Abstract
Background
In patients who experience frequent vaso-occlusive crises (VOC), opioid dependence may be due to a need for pain control as opposed to addiction; the implications of opioid use disorder (OUD) in this population are unclear.
Objective
To compare outcomes in hospitalizations for VOC in those with a history of OUD to those without a history of OUD.
Design
A retrospective assessment of hospitalizations for adults in the USA with a primary discharge diagnosis of VOC using the National Inpatient Sample database from 2016 to 2019. We also compared VOC hospitalizations to hospitalizations for all other reasons to assess differences in OUD-associated clinical factors.
Participants
In total, 273,460 hospitalizations for VOC; 23,120 (8.5%) of these hospital stays involved a secondary diagnosis of OUD.
Main Measures
Primary outcomes were length of hospital stay and cost. Mortality was a secondary outcome.
Key Results
Hospital length of stay was increased (mean 6.2 vs 4.9 days) in patients with OUD (adjusted rate ratio = 1.24, 95% CI 1.20–1.29, p < 0.001). Mean cost was also higher in those with OUD ($9076) than those without OUD ($8020, p < 0.001). Mortality was decreased in VOC hospitalizations in those with OUD, but the difference was not statistically significant (adjusted OR = 0.64, 95% CI 0.028–1.48, p = 0.30).
Conclusions
OUD is associated with increased length of stay and costs in patients with VOC. While there are many possible explanations, providers should consider undertreatment of pain due to addiction concerns as a potential factor; individualized pain plans to mitigate this challenge could be explored.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
Sickle cell disease (SCD) affects 100,000 patients within the United States (US) and there are over 200,000 annual admissions in the US for SCD-related complications.1,2 Vaso-occlusive crisis (VOC) is responsible for 95% of such admissions and 60% of patients with SCD will experience a VOC each year.1,2 VOCs are the result of sickled erythrocytes occluding microvasculature leading to severe pain.3,4,5,6,7 Heat, ice, topical medications, and non-steroidal anti-inflammatory drugs are all utilized for controlling pain in VOCs, but adequate analgesia typically requires opioids.3,8,9 However, concerns from healthcare providers over contributing to addiction development and accidental overdoses while under the provider’s care have long served as a barrier to treatment for patients with SCD who frequently report dissatisfaction with care and a perception of staff as unsympathetic, judgmental, and biased.4,10,11,12,13 Additionally, patients with SCD in the US are primarily Black (1:365 births) or Hispanic (1:16,300), populations which have historically reported that their pain goes unaddressed.14,15 Untreated pain results in not only physical distress but also economic strain for patients as individuals with untreated chronic pain are at risk for significant absenteeism, income loss, and healthcare costs.16
The absence of objective markers of pain in VOC contributes to provider uncertainty about how much opioid medication to provide, particularly given the current emphasis on opioid misuse and overuse.3,17 This uncertainly may allow for a variety of influences, such as provider bias, racial-ethnic disparities, and current opioid prescribing trends to impact a provider’s perception of pain in patients with VOC. Additionally, as highlighted in a recent review in JAMA,18 two in five (40%) patients with SCD may receive treatment for chronic SCD-related pain, with “nociceptive, neuropathic, and central components”; this chronic pain, accompanied at times by opioid use, can further increase provider concern for addiction as they fear giving more opioids, while having concerns about potential withdrawal if opioids were to be stopped.4,19 Indeed, rates of opioid addiction in patients with SCD are increased compared to the general population and have previously been estimated at 3–10%.20,21,22,23 One study found that by Diagnostic and Statistical Manual of Mental Disorders IV criteria, 31% of patients with SCD had substance dependence (a need for opioids to avoid withdrawal symptoms).24 However, only 2% of patients with SCD had substance dependence unrelated to pain; thus, what is perceived to be addiction to opioids may instead be reliance on them for adequate pain control.24
While prior studies have assessed how the route of administration and total amounts of opioids may impact VOC outcomes, the associations between OUD and outcomes such as length of stay (LOS), costs, or mortality have not been thoroughly explored in patients with VOC.25,26 It is not known if OUD is associated with an increase in LOS or increased cost in patients with VOC. Similarly, it is not known if OUD, which is associated with increased mortality in a variety of other inpatient conditions, increases mortality or other adverse outcomes in those with VOC.27,28,29 Additionally, there has been minimal study of clinical factors related to OUD in adult patients with VOC and how they may differ from OUD-associated factors in patients who do not have SCD. Wilson et al. found male sex and lower income, established associations with OUD in patients without SCD, to also be associated with OUD in patients with SCD.30,31,32 However, the study assessed patients in the outpatient setting and had a limited sample size that included pediatric cases.
To address these important gaps in knowledge, we performed a US nationwide retrospective study of hospitalizations for VOC to compare healthcare utilization and clinical outcomes in patients with SCD with and without a diagnosis of OUD. Furthermore, we compared VOC hospitalizations to hospitalizations for all other reasons to assess (1) differences in OUD-associated factors between the two populations and (2) differences in associations between presence of OUD and varied clinical outcomes. We hypothesized that a diagnosis of OUD would be associated with increased healthcare utilization (LOS and cost) and worse clinical outcomes (mortality) in patients with VOC and that OUD-associated factors would differ between hospitalizations for VOC and hospitalizations for other reasons.
METHODS
Study Design and Database Description
This is a retrospective cohort-comparison study. The National Inpatient Sample (NIS) was utilized to collect data on hospitalizations in the US from 2016 to 2019. The NIS was developed for the Healthcare Cost and Utilization Project (HCUP) which provides encounter-level data dating back to 1988 (https://hcup-us.ahrq.gov/overview.jsp). The NIS is an all-payer inpatient database that characterizes approximately 35 million annual US hospitalizations after weighting of its sample and includes data on inpatient utilization, cost, and outcomes. Prior to weighting, the NIS is composed of a 20% stratified sample of US hospital discharges, excluding rehabilitation and long-term acute care hospitals. A primary discharge diagnosis is provided by the NIS along with secondary diagnoses, basic demographic data, LOS, total hospital charges, and procedural data. The NIS is a publicly available, deidentified database and Institutional Review Board review and ethical approval were not required.
Study Samples and Variables
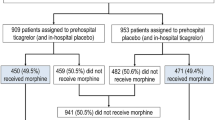
Cohort 1: Hospitalizations for patients 18 years of age or older with a primary discharge diagnosis of VOC in the years 2016–2019 were included in Cohort 1 (Fig. 1). For cases of hospitalizations with missing patient or outcome variables, the hospitalizations were included in the overall study sample but were excluded from assessments that involved the missing variables. The presence of a secondary diagnosis of OUD was evaluated in each hospitalization. ICD-10-CM codes were used to establish the diagnoses of VOC (D57.41, D57.419, D57.21, D57.219, D57.0, D57.00, D57.81, and D57.819) and OUD (F11.xxx) as previously described by Kang et al. and Donohue et al., respectively.1,33 Of note, the included ICD-10 codes for SCD included sickle-hemoglobin C disease and codes for unspecified sickle cell disorders. Baseline clinical data along with demographic and socioeconomic data were collected for each hospitalization with evaluated variables found in Table 1. The Deyo Modification of the Charlson Comorbidity Index was used. The Deyo Modification is a validated method of characterizing a patient’s risk of death based on their burden of comorbid illness.34,35 Income was determined by the median income within a patient’s ZIP code which is provided by the NIS.
Derivation of a study sample of hospitalizations with a primary diagnosis of vaso-occlusive crisis with and without a secondary diagnosis of opioid use disorder. The derivation of a second study sample consisting of hospitalizations for all reasons other than vaso-occlusive crisis is also presented and stratified by the presence of a secondary diagnosis of opioid use disorder.
Cohort 2: A second study sample was created that included all adult hospitalizations for reasons other than VOC during the same period (Fig. 1). Again, the presence of a secondary diagnosis of OUD was evaluated in the second study sample. The variables located in Table 1 were recorded for the non-VOC group.
Outcomes
In the comparison between VOC hospitalizations with and without a history of OUD, hospital LOS and cost were the primary outcomes and mortality was a secondary outcome. In the comparison of hospitalizations for VOC to non-VOC hospitalizations, a diagnosis of OUD itself was the assessed outcome and hospitalizations were assessed for OUD-associated factors including age, sex, race (white, Black, Hispanic, other), comorbid illness burden, hospital region (as defined in Table S1), income, primary payer, hospital teaching status, and hospital bed size.
Statistical Analysis
Standard procedures provided by HCUP were used to generate weighted results to estimate US nationwide results (https://hcup-us.ahrq.gov/tech_assist/tutorials.jsp) with clustering accounted for per HCUP guideline. The cost-to-charge ratios supplied by HCUP were used to generate cost estimates from total hospital charges (https://hcup-us.ahrq.gov/reports/methods/MS2021-05-CCR-Methodologies.pdf). Continuous variables were recorded as means with Student’s t-tests used for comparisons. Categorical variables were recorded as proportions with chi-square used for comparisons. Multilevel, univariable, and multivariable regressions were used to characterize associations with odds ratios and 95% confidence intervals and p-values reported for each outcome. Negative binominal regression analysis was used to evaluate for associations with LOS while a log-gamma model was used to evaluate for associations with cost with exponentiated coefficients presented as rate ratios for both outcomes. A p-value < 0.05 was considered statistically significant. Due to previous research demonstrating associations with SCD-related outcomes, we included, age, sex, race, income, primary payer, Charlson Comorbidity Index, hospital teaching status, and hospital bed size in each multivariable analysis.36,37,38 STATA, version 17.0 was used for all statistical computations.
RESULTS
Basic Characteristics
In total, there were 273,460 hospitalizations for VOC from 2016 to 2019 (Table 1), with OUD as a secondary diagnosis in 8.5% of those hospitalizations. The vast majority (> 90%) of patients were Black. Over 50% of hospitalizations occurred in the US South and the primary payer for most patients was either Medicare or Medicaid. Those with and without OUD had relatively similar incomes with approximately half in each cohort having a median income in the 25th percentile nationally. OUD was more common in Black patients, those with a higher burden of comorbidities, Medicare and Medicaid patients, and those hospitalized in the US Western region.
Primary Outcomes, Cohort 1
Mean LOS for all VOC hospitalizations was 5.01 days, while mean LOS for VOC in those with OUD was 6.16 days. Those without OUD had a significantly shorter mean LOS (4.90 days) which was significant prior to and after adjusting for confounding variables (p’s < 0.001). Mean cost was significantly higher in those with OUD ($9076) compared to those without OUD ($8020) (p < 0.001). After adjusting for confounding variables, mean cost in patients with OUD remained significantly increased (p < 0.001) (Table 2).
Secondary Outcomes, Cohort 1
In total, 600 deaths were recorded in VOC hospitalizations, 30 (5%) of which occurred in patients with OUD. Mortality in all VOC hospitalizations was 0.2% and was decreased in patients with OUD (0.1%) compared to those without OUD (0.2%), although the difference was not statistically significant (p = 0.180). After adjusting for confounding variables, mortality remained decreased in those with OUD, but the difference was again not statistically significant (aOR = 0.64, 95% CI 0.28–1.48, p = 0.295).
Associated Clinical Factors for an OUD in VOC (Cohort 2)
In hospitalizations for VOC, increased comorbidity index was associated with a secondary diagnosis of OUD in a multivariable assessment while age, non-Black race, and sex were not associated with OUD (Table 3). In contrast, for hospitalizations for all other reasons (Cohort 2), younger age, male sex, and non-Black race were all associated with the presence of OUD in multivariable and univariable analyses (Table 3 and Table S2). Similarly, income was not associated with OUD in those hospitalized for VOC but was significantly associated with OUD in all other hospitalizations with the lower income patients having higher rates of OUD.
OUD and Non-VOC Hospitalization Outcomes (Cohort 2)
A diagnosis of OUD was present in 2.2% of non-VOC hospitalizations. As in our patients with OUD and VOC, LOS (mean 4.73 days vs 5.96 days, p < 0.001) and cost (mean $13,236 vs $13,340, p < 0.001) were increased in those with OUD after adjusting for confounding variables (Table S3). In hospitalizations for all reasons other than VOC, a secondary diagnosis of OUD was associated with an increase in mortality (aOR = 1.08, 95% CI 1.05–1.11, p < 0.001).
DISCUSSION
The clinical implication of OUD and its association with outcomes in patients presenting with VOC were previously unknown. Here, in the first assessment of OUD and outcomes in VOC hospitalizations, our principal findings were that OUD was associated with increased markers of healthcare utilization (LOS and hospital costs). While not significantly different, there was a signal of potentially lower mortality in those with OUD and VOC, with 36% lower odds (aOR 0.64) of mortality with OUD, in contrast to the higher mortality associated with OUD (aOR 1.08) in those with OUD hospitalized for causes other than VOC.
Our major findings, persisting after adjustment for numerous covariates, were focused on the association between OUD and increases in LOS and costs in VOC hospitalizations. These differences were considerable, with a 24% increase in LOS and 11% cost increase per hospitalization. One potential explanation would be deficient use of opiates for pain control with a known OUD. Because inadequate pain control for VOC has been associated with high readmission rates,20 we hypothesize that a diagnosis of OUD may, with deficient use of opioids, lead to an increased LOS from poor pain control. Similarly, a patient with historically difficult-to-treat pain may be more likely to be given an OUD diagnosis (even if one is not present), and they may have a longer LOS simply because of their pain being hard to control.
Despite the increases in LOS and costs, OUD was not associated with increased mortality in patients with VOC, and in fact, mortality appeared to be lower (aOR 0.64), although not significantly so. In contrast, OUD was associated with increased mortality in patients hospitalized for other reasons. Of note, recent literature has shown opioids to be a relatively uncommon cause of death in patients with SCD and that those who suffer from migraines, individuals with chronic back pain, and patients with fibromyalgia all have a higher proportion of death secondary to opioids than patients with SCD.23,39 Our interpretations of possible reasons for the lower odds of mortality are limited due to the cause of inpatient death not being available in the NIS. Patients with SCD may be more familiar with how to self-manage opioids for their pain in comparison to patients without SCD due to the exposure to opioids over many years in patients with SCD. This could lead to less risk for overdose in patients with SCD compared to others. To be further investigated is the possibility that opiates are protective in SCD against adverse events that might culminate in mortality.
Similar to hospitalizations for VOC, OUD was associated with increased LOS and cost in non-VOC hospitalizations (Cohort 2). However, associated factors related to OUD differed in those hospitalized with VOC compared to non-VOC hospitalizations. Previously described31,40 clinically associated factors for OUD such as younger age, male sex, and white race were confirmed in our cohort hospitalized for reasons other than VOC but were not found to be associated with OUD in VOC hospitalizations. Additionally, while lower income was associated with OUD in the non-VOC cohort, no association between income and OUD was present in the VOC cohort. The differences in associated variables for OUD in those with VOC provide further evidence that OUD may not have the same clinical meaning in patients with SCD and that interpretation requires putting the diagnosis of OUD in the context of the patient’s pain experience and their opportunity to receive adequate analgesia. The increase in OUD in Black SCD patients also raises further concerns for provider bias when evaluating for problematic opioid use. Black patients being treated for VOC have reported feeling that they receive worse care10,41 due to their race; thus, racial bias may also contribute to undertreatment of VOC pain throughout their lives.
Relationship to Burnout, and the Benefit of Pain Plans
Treatment of VOC is challenging, and it can be made even more challenging when patient-provider trust is not present. A small proportion (10–20%) of patients with SCD constitute approximately half of VOC admissions and providers are at high risk for burnout (see Burstein’s scoping review showing the possible relationship of burnout to not being able to care for patients, JGIM 202242) when feeling like they are not helping this group of patients-in-need.4,7,17,43 Opioids are generally accepted as indicated for severe acute pain even in patients with OUD; however, this too can be related to providers experiencing burnout or moral injury after feeling like they may be harming a patient.44,45 Individualized pain plans for VOC have been shown to improve patient outcomes including time to first opioid use, LOS, and readmission rates.46,47 We would advocate for the implementation of pain plans developed through shared decision-making based on previous response to pain medications in those with VOC and OUD beginning during their first VOC. Plans that document a suggested initial regimen and a standard approach to escalation would provide guidance for providers who are unfamiliar with the patient and could resolve delays in treatment caused by concerns for addiction and cautious prescribing. Effectively utilized, these plans could improve both patient and provider outcomes.12,17,24,48,49 Other mechanisms to address OUD in SCD would include monitoring patient controlled substance use through Patient Drug Monitoring Programs and referring patients to pain management specialists with experience in treating communities traditionally mistrusted for adherence to regimens.
Our Study Has Both Strengths and Limitations
This study was limited by the administrative nature of the NIS which does not provide narrative assessments of encounters or laboratory data. The available information did not allow us to assess important aspects of care such as time to first opioid received. In addition, NIS data does not provide patient identifiers; thus, it did not allow for performing mixed-effect models to account for recurrent hospitalizations for the same patients. Given the large proportion of VOC hospitalizations in a relatively smaller number of patients, many patients likely contributed multiple hospitalizations to these findings. Strengths include the very large sample with a large geographic representation across the US.
These Findings Lead to Several Implications and Recommendations
While opioids are indicated for the management of acute VOC pain, the findings suggest a complex relationship between providers’ desires to treat pain and a potential worry about exacerbating or not acknowledging possible opiate dependence. For these or other reasons, there is a clear relationship between OUD, longer hospital stays, and increased costs in SCD patients with VOC, without a corresponding increase in mortality. Developing individual pain management plans based on shared decision making and acknowledging a patient’s prior experiences would allow for better alignment of patients and clinicians around treatment goals in acute management of VOC. Future studies should further explore these relationships, the benefits of pain management plans, and possible presence of and reasons for a mortality benefit from OUD which could better inform pain management in SCD both inside and outside the hospital.
Data Availability:
The data supporting the findings of this study are publicly available.
References
Kang HA, Barner JC, Richards KM, Bhor M, Paulose J, Kutlar A. Association Between Vaso-Occlusive Crises and Opioid Prescriptions Among Patients with Sickle Cell Disease: A Retrospective Claims-Based Study. J Health Econ Outcomes Res. 2020;7(1):94-101.
Ballas SK. Opioids and Sickle Cell Disease: From Opium to the Opioid Epidemic. J Clin Med. 2021;10(3).
Yawn BP, Buchanan GR, Afenyi-Annan AN, et al. Management of sickle cell disease: summary of the 2014 evidence-based report by expert panel members. JAMA. 2014;312(10):1033-48.
Carroll CP. Opioid treatment for acute and chronic pain in patients with sickle cell disease. Neurosci Lett. 2020;714:134534.
Carroll CP, Lanzkron S, Haywood C, Jr., et al. Chronic Opioid Therapy and Central Sensitization in Sickle Cell Disease. Am J Prev Med. 2016;51(1 Suppl 1):S69-77.
Telfer P, Bahal N, Lo A, Challands J. Management of the acute painful crisis in sickle cell disease- a re-evaluation of the use of opioids in adult patients. Br J Haematol. 2014;166(2):157-64.
Field JJ. Five lessons learned about long-term pain management in adults with sickle cell disease. Hematology Am Soc Hematol Educ Program. 2017;2017(1):406-11.
Cooper TE, Hambleton IR, Ballas SK, Johnston BA, Wiffen PJ. Pharmacological interventions for painful sickle cell vaso-occlusive crises in adults. Cochrane Database Syst Rev. 2019;2019(11).
Brandow AM, Carroll CP, Creary S, et al. American Society of Hematology 2020 guidelines for sickle cell disease: management of acute and chronic pain. Blood Adv. 2020;4(12):2656-701.
Ruta NS, Ballas SK. The Opioid Drug Epidemic and Sickle Cell Disease: Guilt by Association. Pain Med. 2016;17(10):1793-8.
Shapiro BS, Benjamin LJ, Payne R, Heidrich G. Sickle cell-related pain: perceptions of medical practitioners. J Pain Symptom Manage. 1997;14(3):168-74.
Sagi V, Mittal A, Tran H, Gupta K. Pain in sickle cell disease: current and potential translational therapies. Transl Res. 2021;234:141-58.
Linton EA, Goodin DA, Hankins JS, et al. A Survey-Based Needs Assessment of Barriers to Optimal Sickle Cell Disease Care in the Emergency Department. Ann Emerg Med. 2020;76(3S):S64-S72.
Centers for Disease Control and Prevention. (2023, July 6). Data & statistics on Sickle Cell Disease. https://www.cdc.gov/ncbddd/sicklecell/data.html. Accessed 6/30/2023.
Meghani SH, Byun E, Gallagher RM. Time to take stock: a meta-analysis and systematic review of analgesic treatment disparities for pain in the United States. Pain Med. 2012;13(2):150-74.
Adams G, Salomons TV. Attending work with chronic pain is associated with higher levels of psychosocial stress. Can J Pain. 2021;5(1):107-16.
Brown SE, Weisberg DF, Balf-Soran G, Sledge WH. Sickle cell disease patients with and without extremely high hospital use: pain, opioids, and coping. J Pain Symptom Manage. 2015;49(3):539-47.
Kavanagh PL, Fasipe TA, Wun T. Sickle Cell Disease: A Review. JAMA. 2022;328(1):57-68.
Salsitz EA. Chronic Pain, Chronic Opioid Addiction: a Complex Nexus. J Med Toxicol. 2016;12(1):54-7.
Feliu MH, Wellington C, Crawford RD, et al. Opioid management and dependency among adult patients with sickle cell disease. Hemoglobin. 2011;35(5-6):485-94.
Smith WR, McClish DK, Roberts JD, et al. Prescription Opioid Misuse Index in sickle cell patients: A brief questionnaire to assess at-risk for opioid abuse. J Opioid Manag. 2019;15(4):323-31.
Bolshakova M, Bluthenthal R, Sussman S. Opioid use and misuse: health impact, prevalence, correlates and interventions. Psychol Health. 2019;34(9):1105-39.
Ballas SK, Kanter J, Agodoa I, et al. Opioid utilization patterns in United States individuals with sickle cell disease. Am J Hematol. 2018;93(10):E345-E7.
Elander J, Lusher J, Bevan D, Telfer P. Pain management and symptoms of substance dependence among patients with sickle cell disease. Soc Sci Med. 2003;57(9):1683-96.
Russo K, Chhunchha P. Patient-Controlled Analgesia vs Intravenous Push Hydromorphone for Pain Management of Vaso-Occlusive Crisis Associated With Sickle Cell Disease. J Pain Palliat Care Pharmacother. 2023;37(2):116-22.
Katsivalis KV, Kosacz J, Austin Szwak J. Opioid Use in Vaso-Occlusive Crisis During Intravenous Opioid Drug Shortage. Hosp Pharm. 2022;57(6):721-6.
Summers S, Grau L, Massel D, Rosas S, Ong A, Hernandez VH. Opioid Use Disorders Are Associated With Perioperative Morbidity and Mortality in the Hip Fracture Population. J Orthop Trauma. 2018;32(5):238-44.
Gharbin J, Winful A, Hassan MA, et al. Differences in the Clinical Outcome of Ischemic and Nonischemic Cardiomyopathy in Heart Failure With Concomitant Opioid Use Disorder. Curr Probl Cardiol. 2023;48(5):101609.
Shaikh AS, Al Mouslmani MY, Raza Shah A, et al. Preexisting opioid use disorder is associated with poor outcomes in hospitalized acute pancreatitis patients. Eur J Gastroenterol Hepatol. 2021;33(11):1348-53.
Wilson JD, Lanzkron S, Pecker LH, Bediako SM, Han D, Beach MC. Psychosocial and Clinical Risk Factors Associated with Substance Use in Observational Cohort of Patients with Sickle Cell Disease. Subst Use Misuse. 2020;55(13):2205-12.
Webster LR. Risk Factors for Opioid-Use Disorder and Overdose. Anesth Analg. 2017;125(5):1741-8.
Song Y, Tang R, Roses RE, et al. Opioid Use Disorder is Associated With Complications and Increased Length of Stay After Major Abdominal Surgery. Ann Surg. 2021;274(6):992-1000.
Medicaid Outcomes Distributed Research N, Donohue JM, Jarlenski MP, et al. Use of Medications for Treatment of Opioid Use Disorder Among US Medicaid Enrollees in 11 States, 2014-2018. JAMA. 2021;326(2):154-64.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613-9.
Gutacker N, Bloor K, Cookson R. Comparing the performance of the Charlson/Deyo and Elixhauser comorbidity measures across five European countries and three conditions. Eur J Public Health. 2015;25 Suppl 1:15-20.
McCavit TL, Lin H, Zhang S, Ahn C, Quinn CT, Flores G. Hospital volume, hospital teaching status, patient socioeconomic status, and outcomes in patients hospitalized with sickle cell disease. Am J Hematol. 2011;86(4):377-80.
Pokhrel A, Olayemi A, Ogbonda S, Nair K, Wang JC. Racial and ethnic differences in sickle cell disease within the United States: From demographics to outcomes. Eur J Haematol. 2023;110(5):554-63.
Kumar V, Chaudhary N, Achebe MM. Epidemiology and Predictors of all-cause 30-Day readmission in patients with sickle cell crisis. Sci Rep. 2020;10(1):2082.
Ballas SK. Opioids are not a major cause of death of patients with sickle cell disease. Ann Hematol. 2021;100(5):1133-8.
Lee SW, Shen J, Kim SJ, et al. US Trends of Opioid-use Disorders and Associated Factors Among Hospitalized Patients With Spinal Conditions and Treatment From 2005 to 2014. Spine (Phila Pa 1976). 2020;45(2):124-33.
Osborne JC, Osakwe Z, Odlum M. Opioid Use in Adults With Sickle Cell Disease Hospitalized During Vaso-Occlusive Crisis: A Systematic Review. J Hematol. 2021;10(2):46-52.
Burstein DS, Svigos F, Patel A, et al. A Scoping Review on the Concept of Physician Caring. J Gen Intern Med. 2022;37(12):3134-46.
Lanzkron S, Carroll CP, Haywood C, Jr. The burden of emergency department use for sickle-cell disease: an analysis of the national emergency department sample database. Am J Hematol. 2010;85(10):797-9.
The ASAM National Practice Guideline for the Treatment of Opioid Use Disorder: 2020 Focused Update. J Addict Med. 2020;14(2S Suppl 1):1–91.
Dowell D, Ragan KR, Jones CM, Baldwin GT, Chou R. CDC Clinical Practice Guideline for Prescribing Opioids for Pain - United States, 2022. MMWR Recomm Rep. 2022;71(3):1-95.
Mager A, Pelot K, Koch K, et al. Opioid management strategy decreases admissions in high-utilizing adults with sickle cell disease. J Opioid Manag. 2017;13(3):143-56.
Della-Moretta S, Delatore L, Purcell M, et al. The Effect of Use of Individualized Pain Plans in Sickle Cell Patients Presenting to the Emergency Department. Ann Emerg Med. 2020;76(3S):S21-S7.
Pecker LH, Darbari DS. Psychosocial and affective comorbidities in sickle cell disease. Neurosci Lett. 2019;705:1-6.
Welch-Coltrane JL, Wachnik AA, Adams MCB, et al. Implementation of Individualized Pain Care Plans Decreases Length of Stay and Hospital Admission Rates for High Utilizing Adults with Sickle Cell Disease. Pain Med. 2021;22(8):1743-52.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest:
Dr. Linzer is supported through his employer, Hennepin Healthcare, for burnout reduction projects by the AMA, IHI, and the Optum Office for Provider Advancement, as well as other large health systems. The other authors have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These findings have not been presented previously.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sanni, A., Goble, S., Gilbertson, D.T. et al. The Associations Between Opioid Use Disorder and Healthcare-Related Outcomes in Vaso-occlusive Crisis. J GEN INTERN MED 39, 1666–1672 (2024). https://doi.org/10.1007/s11606-024-08717-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-024-08717-7