Abstract
Summary
A randomised controlled trial of vertebroplasty (VP) versus placebo assessed the effect of VP on the risk of further vertebral fractures. While no statistically significant between-group differences for new or progressed fracture risk at 12 and 24 months were observed, we observed a consistent trend towards higher risk of any type of fracture in the group undergoing VP. Our analysis was underpowered, and further adequately powered studies are needed to be able to draw firm conclusions about further vertebral risk with vertebroplasty.
Purpose
This study seeks to assess the effect of VP on the risk of further radiologically apparent vertebral fracture within two years of the procedure.
Methods
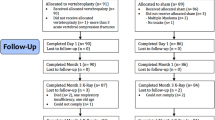
We conducted a randomised placebo-controlled trial of VP in people with acute osteoporotic vertebral fracture. Eligible participants were randomly assigned to VP (n = 38) or placebo (n = 40). Cement volume and leakage were recorded for the VP group. Plain thoracolumbar radiographs were taken at baseline, 12 and 24 months. Two independent radiologists assessed these for new and progressed fractures at the same, adjacent and non-adjacent levels.
Results
At 12 and 24 months, radiographs were available for 45 (58 %) and 47 (60 %) participants, respectively. There were no between-group differences for new or progressed fractures: 32 and 40 in the VP group after 12 and 24 months compared with 21 and 33 in the placebo group (hazard ratio (HR) 1.80, 95 % confidence interval (CI) 0.82 to 3.94). Similar results were seen when considering only adjacent (HR (95 % CI) 2.30 (0.57 to 9.29)) and non-adjacent (HR (95 % CI) 1.45 (0.55 to 3.81) levels. In all comparisons, there was a consistent trend towards higher risk of any type of fracture in the group undergoing VP. Within the VP group, fracture risk was unrelated to total (HR (95 % CI) 0.91 (0.71 to 1.17)) or relative (HR (95 % CI) 1.31 (0.15 to 11.48)) cement volume or cement leakage (HR (95 % CI) 1.20 (0.63 to 2.31)).
Conclusion
For patients undergoing VP, our study did not demonstrate significant increases in subsequent fracture risk beyond that experienced by those with vertebral fractures who did not undergo the procedure. However, because of the non-significant numerical increases observed, studies with adequate power are needed to draw definite conclusions about fracture risk.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Vertebroplasty (VP) is a minimally invasive procedure used to palliate pain from painful osteoporotic vertebral compression fractures. It was first introduced in the late 1980s, but recent evidence has questioned its efficacy [1, 2], while data regarding its long-term safety is limited and inconclusive. Serious complications, including subsequent vertebral fractures, pulmonary and cerebral embolism, infection, cardiac perforation and cement leakage resulting in neurological deficit, have been reported [3–5].
Retrospective reviews of patients undergoing VP for osteoporotic compression fractures have reported that between 6 and 34 % had new vertebral fractures following the procedure [6, 7], but without the fracture risk for an appropriate comparison group, this information has limited value. Those with a prevalent fracture are at higher risk of a new vertebral fracture, therefore it is important to determine whether VP increases the fracture risk beyond that expected for patients not having VP.
Treated vertebral fractures can undergo height loss and persistent oedema [8], while vertebrae adjacent to the treated level appear to be more susceptible to incident fracture following VP [7, 9–12], particularly in the short term, but the time frame for the occurrence of these subsequent fractures is unclear. A prevalent osteoporotic vertebral fracture also increases the risk of adjacent fractures [13] as there are spinal zones where risk is considered to be increased across several levels simultaneously [14].
A higher fracture risk for patients having VP compared with patients choosing alternative management has been reported by some [15, 16], but not all studies [10, 17, 18]. Fracture risk may also be related to the volume of cement injected, cement leakage or patient characteristics such as age or bone mineral density (BMD). A meta-analysis of 16 case–control studies found that the risk of new vertebral fractures was higher for patients with low BMD, low body mass index and cement leakage, but was not associated with age or cement volume [3].
Two recent blinded, randomised controlled trials (RCTs) showed no benefit of VP compared with a placebo procedure for improving pain or function in the short term [1, 2]. Adequately powered sub-group analyses based on these two RCTs also showed no differences in pain improvement between the groups up to 1 month following the trial procedure for patients with acute pain (less than 6 weeks) or severe pain (>8 on a 0 to10 VAS pain scale) [19]. The US-based trial allowed cross-over after 1 month complicating the assessment of the risk of subsequent vertebral fracture [2]. In the Australian-based trial, there was no difference between the groups in new clinical vertebral fractures reported to 6 months [1]. Two-year follow-up also demonstrated no pain or function benefit of VP over the placebo procedure [20].
We report here the 24-month independent radiology review of outcomes. The incidence of radiologically evident new and progressed vertebral fractures at the procedure level and adjacent and non-adjacent vertebrae is compared for the two groups. We also investigate the risk of new or progressed incident fractures in relation to cement volume, cement leakage and certain baseline patient clinical characteristics.
Methods
Between April 2004 and October 2010, we conducted a participant and outcome assessor-blinded placebo-controlled trial of VP. Full protocol details [21] and efficacy and safety results have been reported elsewhere [1, 19]. Briefly, eligible participants had one or two acute osteoporotic vertebral compression fractures (OVCFs) of at least grade 1 [22] confirmed by history, radiograph and the presence of bone oedema on magnetic resonance imaging (MRI). If MRI was contraindicated or could not be performed, a bone scan was required to determine the presence of increased uptake compatible with recent fracture. This applied to 12 (15 %) of the 78 participants. Eligible participants were randomised to VP or a placebo procedure stratified by study centre, sex and duration of symptoms (<6 weeks or ≥6 weeks). Participants and all study personnel other than the treating radiologist were blinded to treatment allocation. The human research ethics committees at each participating centre approved the study, and all participants provided written informed consent. The trial was registered with the Australian New Zealand Clinical Trials Registry (ACTRN012605000079640).
For the VP intervention, the participant was sedated with midazolam and fentanyl and local anaesthetic infiltrated into the skin overlying the target pedicle and the periosteum of the posterior lamina prior to making a small incision in the skin. Under image guidance, prepared polymethylmethacrylate (PMMA) cement was slowly injected into the vertebral body via the pedicle(s), using a 13-gauge needle, until substantial resistance was met or the cement reached the posterior quarter of the vertebral body. Fourteen (31 %) of the 45 treated levels used a bipedicular approach. The total volume of cement injected and any cement leakage was determined during cement injection and assessed on final AP and lateral images post procedure.
The placebo procedure was identical up to the skin incision. A 13-gauge needle was introduced through the excision to rest on the lamina. The lamina was gently tapped with a blunt stylet, but not penetrated, to mimic the VP procedure and a small quantity of PMMA was prepared so that its smell permeated the room.
Baseline data collected included lumbar and femoral neck bone mineral density (current or in the past year) and use of bisphosphonates and oral glucocorticoids. Plain radiograph and either MRI or bone scintigraphy and computerised tomography (CT) scans were performed at baseline to assess eligibility for the trial. Antero-posterior and lateral images were taken after the injection of cement in the active treatment group, and all participants had plain radiographs taken at 12 and 24 months post-procedure. At the end of the study, the baseline plain radiographs and MRI or bone and CT scans, and the follow-up radiographs were digitised. CDs containing the digitised images were couriered by registered mail to two independent radiologists (BMH and MDR) at the Mayo Clinic for review. Any plain radiographs taken to confirm symptomatic fractures occurring during the follow-up period were also digitised and sent for review. Any confirmed fractures were included in the analysis with the confirmed fracture date.
The radiologists reviewed all available imaging and recorded vertebral body compression fractures of the visualized spine. CT, MRI, bone scan and radiographs were reviewed together to identify the fractures. The fractures were categorized as mild, moderate and severe with morphology of wedge, biconcave or crush according to Genant’s semi-quantitative technique [22]. The 12- and 24-month radiographs were assessed for new vertebral fractures and any progression of pre-existing vertebral fractures. New fractures were defined as development of abnormal vertebral body morphology with loss of normal height. Progression of pre-existing fractures was defined as increased loss of vertebral body height or change in fracture morphology according to this semi-quantitative technique. For participants who had undergone VP, the amount of cement injected was assessed from the radiograph at the time of the procedure as the ratio of the length of cement to the total length of the vertebra in each of the craniocaudal, anterior-posterior and medial-lateral directions. The relative volume of cement injected was then calculated as the product of the three ratios. The values used in the analyses were the mean scores for the two radiologists.
Because of the radio-opacity of PMMA, it was not possible to blind the radiologists reviewing the follow-up films. The radiologists reviewed the films independently and discrepancies were resolved by consensus at the completion of the review process.
The risk of new and progressed fractures at the treated, adjacent and non-adjacent vertebral levels was compared for both treatment groups using Kaplan–Meier survival analysis. The event date was taken as the date of the X-ray and the censor date was the date of the 24-month X-ray or the date of the final questionnaire completed if no X-ray was available. Because an individual could experience multiple fracture events, participants remained in the risk set if a fracture event occurred. If a new fracture was assessed as progressed at one time point, it was not included again at the later time.
Possible predictors of overall fracture risk were assessed using Cox proportional hazards models including sex, site of treated level (thoracic or lumbar) and baseline values of age, lumbar and femoral neck T score ≤−2.5 or >2.5, previous spinal fracture, glucocorticoid use and duration, use of osteoporosis medication at baseline and current use collected at 1 and 2 years.
The influence of total cement volume, relative cement volume and cement leakage on the risk of fracture was also investigated for the VP group using Cox modelling.
We calculated that a total sample of 164 participants (82/group) would be needed to show a threefold increase in the risk of further vertebral fractures at 24 months assuming a 10 % event rate in the placebo group [21]. However, trial enrolment was terminated prior to reaching the planned sample size for long-term outcomes due to recruitment difficulties. The decision was made with the knowledge that the study’s power was sufficient to address the primary outcome. The decision to curtail recruitment was made without knowledge of any outcome results.
Results
A total of 92 vertebral levels were treated in the trial; 45 levels for the 38 participants having the VP procedure and 47 levels for the 40 participants undergoing placebo treatment. Treated levels were 15 thoracic (T6–T8, 6 placebo; 9 VP), 60 thoracolumbar (T7–L2, 29 placebo; 31 VP) and 17 lumbar (L3–L4, 12 placebo; 5 VP). Not all pre-treatment MRI and/or bone scans were available for review. Some participants did not attend for follow-up radiographs or did not return their films and copies were not available from the imaging facility. Table 1 shows the availability of films sent for independent radiological review at baseline and each follow-up time point.
Of the 68 (74 %) pre-treatment levels reviewed (29 (64 %) VP and 39 (83 %) placebo), bone marrow oedema and/or increased uptake on bone scintigraphy was detected in 61 (90 %) levels (27 (90 %) were in the VP levels and 34 (87 %) were in the placebo procedure levels). The mean (SD) cement volume per level for the treated group was 2.8 (1.2) ml and cement leakage occurred at 18 (40 %) treated levels. The mean (SD) relative cement volume was 34 % (16 %) for the 36 levels assessed at the radiology review. At 1 year, 60.6 % of the VP group and 70.6 % of the placebo group (65.7 % overall; p = 0.34) reported taking treatment for osteoporosis that included bisphosphonates (93 %) and raloxifene (7 %); at 2 years, this had changed to 65.5 % for the VP group and 67.9 % for the placebo group (66.7 % overall, 87 % bisphosphonates, 11 % raloxifene and 2 % strontium ranelate; p = 0.85).
Subsequent fractures for each group are shown in Table 2 by position, type and time after the procedure. Within the 2-year follow-up period, there were 17 new fractures and 23 progressed fractures in the VP group and 10 new and 23 progressed fractures in the placebo group. There were no significant differences between the groups for the risk of new or new and progressed fractures combined at any level, adjacent or non-adjacent (Table 3). Similarly, there were no significant differences between the groups for new or new and progressed fractures combined at the procedure level. In all comparisons, however, there was a consistent trend towards higher risk of any type of fracture in the group undergoing VP. Kaplan–Meier curves for new (Fig. 1a) and progressed fractures (Fig. 1b) at any level by treatment group are shown in Fig. 1. Figure 2 shows Kaplan–Meier curves for new (2A) and new and progressed (2B) adjacent level fractures by group.
Cox regression also indicated no association between the risk of new or progressed fractures at adjacent, non-adjacent or procedure level and age, sex, site of treated level, use of bisphosphonates at baseline or current bisphosphonate use, glucocorticoid use or duration of use, previous vertebral fracture, BMD, total or relative cement volume or cement leakage (Table 4).
Discussion
In this randomised controlled trial with 24-month follow-up, there were no statistically significant differences in the risk of new or progressed radiographically apparent fractures in participants who received VP compared with those who received a placebo procedure. However, in all comparisons, there was a consistent trend towards higher risk of any type of fracture in the group undergoing VP. Neither the volume of cement injected, cement leakage or VP level was associated with the risk of subsequent fractures. In addition, none of the patient characteristics we examined were linked with subsequent fracture risk.
Results from randomised controlled trials that have compared risk of subsequent vertebral fracture in participants receiving VP compared with those receiving conservative treatment have been inconsistent. One trial reported a significantly increased risk of radiologically apparent vertebral fractures associated with VP in comparison to usual care over 12 months follow-up (29 new radiologic vertebral fractures observed in 17 of 64 patients treated with VP compared with 8 in 8 of 61 patients treated with usual care; odds ratio (OR) 2.78 (95 % CI 1.02 to 7.62)) [9]. They also reported a significantly higher risk of symptomatic vertebral fractures (OR 25.67 (95 % CI 3.04 to 216.8)). Another trial reported a significantly lower risk of symptomatic vertebral fractures among patients receiving VP compared with usual care over 2 years of follow-up (2.2 % versus 13.3 %, p < 0.01), but did not report risk of radiologically apparent fractures [18]. Two trials did not observe an increased risk of radiologically apparent fractures with VP. Rousing et al. [23, 24] found no between-group difference in new radiologically apparent fractures at either 3 months (3 new fractures in the VP group versus 1 new fracture in the usual care group; relative risk (RR) 2.9 (95 % CI 0.3 to 25.7)) or 12 months (4 and 3 new fractures respectively; RR 1.3 (95 % CI not reported)). Klazen et al. [25] reported 18 new radiologically apparent fractures in 15 of 91 participants treated with VP compared with 30 new fractures in 21 of 85 participants treated conservatively (p = 0.44) after a mean of 11.4 months follow-up (median 12.0, range 1 to 24 months; 12 people refused radiographs during follow-up).
The main strength of our study is the randomised and blinded allocation of participants to treatment group. This minimises the selection bias associated with participant or clinician choice of the procedure and gives a more appropriate assessment of the true effect of VP. Although the presence of bone marrow oedema was an eligibility criterion for inclusion in the study, independent radiology review confirmed the presence of oedema in only 90 %. Given that bone marrow oedema can be quite subtle and is subject to false positive diagnosis, there will be unavoidable inter-observer variability. Wang et al. [26] reported a kappa statistic for inter-rater reliability for Modic changes on vertebral MRIs of 0.79 and several studies have reported inter-rater agreement to be no higher than around 75 % [27, 28].
Our sample size to assess safety outcomes was limited due to the early termination of recruitment, and we had limited power to detect small to moderately increased risk of further vertebral fracture. With a total sample size of 78, we had only 50 % power to demonstrate the hypothesised threefold increase in fracture risk associated with VP. The hazard ratios seen in our study did not differ significantly from unity, ranging from 1.05 to 2.30 with wide 95 % confidence intervals. While all comparisons consistently indicated an increased risk, we have insufficient power to draw definite conclusions.
Another limitation is that we had standardised long-term radiological follow-up of only 60 % of all participants and 69 % of those still participating. We also included radiologically confirmed fractures identified at non-standard follow-up points for patients with back pain, but as we have no information from those without radiological follow-up, we have no way of determining whether follow-up was related to fracture outcomes.
We sought to determine whether VP increased the risk of any subsequent vertebral fracture. Our radiological review confirmed 73 new or progressed fractures but only around one third of these (n = 27) were clinically apparent [20]. Under diagnosis (false negative) rates of up to 46 % have been reported for radiologically confirmed vertebral fractures [29]. Delmas et al. also reported discrepancies between local and subsequent central radiology review indicating a 34 % false negative rate. Discrepancies between the two independent reviewers in our study were adjudicated to obtain consensus. Symptomatic, or clinically apparent, fractures are likely to cause the patient greater distress, but morbidity and mortality are increased following both symptomatic and asymptomatic fractures [30–32]. By either measure, there were no statistically significant differences between participants having the VP or the placebo procedure.
Objective outcomes such as radiologically confirmed fractures should be less prone to bias in outcome assessment but the radio-opacity of the cement makes blinded assessment impossible. Therefore, the two radiologists (BMH and MDR), who were not otherwise involved in the trial, would have been unblinded to the presence of cement in treated vertebrae in follow-up X-rays. If either radiologist had a pre-conceived belief, either positive or negative, about fracture risk following VP, this could have resulted in bias of either direction.
To conclusively establish whether or not there is an increased risk of further vertebral fracture associated with VP would require further randomised placebo-controlled trials. These studies would need to be large and have extended follow-up to demonstrate even a moderate risk increase. However, in the absence of proven benefits over placebo, it is questionable whether further placebo-controlled trials should be pursued. Meta-analyses of our study and other randomised placebo-controlled trials could also provide some insights.
Population-based studies may be an alternative option, but these need to be analysed carefully to account for differences in patient selection leading to biases in who gets treatment [33]. McCullough et al. examined a large database of US Medicare claims for patients with newly diagnosed vertebral fractures and illustrated how selection biases within claims data can alter results in this type of research; those undergoing VP differed from those not having vertebral augmentation. After adjusting for pre-treatment pain and function, age, comorbidities, socio-economic status and access to healthcare, factors that may influence patient or physician choice of treatment, they found increased healthcare utilisation in the augmented group, but no differences between the augmented and control groups in mortality or major medical complications at 1 year.
Conclusions
While VP in placebo-controlled studies has failed to provide superior pain relief or functional benefit compared with placebo, our study did not observe an increase in subsequent fracture risk beyond that experienced by those with vertebral fractures who do not undergo the procedure although lack of sufficient power precludes drawing definitive conclusions about fracture risk.
References
Buchbinder R et al (2009) A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med 361(6):557–568
Kallmes DF et al (2009) A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med 361(6):569–579
Zhang Z et al. (2012) Risk factors for new osteoporotic vertebral compression fractures after vertebroplasty: a systematic review and meta-analysis. J Spinal Disord Tech
Al-Nakshabandi NA (2011) Percutaneous vertebroplasty complications. Ann Saudi Med 31(3):294–297
Venmans A. et al. (2010) Percutaneous vertebroplasty and pulmonary cement embolism: results from VERTOS II. AJNR Am J Neuroradiol
McKiernan F, Faciszewski T, Jensen R (2006) Latent mobility of osteoporotic vertebral compression fractures. J Vasc Interv Radiol 17(9):1479–1487
Tanigawa N et al (2011) Percutaneous vertebroplasty for osteoporotic compression fractures: long-term evaluation of the technical and clinical outcomes. AJR Am J Roentgenol 196(6):1415–1418
Dansie DM et al (2005) MRI findings after successful vertebroplasty. AJNR Am J Neuroradiol 26(6):1595–1600
Blasco J et al (2012) Effect of vertebroplasty on pain relief, quality of life, and the incidence of new vertebral fractures: a 12-month randomized follow-up, controlled trial. J Bone Miner Res 27(5):1159–1166
Chosa K, Naito A, Awai K (2011) Newly developed compression fractures after percutaneous vertebroplasty: comparison with conservative treatment. Jpn J Radiol 29(5):335–341
Hulme PA et al (2006) Vertebroplasty and kyphoplasty: a systematic review of 69 clinical studies. Spine (Phila Pa 1976) 31(17):1983–2001
Uppin AA et al (2003) Occurrence of new vertebral body fracture after percutaneous vertebroplasty in patients with osteoporosis. Radiology 226(1):119–124
Trout AT, Kallmes DF, Kaufmann TJ (2006) New fractures after vertebroplasty: adjacent fractures occur significantly sooner. AJNR Am J Neuroradiol 27(1):217–223
Melton LJ 3rd, Kallmes DF (2006) Epidemiology of vertebral fractures: implications for vertebral augmentation. Acad Radiol 13(5):538–545
Álvarez L et al (2006) Percutaneous vertebroplasty: functional improvement in patients with osteoporotic compression fractures. Spine 31(10):1113–1118
Mudano AS et al (2009) Vertebroplasty and kyphoplasty are associated with an increased risk of secondary vertebral compression fractures: a population-based cohort study. Osteoporosis Int 20:819–826
Tang H, Zhao J, Hao C (2011) Osteoporotic vertebral compression fractures: surgery versus non-operative management. J Int Med Res 39:1438–1447
Farrokhi M, Alibai E, Maghami Z (2011) Randomized controlled trial of percutaneous vertebroplasty versus optimal medical management for the relief of pain and disability in acute osteoporotic vertebral compression fractures. J Neurosurg Spine 14(5):561–569
Staples MP et al (2011) Effectiveness of vertebroplasty using individual patient data from two randomised placebo controlled trials: meta-analysis. BMJ 343:d3952
Kroon F et al (2014) Two year results of a randomised placebo-controlled trial of vertebroplasty for acute osteoporotic vertebral fractures. J Bone Mineral Res 29(6):1346–1355
Buchbinder R et al (2008) Efficacy and safety of vertebroplasty for treatment of painful osteoporotic vertebral fractures: a randomised controlled trial [ACTRN012605000079640]. BMC Musculoskelet Disord 9:156
Genant HK et al (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Min Res 8(9):1137–1148
Rousing R et al (2009) Percutaneous vertebroplasty compared to conservative treatment in patients with painful acute or subacute osteoporotic vertebral fractures: three-months follow-up in a clinical randomized study. Spine (Phila Pa 1976) 34(13):1349–1354
Rousing R et al (2010) Twelve-months follow-up in forty-nine patients with acute/semiacute osteoporotic vertebral fractures treated conservatively or with percutaneous vertebroplasty: a clinical randomized study. Spine (Phila Pa 1976) 35(5):478–482
Klazen CA et al. (2010) Percutaneous vertebroplasty is not a risk factor for new osteoporotic compression fractures: results from VERTOS II. AJNR Am J Neuroradiol
Wang Y et al (2011) Quantitative measures of modic changes in lumbar spine magnetic resonance imaging: intra- and inter-rater reliability. Spine (Phila Pa 1976) 36(15):1236–1243
Hauptfleisch J et al (2013) Interobserver agreement of magnetic resonance imaging signs of osteomyelitis in pelvic pressure ulcers in patients with spinal cord injury. Arch Phys Med Rehabil 94(6):1107–1111
Madsen KB, Jurik AG (2010) MRI grading method for active and chronic spinal changes in spondyloarthritis. Clin Radiol 65(1):6–14
Delmas PD et al (2005) Underdiagnosis of vertebral fractures is a worldwide problem: the IMPACT study. J Bone Miner Res 20(4):557–563
Cauley JA et al (2000) Risk of mortality following clinical fractures. Osteoporos Int 11(7):556–561
Center JR et al (1999) Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet 353(9156):878–882
Kado DM et al (2000) Rate of bone loss is associated with mortality in older women: a prospective study. J Bone Min Res 15(10):1974–1980
McCullough BJ et al. (2013) Major medical outcomes with spinal augmentation vs conservative therapy. JAMA Intern Med
Acknowledgments
The authors would like to acknowledge the valuable contribution of Dr. Leigh Gray from the Department of Radiology, Mayo Clinic College of Medicine, Rochester, MN, USA. The trial was supported by grants from the Australian National Health and Medical Research Council (NHMRC) (284354), Arthritis Australia, Cabrini Institute, and Cook Australia. The Mayo Clinic received funding from NIH (R01 AR49373) for the work submitted and from Benvenue Medical, Inc. for an unrelated spine augmentation project. Rachelle Buchbinder is supported by an Australian NHMRC Senior Principal Research Fellowship.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Staples, M.P., Howe, B.M., Ringler, M.D. et al. New vertebral fractures after vertebroplasty: 2-year results from a randomised controlled trial. Arch Osteoporos 10, 26 (2015). https://doi.org/10.1007/s11657-015-0229-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-015-0229-0