Abstract
Summary
The Ecuadorian hospital discharge system examined trends in hip fracture hospitalization rates among older adults. A significant upward trend in hip fracture rates occurred in both genders over the study period.
Introduction
Previous research has reported increasing hip fracture rates in Ecuador. Thus, this study aimed to extend previous findings by examining the nationwide incidence of hip fractures among adults aged 65 years and older between 1999 and 2016. A secondary objective was to compare hip fracture trends among older Ecuadorians with their counterparts in the United States (U.S.).
Methods
The National Hospital Discharge System and the Healthcare Cost and Utilization Project net were assessed to identify older adults hospitalized with a principal diagnosis of hip fractures in Ecuador and the U.S., respectively. The Joinpoint regression analysis software was used to examine the average annual percent change in hip fracture rates.
Results
A total of 20,091 adults with a mean age of 82.3 (SD 8.1) years were hospitalized with a principal diagnosis of hip fractures during the study period. After an adjustment for age, hip fracture rates increased annually on average by 4.6% (95% CI 3.8%, 5.4%) from 96.4/100,000 in 1999 to 173.1/100,000 persons in 2016. Between 1999 and 2014, hip fracture age-adjusted rates decreased on average by − 2.5% (95% CI − 2.7%, − 2.3%) among older adults in the U.S. while hip fracture rates steadily increased by 4.6% (95% CI, 3.6%, 5.7%) per year in their Ecuadorian counterparts.
Conclusions
Hip fracture rates markedly increased among older adults in Ecuador. The present findings should alert public health authorities to implement policies of osteoporosis awareness and prevention in Ecuador.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip fracture in older adults represents a major public health burden associated with considerable morbidity, healthcare costs, and increased mortality [1,2,3]. Although the incidence of hip fracture in Ecuador was reported as one of the lowest worldwide, hip fracture rates nationwide significantly increased by 4.2 and 3.4% per year among women and men aged 50 years and older between 1999 and 2008, respectively. Notably, the increased hip fracture incidence during the study period was attributed to upward trends in hip fracture rates, particularly among those aged 80 years and older. Moreover, it was projected that the number of hip fractures will increase among older Ecuadorians over the next decades [4,5,6].
Previous population-based studies in North America have reported that age-standardized hip fracture rates steadily declined in Canada and among Medicare beneficiaries in the United States (U.S.) between 1996 and 2005 [7, 8]. While there is scarce data about the incidence of hip fractures in Central and South America, increasing hip fracture rates were documented in Mexico and Barranquilla, Colombia [9,10,11]. In Ecuador, life expectancy has gradually increased over the past decades. For instance, Ecuadorians were expected to live 64.6 years in 1980–1985 and 75.6 years in 2010–2015. Moreover, it is estimated that life expectancy will increase to 82.1 years by 2050–2055 [12]. These demographic changes along with a higher prevalence of falls and vitamin D deficiency recently reported among older adults in the country may increase the number of individuals at risk of hip fracture [13, 14]. The present study aimed to extend previous research findings by examining hip fracture rate samong adults aged 65 years and older in Ecuador between 1999 and 2016. Moreover, temporal trends hip fracture incidence rates in South America have not been previously reported except for Ecuador [9]. Therefore, a secondary objective was to compare recent national hip fracture rates with their counterparts in the U.S.
Methods
The National Hospital Discharge Surveillance System (Anuario de Egresos Hospitalarios) is conducted annually by the National Institute of Statistics and Census (INEC). It covers discharges from private and public hospitals in Ecuador. Data abstracted from hospital records contain items relating to demographic, administrative information, length of stay, discharge status, and a principal discharge diagnosis [15]. The discharge diagnoses have been coded according to the International Classification of Diseases, tenth revision, Clinical Modification (ICD-10-CM) since 1999 [16]. The data selected for this study comprised subjects aged 65 years and older hospitalized with a principal diagnosis ICD-10 code of femoral neck (S72.0) or pertrochanteric (S72.1) hip fracture. Estimates of the Ecuadorian population aged 65 years and older and projections of the population by provinces of the country were obtained from the Latin American and Caribbean Demographic Center and National Information System, respectively [17, 18]. Age-specific (65–69, 70–74, 75–79, and 80 years and older) hip fracture rates by gender and regions of the country were calculated per 100,000 population. Subsequently, fracture rates were age adjusted using the 2010 Ecuadorian Census as the standard population.
The Healthcare Cost and Utilization Project net (HCUPnet), online query system sponsored by the Agency for Healthcare Research and Quality (AHRQ), was assessed to generate hip fracture data from the Nationwide Inpatient Sample, which is representative of 20% of all U.S hospitals. The ICD-9-CM codes 820.00–820.9 were selected to identify individuals aged 65 years and older hospitalized with a principal diagnosis of hip fracture between 1999 and 2014 [19]. Age-specific (65–75 and ≥ 85 years) hip fracture rates per 100,000 persons were calculated using the U.S. population estimates [20]. Similarly, age-specific hip fracture rates were calculated among older Ecuadorians during the study period. Subsequently, to compare hip fracture rates between countries over time, hip fracture rates were directly standardized by the 2010 Ecuadorian population to account for demographic changes of the country’s population.
Statistical analysis
The Joinpoint regression program software, V.4.2.0.2 was used to identify points where a statistically significant change occurred in the linear slope of rates. The joinpoint regression detects points at which significant changes in the direction and magnitude of trends occur over time, assuming constant variance and uncorrelated errors [21]. The results are presented as the average annual percent change (AAPC) with their corresponding 95% confidence interval (95% CI). The AAPC in rates is a summary measure of the trend over a prespecified fixed interval. This measure describes the average annual percent changes over a period of multiple years, which is valid even if the joinpoint model indicates that there were changes in trends during those years. The AAPC is computed as a weighted average of the annual percentage change in rates from the joinpoint model, with the weights equal to the length of the annual percent change interval [22]. The AAPC in age-specific and age-adjusted hip fracture rates by gender and regions of the country was examined during the study period. In the figures, the observed rates are represented by symbols and the predicted trends from the joinpoint regression model are represented by dashed lines.
Results
A total of 20,091 adults with a mean age of 82.3 (SD 8.1) years were hospitalized with a principal diagnosis of hip fractures between 1999 and 2016. Overall, women accounted for 69.8% of the cases. Notably, 13,739 (68.3%) hip fractures occurred among older adults residing in the provinces of Pichincha and Guayas, which are the most urbanized provinces of the country. By region of the country, 55.0% of the hip fractures were reported in the Andes Mountains, 42.9% on the coast, and only 2.0% in the Amazon. Overall, hip fracture in-hospital mortality was 4.9% in men and 3.7% in women during the study period. However, up to 6.2% of the men aged 80 years and older died during hospitalization after a hip fracture. Moreover, the mean length of stay after hip fracture hospitalization was 10.2 (SD 7.8) days.
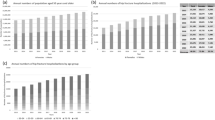
The total number of hip fractures increased from 575 in 1999 to 1950 in 2016. However, the estimated population of Ecuadorians aged 65 years and older also increased from 573,000 in 1999 to 1 million in 2016. After adjustment for age, hip fracture rates increased annually on average by 4.6% (95% CI 3.8%, 5.4%) from 96.4/100,000 in 1999 to 173.1/100,000 persons in 2016. As shown in Table 1, hip fracture rates increased exponentially with advancing age and were about twofold higher among women. In general, the highest AAPC in fracture rates was seen among subjects aged 80 years and older at 4.7% (95% CI, 3.8%, 5.6%) per year. Moreover, after age adjustment, hip fracture rates increased in men on average by 3.5% (95% CI 2.7%, 4.4%) per year while the AAPC increase in hip fracture rates was even higher in women at 4.7% (95% CI 3.8%, 5.6%) per year (Fig. 1).
As shown in Fig. 2, age-adjusted hip fracture rates increased in all regions of the country. However, hip fracture rates markedly increased in the coastal region of the country on average by 7.8% (95% CI, 6.0%, 9.6%) per year. In the Andes Mountains, the rates increased on average by 1.9% (95% CI, 0.5%, 3.3%) per year. However, a significant increase in hip fractures was seen since 2009 onward by 5.7% (95% CI, 2.8%, 8.8%) per year. As shown in Fig. 3, age-adjusted hip fracture rates decreased on average by − 2.5% (95% CI − 2.7%, − 2.3%) among older adults in the U.S. while the AAPC in hip fracture rates significantly increased by 4.6% (95% CI, 3.6%, 5.7%) among their Ecuadorian counterparts between 1999 and 2014.
Discussion
The present findings indicate that hip fracture rates increased among older adults in Ecuador between 1999 and 2016. Moreover, upward trends in hip fracture were predominantly attributed to a marked increase in fracture rates among men and women aged 80 years and older during the study period. Notably, after age adjustment, hip fracture rates gradually increased on average by 3.5 and 4.6% per year in men and women, respectively. These results extend and are consistent with those from a prior analysis describing an increase in hip fracture age-adjusted rates among Ecuadorian men and women aged 50 years and older by 3.4 and 4.2% per year between 1999 and 2008, respectively [6]. While there is scarce data on the epidemiology of hip fracture in South America, hip fracture age-adjusted rates among Mexican men and women aged 50 years and older beneficiaries of the Mexican Institute of Social Security increased by 1% per year during 2000–2006 [9, 10]. Similarly, previous studies have projected increasing hip fracture rates in Ecuador and Colombia over the next decades [6, 11]. Of interest, Ballane et al. in a study conducted to examine the annual percentage change in age-adjusted hip fracture rates worldwide demonstrated downward trends in hip fracture rates in most Western countries and Oceania since the mid-1990s. However, the same study reported geographic differences in hip fracture trends in South East Asia. For instance, increasing hip fracture rates occurred in Japan, China, and South Korea, except in urbanized areas such as Hong Kong and Taiwan, which are in agreement with the present study results [9].
Notably, marked opposing hip fracture trends were seen among older adults in Ecuador and the U.S. between 1999 and 2014. While the precise reasons for these findings are unknown, there are possible explanations for the present results. The increased hip fracture rates in Ecuador may reflect improved medical care resulting in longer survival of frail elders at higher risk of hip fracture [23]. Moreover, the use of specific osteoporosis therapy has also been postulated as a contributor to the decreasing fracture rates in many countries [9]. For instance, a significant downward trend in hip fracture age-adjusted rates occurred after 1995 in Canada and among Medicare beneficiaries the U.S., which coincided with increasing use of bisphosphonates [7, 8]. Of interest, a recent study among Medicare beneficiaries suggested that the decline in hip fracture rates in the U.S. over the past 15 years may be ending. In that particular study, hip fracture rates in 2013 and 2014 were greater that the predicted trends. Similarly, we found that hip fracture rates among older Americans leveled off during the last 2 years of the study. As the investigators concluded, possible explanations for this finding may be related to fewer dual-energy X-ray absorptiometry (DXA) scan performed since 2009 and consequently fewer women diagnosed and treated for osteoporosis [24].
In Ecuador, a small cross-sectional study conducted among 53 women aged 60 years and older in Riobamba, Chimborazo, reported that the prevalence of osteoporosis and osteopenia was 13.2 and 50.9%, respectively [25]. Overall, about 50% of the participants used calcium supplements and were treated with bisphosphonates. Of note, osteoporosis prevalence rates among older women from this region of the country were comparable to those reported among U.S. women aged 60–69 years during 2005–2010 [26]. While it is unknown, the number of DXA machines or the access to bone mineral density (BMD) testing in Ecuador, the Latin American regional audit conducted in 2012 reported that the number DXA machines varies considerably in the region from 2 machines per million population in Bolivia and Guatemala to 10 per million in Chile and Brazil [27]. Despite these facts, a FRAX score calculator was developed to estimate the 10-year probability of hip or a major osteoporotic fracture in Ecuador. The FRAX calculation tool was designed to assist clinicians in predicting the 10-year probability of fracture with or without the addition of femoral neck BMD [28].
Of relevance, a recent study described that overall, 67.8 and 21.6% of the adults aged 60 years and older had evidence of vitamin D insufficiency and deficiency in Ecuador, respectively. In addition, even higher vitamin D deficiency prevalence rates were present among older women, indigenous, and those residing in the Andes Mountains region of the country. For instance, up to 40.5 and 34.8% of older indigenous and residents in the rural Andes Mountains had evidence of vitamin D deficiency, respectively. Since vitamin D deficiency is a well-known risk factor for secondary hyperparathyroidism, osteoporosis, and increased risk of fractures, the higher proportion of older Ecuadorians affected with this condition may partly explain the increased incidence of hip fracture seen in the present study [14]. Likewise, fall-related injuries represent an important public health problem affecting aging populations. For instance, about 1–14% of the falls in women result in hip fracture and over 90% of the hip fractures are the result of a fall [29]. Previous population-based studies indicate that 34.7 and 11.4% of the subjects aged 60 years sustained falls or fall-related injuries requiring medical attention in Ecuador, respectively. Of those who had fallen, up to 30.6% reported a fall-related injury[13, 30]. Moreover, subjects residing in the provinces of Guayas and Pichincha, the most urbanized provinces of the country, had significantly higher fall-related injuries as compared with other provinces of the country [30]. Similarly, two thirds of hospitalizations for hip fracture occurred in these provinces of the country. Moreover, hip fracture age-adjusted rates differed by region of the country with the highest rates found among residents in the Andes Mountains. However, a marked annual increase in hip fracture rates was seen predominantly among residents in the coastal region exceeding those rates in the Andes Mountains in 2016. Although we could postulate that hip fractures occurred predominantly in urbanized areas of the country, further studies are needed to examine urban vs. rural differences in hip fracture rates in Ecuador. Consistent with our results, previous studies have described that changes in lifestyle with urbanization as a possible explanation of increasing hip fractures rates, particularly in Asia [9, 23].
The present study has several limitations. First, the diagnosis of hip fracture was not radiographically confirmed and misclassification of fractures may have occurred. In addition, no previous study has validated the report of ICD-10 hip fracture codes in Ecuador. Second, because the mechanism of injury resulting in hip fractures is not reported by the National Hospital Discharge Surveillance System, high-impact injuries such as those related to motor vehicle accidents may have overestimated the number of hip fractures. Third, comorbidities, medications, or lifestyle behaviors, which may increase the risk of hip fracture, are not documented in this hospitalization discharge survey. Fourth, the present findings may be generalized only to populations with similar racial and geographic characteristics in Latin America.
In conclusion, hip fracture rates markedly increased among older adults in Ecuador. The present findings should alert public health authorities to implement policies of osteoporosis awareness and prevention in Ecuador.
References
Cummings SR, Melton LJ (2002) Epidemiology and outcomes of osteoporotic fractures. Lancet 359(9319):1761–1767. https://doi.org/10.1016/S0140-6736(02)08657-9
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res 22(3):465–475. https://doi.org/10.1359/jbmr.061113
Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR (2009) Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA 301(5):513–521. https://doi.org/10.1001/jama.2009.50
Kanis JA, Odén A, McCloskey EV, Johansson H, Wahl DA, Cooper C (2012) IOF Working Group on Epidemiology and Quality of Life. A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 9:2239–2256
Orces CH (2009) Epidemiology of hip fractures in Ecuador. Rev Panam Salud Publica 25(5):438–442
Orces CH (2011) Trends in hip fracture rates in Ecuador and projections for the future. Rev Panam Salud Publica 29(1):27–31
Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB (2009) Incidence and mortality of hip fractures in the United States. JAMA 302(14):1573–1579. https://doi.org/10.1001/jama.2009.1462
Leslie WD, O'Donnell S, Jean S, Lagacé C, Walsh P, Bancej C, Morin S, Hanley DA, Papaioannou A, Osteoporosis Surveillance Expert Working Group (2009) Trends in hip fracture rates in Canada. JAMA 302(8):883–889. https://doi.org/10.1001/jama.2009.1231
Ballane G, Cauley JA, Luckey MM, Fuleihan G-H (2014) Secular trends in hip fractures worldwide: opposing trends East versus West. J Bone Miner Res 29(8):1745–1755. https://doi.org/10.1002/jbmr.2218
Johansson H, Clark P, Carlos F, Oden A, McCloskey EV, Kanis JA (2011) Increasing age- and sex-specific rates of hip fracture in Mexico: a survey of the Mexican Institute of Social Security. Osteoporos Int 22(8):2359–2364. https://doi.org/10.1007/s00198-010-1475-z
Jaller-Raad JJ, Jaller-Char JJ, Lechuga-Ortiz JA, Navarro-Lechuga E, Johansson H, Kanis JA (2013) Incidence of hip fracture in Barranquilla, Colombia, and the development of a Colombian FRAX model. Calcif Tissue Int 93(1):15–22. https://doi.org/10.1007/s00223-013-9717-7
http://www.eclac.cl/celade/proyecciones/basedatos_BD.htm.Accessed 1 June2017
Orces CH (2013) Prevalence and determinants of falls among older adults in Ecuador: an analysis of the SABE I survey. Curr Gerontol Geriatr Res 2013:1–7. https://doi.org/10.1155/2013/495468
Orces CH (2015) Vitamin D status among older adults residing in the littoral and Andes Mountains in Ecuador. ScientificWorldJournal 2015:1–8. https://doi.org/10.1155/2015/545297
http://www.ecuadorencifras.gob.ec/camas-y-egresos-hospitalarios/. Accessed 2 May 2017
http://apps.who.int/classifications/icd10/browse/2015/en.Accessed June 1, May 2017
http://www.cepal.org/celade/publica/bol66/BD66.html.Accessed 1 June2017
http://sni.gob.ec/proyecciones-y-estudios-demograficos Accessed 27 Oct 2017
https://hcupnet.ahrq.gov/#setup Accessed 1 June2017
https://wonder.cdc.gov/bridged-race-population.html. Accessed 1 June2017
http://surveillance.cancer.gov/joinpoint/.Accessed 1 June2017
Clegg LX, Hankey BF, Tiwari R, Feuer EJ, Edwards BK (2009) Estimating average annual per cent change in trend analysis. Stat Med 28(29):3670–3682. https://doi.org/10.1002/sim.3733
Xia WB, He SL, Xu L, Liu AM, Jiang Y, Li M, Wang O, Xing XP, Sun Y, Cummings SR (2012) Rapidly increasing rates of hip fracture in Beijing, China. J Bone Miner Res 27(1):125–129. https://doi.org/10.1002/jbmr.519
LewieckiEM, CurtisJ, GagelR, SirisE, WrightNC, YunH (2016). Hip fracture and declining DXA testing: at a breaking point. J Bone Miner Res 31 (Suppl 1) Available at http://www.asbmr.org/education/2016-abstracts. Accessed 22 Oct 2017
Betancourt Ortiz SL (2014) Bone mineral density, dietary calcium and risk factor for presumptive osteoporosis in Ecuadorian aged women. Nutr Hosp 30(2):372–384. https://doi.org/10.3305/nh.2014.30.2.7563
Wright NC, Looker AC, Saag KG, Curtis JR, Delzell ES, Randall S, Dawson-Hughes B (2014) The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res 29(11):2520–2526. https://doi.org/10.1002/jbmr.2269
https://www.iofbonehealth.org/sites/default/files/media/PDFs/Regional%20Audits/2012-Latin_America_Audit_0_0.pdf. 1 Accessed June 2017
https://www.sheffield.ac.uk/FRAX/tool.aspx?country=43. Accessed 1 June 2017
Orces CH (2013) Emergency department visits for fall-related fractures among older adults in the USA: a retrospective cross-sectional analysis of the National Electronic Injury Surveillance System All Injury Program, 2001–2008. BMJ Open 3(1):e001722. https://doi.org/10.1136/bmjopen-2012-001722
Orces CH (2014) Prevalence and determinants of fall-related injuries among older adults in Ecuador. Curr Gerontol Geriatr Res 2014:1–7. https://doi.org/10.1155/2014/863473
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Orces, C.H., Gavilanez, E.L. Increasing hip fracture rates among older adults in Ecuador: analysis of the National Hospital Discharge System, 1999–2016. Arch Osteoporos 12, 109 (2017). https://doi.org/10.1007/s11657-017-0410-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-017-0410-8