skeletal age is recommended for evaluating skeletal maturation using a well-established pattern of ossification center appearance in long bone epiphyses or short bones. This method has largely been determined using an anteroposterior x-ray image of the non-dominant hand [17]. In 1976,Tanner and Whitehouse established that pubertal stages, including the growth spurt, correlate better with BA than with chronological age both in boys and girls, given the considerable variation in maturation onset ages [18]. In our work, we decided to use BA as another factor for analysis.
Methods
Study design:cross-sectional
Study population
Healthy children of both sexes aged 4–19 years from a subsample of those currently being recruited at the Clinical Epidemiology Unit, Hospital Infantil de México Federico Gómez, for a body composition reference values study were invited to participate. Written consent was obtained from their parents and assent was obtained from children 8 years and over before performing DXA scans. The sample used for this analysis was balanced to get enough numbers for each chronological year as well as to allow for sex comparisons. Lumbar region and non-dominant hand scans were obtained separately with an iDXA (GE Healthcare, Madison, WI) in all participants. Pseudo volumetric lumbar BMD (3D BMD) was calculated based on cylindrical model proposed by Kröger et al. [19]. TBS assessment was conducted with a custom version of TBS (Med-Imaps SASU, France) that includes a dedicated soft tissue correction for pediatric subjects based on exvivo data and considering spinal tissue thickness and acquisition mode. Hand skeletal images were interpreted by a single pediatric endocrinologist using Greulich and Pyle Atlas [17] blinded to the chronological age of the child. DXA-obtained images to calculate BA have been validated previously by other groups [20].
Statistical analysis
It was generated by SPSS v.21. The LMS statistical method proposed by Cole and Green [21] was used to construct TBS BA-related curves using Cole’s LMS smoother module in R.
Results
DXA scans of lumbar region for TBS analysis and AP images of the non-dominant hand for BA were obtained for 565 children (269 females) aged 4–19 years (Table 2). Data were collected and images were analyzed with a custom TBS version as previously described.
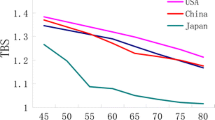
Simple correlation was calculated and r2 values for TBS and chronological age were obtained by linear regression, with low correlations (0.36 for boys and 0.38 for girls). In a more detailed analysis, we used a Loess curve to show the change for consecutive ages. When only chronological age was used, the Loess curve in girls forms a U-shaped curve with a nadir point at approximately age 10, which then starts to increase steadily. In boys, no U shape is seen, and there is only an inflection by age 11 (Fig. 1a,b). Such a U shape resembles those obtained in previous works.
As a second step, we replaced chronological age with BA, and significant change is seen in the girls’ Loess curve (Fig.1c,d), where a turning point is seen at age 8followed by a steady and marked increase until age 19. In boys, the same trend is seen but the turning point appears at age 10, and the curve is slightly more linear with a less-marked slope than in girls.
Finally, TBS curves were constructed using the LMS statistical method proposed by Cole and Green [21]. These were drawn using percentiles 3, 5, 10, 25, 50, 75, 90, 95, and 97 using CA as shown in Fig. 2 and using BA in Fig. 3. The latter are proposed as a method to obtain normal values in pediatric population and may also be seen as mean and SD by age in Table 3.
Discussion
TBS may be a useful and convenient method to evaluate trabecular bone in children.This tool is likely particularly relevant in children with skeletal pathologies from underlying endocrine, metabolic or kidney disease, transplant recipients, among others. However, reference values for each population need to be developed to be useful. Several studies that have reported TBS reference values for a particular group of children and adolescents have found their data difficult to interpret since a U-shaped curve (accentuated among girls) is a common finding. We hypothesized that using BA as a correction factor would yield a more accurate analysis. Therefore, the present study was aimed at presenting the TBS reference values in Mexican children using BA as a correction factor, taking the ISCD recommendations into account. We propose a novel approach using BA instead of chronological age to adjust for the variation found in previous studies to obtain normative data for TBS in children.
The idea of using BA instead of chronological age to analyze TBS in children was conceived when we analyzed the previous failed attempts from other groups to obtain reference data, even those including tanner stage. This is because BA has a good relationship with physiological changes during this period of life because, even though normal puberty may present in diverse timing patterns in healthy children, BA correlates better with pubertal milestones. For example, the timing of pubertal events and the accelerated bone maturation rate associated with the rapid phase of growth are easily recognizable using BA, even though they may present at different ages [22].
The differences between Figs. 1 and 2 show the changes in loess curves when BA is used to adjust for pubertal stage (instead of chronological age). The latter seems to explain better a biological phenomenon. Chronological age of puberty onset may also be variable in both genders and show a wide range of maturational rates, from very early to very late bloomers (up to 5 years of difference) [23]. Puberty onset appears in girls at a BA of 8and in boys at a BA of 10, regardless of chronological age [24]. This is caused by the influence of sexual steroids in bone morphology from which BA is calculated. Therefore, BA better explains many of the hormonal influences of puberty onset as a single variable [25, 26]. It could be inferred that during growth, TBS reflects the crucial influence of sexual steroids at the beginning of puberty in the increase of trabecular complexity of the axial skeleton, which is what TBS texture analysis attempts to calculate. This phenomenon has been described with different bones (long extremities) and technologies (pQCT) in longitudinal studies in girls and in both genders [27, 28]. Unlike other technologies, TBS is widely available; it is a software that may be installed to any DXA equipment and is suitable to be used in research and clinical settings, which would improve diagnosis in pediatric populations. Normative data must be generated for TBS in pediatric populations in the same way they have been published for adult populations [29,30,31]. In the case of pediatric and adolescent populations, we have demonstrated that taking BA into account provides an accurate analysis that allows better understanding of the biological pubertal changes in adolescence.
There is a lack of information for adults between 20 and 30 years regarding TBS values. Information derived from healthy Caucasian American women starts at 30 years of age, and the average lumbar spine TBS in the youngest group (30–39 years old) was 1.382 [29]. Our study ends at individuals who were 19 years old, where the mean TBS found in girls age 19 was 1.628 ± 0.1. A recent cross-sectional study of 44 girls 1 year after menarche found that their TBS values are similar to those found in adult women, 1.352 on average [32], yet data are lacking as to whether this is the definitive peak value. This may indicate that a phenomenon similar to peak bone mass seen with BMD may happen also in TBS; however, until proven, this is just a hypothesis.
Until recently, BA analysis has been a manual process, with either a certain degree of interpersonal variability when using atlas methods or it is cumbersome and time consuming when using score-based methods. In our study, a single pediatric endocrinologist read the hand images blinded to chronological age, to control variability. The development of software tools that can automate such tasks improves both analysis time and reproducibility significantly. BoneXpert [33], developed in Denmark and validated in several populations of healthy children and in some with diverse diseases, may increase the availability and ease of use of BA in clinical practice [34].
The limitations of this study include selection of participants. This was made in a consecutive manner as an exploratory survey, but the sample was taken within a group of a population selected for a larger study, which attempts a better representation of the population. Additionally, age extremes are underrepresented in this sample, particularly in the young adult side where, considering that bone accretion phenomenon, which takes place until age 25–30 when peak bone mass is attained, it would add much to the information currently available about this phenomenon.We did not perform height Z-score or height for age analysis, although this was a healthy children study and no participants had height outside ± 2 Z-score.
Conclusion
TBS is a novel technology with proven utility for bone status evaluation in adults, but so far, it has rarely been used in children. The analysis and interpretation of BA may help widen its use in pediatric populations by enabling the appearance of normative data. Then TBS may be validated for evaluating children with diverse diseases that may affect bone health. This study adds a possible explanation for the apparent lack of biologic sense from the previously reported data in pediatric populations by using BA when analyzing TBS. More data are needed to confirm these findings.
References
Bachrach LK (2001) Acquisition of optimal bone mass in childhood and adolescence. Trends Endocrinol Metab 12(1):22–28
Gordon CM et al (2014) 2013 Pediatric position development conference: executive summary and reflections. J Clin Densitom 17(2):219–224
Crabtree NJ, Arabi A, Bachrach LK, Fewtrell M, el-Hajj Fuleihan G, Kecskemethy HH, Jaworski M, Gordon CM (2014) Dual-energy X-ray absorptiometry interpretation and reporting in children and adolescents: the revised 2013 ISCD pediatric official positions. J Clin Densitom 17(2):225–242
Pothuaud L, Porion P, Lespessailles E, Benhamou CL, Levitz P (2000) A new method for three-dimensional skeleton graph analysis of porous media: application to trabecular bone microarchitecture. J Microsc 199(Pt 2):149–161
Pothuaud L, Carceller P, Hans D (2008) Correlations between grey-level variations in 2D projection images (TBS) and 3D microarchitecture: applications in the study of human trabecular bone microarchitecture. Bone 42(4):775–787
Pothuaud L, Barthe N, Krieg MA, Mehsen N, Carceller P, Hans D (2009) Evaluation of the potential use of trabecular bone score to complement bone mineral density in the diagnosis of osteoporosis: a preliminary spine BMD-matched, case-control study. J Clin Densitom 12(2):170–176
Silva BC, Leslie WD (2017) Trabecular bone score: anew DXA-derived measurement for fracture risk assessment. Endocrinol Metab Clin N Am 46(1):153–180
Silva BC, Broy SB, Boutroy S, Schousboe JT, Shepherd JA, Leslie WD (2015) Fracture risk prediction by non-BMD DXA measures: the 2015 ISCD official positions part 2: trabecular bone score. J Clin Densitom 18(3):309–330
Donaldson AA, Feldman HA, O'Donnell JM, Gopalakrishnan G, Gordon CM (2015) Spinal bone texture assessed by trabecular bone score in adolescent girls with anorexia nervosa. J Clin Endocrinol Metab 100(9):3436–3442
Heinio L, Nikander R, Sievanen H (2015) Association between long-term exercise loading and lumbar spine trabecular bone score (TBS) in different exercise loading groups. J Musculoskelet Neuronal Interact 15(3):279–285
Del Rio LM, Winzenrieth R, Cormier C, DiGregorio S (2013) Bone mass, bone microarchitecture and anthropometric measurements during childhood growth in Spanish girls. Bone Abstracts 2:186
Winzenrieth R et al (2013) Influence of age and gender on spine bone density and TBS microarchitectural texture parameters in infants, in ICCBH: Rotterdam, The Netherlands
Libber J et al (2015) TBS increases over time in pre-teen girls, in ICCBH: Salzburg, Austria
Del Rio Barquero LM, Winzenrieth R, and DiGregorio S (2015) Bone quality and quantity in Duchenne muscular dystrophy patients, in ICCBH: Salzburg, Austria
Shawwa K et al (2015) Predictors of trabecular bone score in school children. Osteoporos Int
Del Rio Barquero LM, DiGregorio S, and Winzenrieth R (2014) Bone microarchitecture (TBS) and bone mass development during childhood and adolescence in a Spanish population group., in WCO-ESCEO-IOF: Sevilla, Spain
Greulich WW, Pyle SI (eds) (1959) Radiographic atlas of skeletal development of the hand and wrist, 2nd edn. Stanford University Press, Stanford
Tanner JM, Whitehouse RH, Marubini E, Resele LF (1976) The adolescent growth spurt of boys and girls of the Harpenden growth study. Ann Hum Biol 3(2):109–126
Kroger H et al (1992) Dual-energy X-ray absorptiometry in normal women: a cross-sectional study of 717 Finnish volunteers. Osteoporos Int 2(3):135–140
Hoyer-Kuhn H, Knoop K, Semler O, Kuhr K, Hellmich M, Schoenau E, Koerber F (2016) Comparison of DXA scans and conventional X-rays for spine morphometry and bone age determination in children. J Clin Densitom 19(2):208–215
Cole TJ, Green PJ (1992) Smoothing reference centile curves: the LMS method and penalized likelihood. Stat Med 11(10):1305–1319
Lazar L, Phillip M (2012) Pubertal disorders and bone maturation. Endocrinol Metab Clin N Am 41(4):805–825
Carrascosa A, Fernández JM, Fernández C, Ferrández A, López-Siguero JP, Sánchez E, Sobradillo B, Yeste D (2008) Spanish growth studies 2008. New anthropometric standards. Endocrinol Nutr 55(10):484–506
Tanner JM, Whitehouse RH, Marshall WA, Carter BS (1975) Prediction of adult height from height, bone age, and occurrence of menarche, at ages 4 to 16 with allowance for midparent height. Arch Dis Child 50(1):14–26
Martin DD, Wit JM, Hochberg Z’, Sävendahl L, van Rijn RR, Fricke O, Cameron N, Caliebe J, Hertel T, Kiepe D, Albertsson-Wikland K, Thodberg HH, Binder G, Ranke MB (2011) The use of bone age in clinical practice - part 1. Horm Res Paediatr 76(1):1–9
Martin DD, Wit JM, Hochberg Z’, van Rijn RR, Fricke O, Werther G, Cameron N, Hertel T, Wudy SA, Butler G, Thodberg HH, Binder G, Ranke MB (2011) The use of bone age in clinical practice - part 2. Horm Res Paediatr 76(1):10–16
Bailey DA, Martin AD, McKay HA, Whiting S, Mirwald R (2000) Calcium accretion in girls and boys during puberty: a longitudinal analysis. J Bone Miner Res 15(11):2245–2250
McKay HA, Bailey DA, Mirwald RL, Davison KS, Faulkner RA (1998) Peak bone mineral accrual and age at menarche in adolescent girls: a 6-year longitudinal study. J Pediatr 133(5):682–687
Simonelli C, Leib E, Mossman N, Winzenrieth R, Hans D, McClung M (2014) Creation of an age-adjusted, dual-energy x-ray absorptiometry-derived trabecular bone score curve for the lumbar spine in non-Hispanic US White women. J Clin Densitom 17(2):314–319
Cheng P, Qi HM, di WJ, Liu J, Yu J, Lv S, Shen YL, Zha JM, Cai JM, Lai B, Ding GX (2016) Establishment of TBS reference plots and correlation between TBS and BMD in healthy mainland Chinese women. Arch Osteoporos 11:5
Looker AC, Sarafrazi Isfahani N, Fan B, Shepherd JA (2016) Trabecular bone scores and lumbar spine bone mineral density of US adults: comparison of relationships with demographic and body size variables. Osteoporos Int 27:2467–2475
Dowthwaite JN, Winzenrieth R, Binkley N, Krueger D, Scerpella TA (2017) A focused evaluation of lumbar spine trabecular bone score in the first year post-menarche. Arch Osteoporos 12(1):90
Thodberg HH, Kreiborg S, Juul A, Pedersen KD (2009) The BoneXpert method for automated determination of skeletal maturity. IEEE Trans Med Imaging 28(1):52–66
Thodberg HH, van Rijn RR, Tanaka T, Martin DD, Kreiborg S (2010) A paediatric bone index derived by automated radiogrammetry. Osteoporos Int 21(8):1391–1400
Acknowledgements
We thank MSc. Regina Ambrosi for her work in the acquisition of DXA scans.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics committee
The bioethics, biosafety, and scientific committees from Hospital Infantil Federico Gómez approved the protocol of this study.
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Guagnelli, M.A., Winzenrieth, R., Lopez-Gonzalez, D. et al. Bone age as a correction factor for the analysis of trabecular bone score (TBS) in children. Arch Osteoporos 14, 26 (2019). https://doi.org/10.1007/s11657-019-0573-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-019-0573-6