Abstract
Background
Anti-obesity medications (AOMs) can be initiated in conjunction with participation in the VA national behavioral weight management program, MOVE!, to help achieve clinically meaningful weight loss.
Objective
To compare weight change between Veterans who used AOM + MOVE! versus MOVE! alone and examine AOM use, duration, and characteristics associated with longer duration of use.
Design
Retrospective cohort study using VA electronic health records.
Participants
Veterans with overweight or obesity who participated in MOVE! from 2008–2017.
Main Measures
Weight change from baseline was estimated using marginal structural models up to 24 months after MOVE! initiation. The probability of longer duration of AOM use (≥ 180 days) was estimated via a generalized linear mixed model.
Results
Among MOVE! participants, 8,517 (1.6%) used an AOM within 24 months after MOVE! initiation with a median of 90 days of cumulative supply. AOM + MOVE! users achieved greater weight loss than MOVE! alone users at 6 (3.2% vs. 1.6%, p < 0.001), 12 (3.4% vs. 1.4%, p < 0.001), and 24 months (2.7% vs. 1.5%, p < 0.001), and had a greater probability of achieving ≥ 5% weight loss at 6 (38.8% vs. 26.0%, p < 0.001), 12 (43.1% vs. 28.4%, p < 0.001), and 24 months (40.4% vs. 33.3%, p < 0.001). Veterans were more likely to have ≥ 180 days of supply if they were older, exempt from medication copays, used other medications with significant weight-gain, significant weight-loss, or modest weight-loss side effects, or resided in the West North Central or Pacific regions. Veterans were less likely to have ≥ 180 days of AOM supply if they had diabetes or initiated MOVE! later in the study period.
Conclusions
AOM use following MOVE! initiation was uncommon, and exposure was time-limited. AOM + MOVE! was associated with a higher probability of achieving clinically significant weight loss than MOVE! alone.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The combined prevalence of overweight (37%) and obesity (41%) in Veterans receiving care in the Veterans Health Administration (VA) is greater than the prevalence in the general US population (72%).1, 2 To help Veterans manage their weight, the VA implemented the MOVE! Weight Management Program for Veterans (MOVE!), a system-wide comprehensive lifestyle intervention, with adjunctive treatment (e.g., anti-obesity medications (AOMs) and bariatric surgery) in some instances.3 Prior studies have found that 25% of MOVE! participants achieve clinically meaningful (i.e., ≥ 5%) weight loss at one year.4, 5 Veterans with more intensive participation achieve greater weight loss, with studies citing up to 30% achieving clinically meaningful weight loss at one year.4
Since behavioral weight management is associated with modest weight loss and bariatric surgery is provided to only 1% of eligible patients each year, AOMs are an important population management strategy.6 Randomized trials have shown when adhered to, AOMs induce 6–11% reductions in baseline weight.7 Several studies show compared to behavioral intervention alone, AOMs combined with behavioral intervention increase the likelihood of achieving ≥ 5% weight loss.8,9,10,11 Whether Veterans receiving VA care achieve clinically meaningful weight loss with AOMs has received little study.
Despite the potential utility of AOMs, only 1–2% of the general population initiate an AOM.12 This is due to a variety of barriers, including insurance coverage restrictions and provider-facing issues related to safety, AOM knowledge, and weight bias.13 Rates of AOM initiation are similarly low in VA.3, 14 One potential barrier to initiation for Veterans was the VA policy requiring 90 days of MOVE! participation to become eligible for an AOM; since July 2016, this is no longer required.9
It is important to understand the impact of AOM use in combination with MOVE! as VA has facilitated greater access to AOMs, and interest in AOMs is increasing with approval of semaglutide for weight loss.15 A recent study of MOVE! participants in 2010–2020 foundAOM users lost more weight and had lower blood sugar, blood pressure, and cholesterol than non-users.11 However, this study was limited to a subgroup who initiated AOM within one month of MOVE! initiation, despite the prior requirement of 90 days of MOVE! participation before eligibility for AOM use.11 We build upon prior literature by examining the larger group of all AOM users and comparing weight change between AOM + MOVE! users and MOVE! users to describe the real-world effectiveness of AOMs and predictors of AOM use following MOVE! participation. Based on a prior call to understand duration of AOM use and who may be more likely to benefit,14 we also describe the use and duration of exposure to AOMs and identify factors associated with duration of exposure. These results will inform an important evidence gap in real-world AOM exposure and impacts.
Methods
Study Population and Data
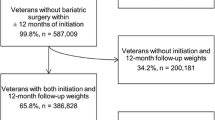
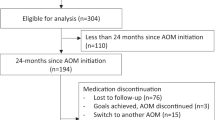
This retrospective cohort study used VA electronic health record data and included Veterans with overweight or obesity who initiated MOVE! in FY2008-2017. MOVE! participants were included if they had ≥ 1 body mass index (BMI) value of ≥ 25 in the two years before their initial MOVE! visit, which served as their index date; resided in the US; and had a valid ZIP code (Supplemental Fig. 1). MOVE! participants were excluded if they had a recorded death before or on index date, were institutionalized (hospital or nursing home) at time of index, had a cancer diagnosis within 5 years before index, had an amputation before index, or received an AOM in the 2 years before index. The duration analysis sample included 8,517 MOVE! participants who initiated AOMs and 534,581 MOVE! participants who did not initiate AOMs. For the weight-change analysis, Veterans without ≥ 1 weight measurement within 24 months after their index MOVE! visit were dropped, resulting in an analytic sample of 523,971.
Exposure, Outcomes, and Covariates
AOM use was identified based on ≥ 1 fill of one of eight AOMs (orlistat, lorcaserin, phentermine-topiramate, naltrexone-bupropion, liraglutide, phentermine, diethylpropion, sibutramine). For the weight-change analysis, AOM use was operationalized as a binary time-varying variable that was positive if a Veteran had ≥ 1 AOM fill, since the objective was to compare AOM + MOVE! to MOVE! alone. Thus, taking an intention-to-treat approach to compare AOM + MOVE! to MOVE! alone, Veterans were considered “exposed” even if they discontinued AOM during the 24-month interval.
For the comparison of AOM + MOVE! users and MOVE! users, the primary clinical outcome was percentage weight loss from baseline (i.e., MOVE! initiation), which was examined at 6-, 12-, 18-, and 24-months following MOVE! initiation. We also examined the proportion of Veterans who achieved ≥ 5% weight loss at the same time points. Unadjusted percentage weight loss from baseline was also reported for each AOM.
Medication outcomes of interest included number of prescription fills and total days supply of AOM in the 24 months after MOVE! initiation. For AOM users, a binary outcome was constructed of total AOM days supply for ≥ 180 days in the 24 months following MOVE! initiation to represent longer duration of use, identified as the 75th percentile.
We constructed several baseline patient characteristics associated with weight change identified in prior research, including demographics, clinical factors, and prior healthcare use.16 Demographic factors included age, sex, race, Hispanic/Latino ethnicity, marital status, enrollment priority group, Medicare eligibility, Medicaid eligibility, census division, and distance to closest VA. Clinical factors included the VA comorbidity summary score called Nosos17 and 17 conditions diagnosed in the year before index date. Other clinical factors included closest BMI and weight before or on MOVE! initiation date, fiscal year of MOVE! initiation and use of medications (e.g., antihyperglycemics, antidepressants) in the prior six months that had potential for significant weight-gain (≥ 3 kg [kg]18), significant weight-loss (≥ 3 kg), modest weight-gain (< 3 kg), or modest weight-loss (< 3 kg) side effects. These medication lists were put together after literature review by study team members.18,19,20,21,22,23,24 Healthcare use factors included hospitalization, inflation-adjusted VA costs, and the number of primary care, specialty care, and mental health visits in the fiscal year before the fiscal year of MOVE! initiation.
Analysis
Characteristics of AOM users and non-users and the medication use outcomes (fills, days supply) were evaluated descriptively for each AOM. Characteristics associated with the binary outcome of total AOM supply ≥ 180 days in the 24 months after MOVE! initiation were examined in a generalized linear mixed model with logit link and binomial error distribution, adjusting for clustering by VA facility.
To compare weight change in the 24 months following MOVE! initiation of AOM users and non-users, we used marginal structural modeling (MSM).25 This approach generates inverse probability of treatment weights (IPTWs) to handle time-varying treatments (e.g., AOM) and time-varying confounders (e.g., number of MOVE! visits) that could influence both the timing of AOM initiation and subsequent weight change. Time-varying IPTWs for the probability of AOM initiation at each healthcare visit were generated using random survival forest (RSF)26 with 100 trees, as this produces less biased estimates than standard and semi-parametric and techniques27 and impose no assumptions on the survival function, such as proportional hazards.
To generate stabilized IPTW, we modeled time until initiating AOM in two models: a numerator model and a denominator model.28 The numerator model included only baseline variables as predictors, specifically age, gender, marital status, race, ethnicity, enrollment priority, census division, distance to nearest VA, four indicators for use of medication with significant (≥ 3 kg) or modest (< 3 kg) weight-gain or weight-loss, indicators for 17 prior-year comorbidities, and year of index date. The denominator model included the same predictors as well as two time-varying predictors of AOM initiation: percent weight change and number of MOVE! visits from baseline up to the beginning of the present interval.
The ensuing structural modeling of percent weight change from baseline during the 24-months post-MOVE! initiation was conducted using weighted generalized additive mixed models (GAMM). Percent weight change from baseline was modeled via a linear model, and probability of ≥ 5% decrease in baseline weight was modeled in a second logistic GAMM. Linear contrasts within the context of the model were examined at 6-, 12-, 18-, and 24-month time points to quantify the effect of AOM. After truncating the IPTW at 0.1% and 99.9%, the IPTW ranged from 0.21 to 10.56, with a mean of 1.04.
Descriptive analyses and logistic models were conducted using SAS Enterprise Guide 8.3. Marginal structural modeling was conducted using R (version 4.2.0). The ‘LTRCforests’ package26 was used to conduct random survival forest analyses, and the ‘gamm4’ package (version 0.2–6) was used to analyze GAMM models. This study was approved by Durham VA Health Care System Institutional Review Board.
Results
Patient Characteristics and AOM Use
Among 543,098 Veterans who used MOVE! between 2008 and 2017, 8,517 (1.6%) had one or more AOM prescriptions in VA within 24 months after MOVE! initiation. Compared to non-users (Table 1), AOM users were younger (mean age = 51.6 vs. 55.6, standardized mean difference [SMD] = 0.34) and had a higher baseline BMI (mean = 39.3 kg/m2 vs. 35.4 kg/m2, SMD = 0.58). AOM users were more likely to be classified as Black (28.1% vs. 23.8%, SMD = 0.11), but less likely to be male (71.6% vs. 86.5%, SMD = 0.37) or enrolled in Medicare (29.7% vs. 37.9%, SMD = 0.18).
AOM Exposure
Across the study period, the most used AOM was orlistat (83%), followed by phentermine-topiramate (6%) and naltrexone-bupropion (5%). Between 2008 and 2013, almost all AOM use was orlistat, which declined to 42% by 2017 (Supplemental Fig. 2) as more AOMs became available. In the two years after MOVE! initiation (Table 2), AOM users on average used one AOM, with a mean of 3.8 AOM prescription fills (median = 3 fills) and a mean of 135 days of supply (median = 90 days). Phentermine-topiramate and liraglutide users had a higher mean (157 and 183 days, respectively) and median day supply (106 and 150 days, respectively).
Among AOM initiators (Table 3), Veterans were more likely to have ≥ 180 days of cumulative supply if they were older (adjusted odds ratio [aOR] = 1.02, 95% confidence interval [CI]: 1.01–1.02); exempt from medication copays (aOR = 1.16, 95% CI: 1.03–1.29); used medications with potential significant weight-gain (aOR = 1.22, 95% CI: 1.09–1.37), weight-loss (aOR = 1.19, 95% CI: 1.04–1.37), or modest weight-loss (aOR = 1.17, 95% CI: 1.04–1.32) side effects; or resided in the West North Central (aOR = 1.53, 95% CI: 1.13–2.09) or Pacific census divisions (aOR = 1.57, 95% CI: 1.11–2.21). Veterans were less likely to have ≥ 180 days of AOM supply if they had diabetes (aOR = 0.80, 95% CI: 0.70–0.91) or MOVE! initiation later in the study period (all aORs except 2016 and 2017 significantly < 1.00 for years after 2009 vs. 2008).
Differences in Weight Change for AOM + MOVE! versus MOVE! alone
In adjusted analysis (Fig. 1), AOM + MOVE! was associated with significantly greater weight loss than MOVE! at 6 months after MOVE! initiation (3.2% of index body weight for AOM vs. 1.6% for no AOM), resulting in a 1.6% point difference [95% CI: 1.40–1.80]. Significantly greater loss among AOM initiators persisted at 12 months (3.4% vs. 1.4%, 1.98% point difference [95% CI: 1.81–2.16]), 18 months (3.0% vs. 1.5%, 1.53% point difference [95% CI: 1.34–1.71), and 24 months after MOVE! initiation (2.7% vs. 1.5%, 1.18% point difference [95% CI: 0.81–1.55]).
In the logistic model, AOM + MOVE! was associated with significantly greater odds of ≥ 5% weight reduction at 6 months (aOR = 1.80, 95% CI: 1.73–1.88), 12 months (aOR = 1.91, 95% CI: 1.85–1.98), 18 months (aOR = 1.51, 95% CI: 1.46–1.57), and 24 months (aOR = 1.36, 95% CI: 1.27–1.45). The corresponding modeled probabilities of a given patient achieving ≥ 5% reduction are depicted in Figure 2. According to these, the probability of ≥ 5% reduction in baseline weight was 38.8% (95% CI: 37.7%-39.8%) for AOM + MOVE! vs. 26.0% (95% CI: 25.6%-26.3%) for MOVE! alone at 6 months; 43.1% (95% CI: 42.2%-44.0%) vs. 28.4% (95% CI: 28.0%-28.7%) at 12 months; 41.3% vs. 31.7% (95% CI: 31.3%-32.1%) at 18 months, and 40.4% (95% CI: 38.7%-42.1%) vs. 33.3% (95% CI: 32.9%-33.7%) at 24 months. Supplemental Fig. 3 shows unadjusted percentage weight loss from baseline stratified by AOM used.
Discussion
This real-world study of a national cohort of Veterans who initiated MOVE! from 2008 to 2017 found AOM + MOVE! led to greater mean weight loss in the two years after MOVE! initiation than MOVE! alone (2.7% vs. 1.5% at 2 years). Most (83%) of the AOM + MOVE! cohort were taking orlistat, so these results generalize primarily to orlistat users. The 3.4% loss of baseline weight for Veterans taking AOMs at 12 months is comparable to the 3.1% loss reported in a meta-analysis of 57 orlistat trials that provided AOMs with lifestyle intervention,7 suggesting real-world weight loss associated with AOM + MOVE! approximates that from AOM use alone. On average, MOVE! is associated with modest weight loss effects (0.13–3.3 kg at 12 months),4, 29 suggesting the greater weight loss seen in the AOM + MOVE! cohort may have been associated with AOM use. More intensive MOVE! participation is associated with more weight loss,4, 29 so the combined weight-loss effects of AOM use with increased MOVE! participation could be larger.
We also found a higher estimated proportion of AOM + MOVE! users achieved ≥ 5% weight loss than users of MOVE! alone, which is consistent with a prior VA study using 2012–2016 data in which the unadjusted proportion achieving ≥ 5% weight loss at 5 months was 26% for MOVE! participants but 40% in the phentermine-topiramate + MOVE! group.30 A more recent study of 3,732 MOVE! participants in 2010–2020 found 39% of AOM users lost ≥ 5% weight at 12 months compared to 21% of matched nonusers.11 This suggests a substantial portion of AOM users lose ≥ 5% weight even if mean weight loss among all AOM users is < 5%.
Similar to a prior VA study, we also saw greater weight loss in the phentermine-topiramate + MOVE! group compared to the orlistat + MOVE! or lorcaserin + MOVE! groups.30 Compared to these latter two groups, our study also showed greater weight loss in the liraglutide + MOVE! and phentermine + MOVE! groups, however, these were descriptive analyses., A future comparative effectiveness trial comparing AOMs could help to determine which AOMs lead to greater weight loss.
Despite greater weight loss through 24 months after MOVE! initiation in the AOM + MOVE! cohort, we found AOM users had short duration of exposure (median = 90 days). A prior non-VA cohort study also found median duration of use of approximately 4 months12 and a prior meta-analysis of longer-term AOM clinical trials found high attrition rates (30–45% in all trials) and that users of longer-term AOMs were more likely to discontinue them compared to placebo due to an adverse event.31 Even among the AOMs indicated for longer-term use (i.e., orlistat, phentermine/topiramate, buprenorphine/naltrexone, liraglutide, and lorcaserin before market withdrawal), duration was generally short (3–5 months). It was unclear whether short duration of use was due to reasons related to side effects versus effectiveness. Manufacturer-provided prescribing information recommends patients discontinue these AOMs if they are unable to achieve ≥ 4% or 5% weight loss at 12–16 weeks. A better understanding of the adverse events experienced from real-world use of AOMs, as well as potential mental health and quality of life benefits, should be explored in future research.
We also found several patient characteristics were associated with longer duration of use (i.e., ≥ 180 days), including older age, being exempt from medication copays, not having diagnosed diabetes, and use of medications with potential for significant weight-gain or weight-loss side effects. Clinicians with patients initiating AOMs may want to consider tracking concurrent antidepressants, diabetes medications, or other medications with the potential for weight gain, since 30–40% of AOM users were taking such medications in the months leading up to MOVE! initiation. VA clinical practice guidelines recommend eliminating or reducing medications that induce weight-gain, suggesting there is room to discontinue and substitute with medications that are weight-neutral or even have weight-loss side effects.32 Given the short duration of AOM real-world use, identifying alternatives to weight gain-inducing medications may be a more sustainable, as well as complementary, approach to addressing obesity.
Barriers to AOM access need to be addressed for AOMs to become more integrated in population weight management. Unlike non-VA settings that often restrict AOM coverage, VA includes three of five FDA-approved AOMs in the national formulary. Yet our study and others find that AOM use in VA is very low.3, 33 Until 2016, VA required ≥ 90 days’ participation in MOVE! before receipt of AOM.30 Now, VA only requires conjunctive participation in a comprehensive lifestyle intervention, which may expand access.8, 30 There may also be provider-level barriers including concerns about safety, time constraints of routine visits, lack of confidence in providing weight loss treatments, weight bias, or insufficient knowledge about current AOMs.34 Providers lack of clarity about the available AOMs and their tradeoffs may be compounded by changes in available AOMs between 2010 and 2015 (sibutramine withdrawn in 2010, lorcaserin approved in 2012, phentermine-topiramate approved in 2012, and bupropion-naltrexone approved in 2014). With the availability of newer, more effective AOMs, future work should examine provider attitudes and preferences about AOMs and the effectiveness of these newer AOMs in real-world use among Veterans.
Several limitations must be acknowledged. Most AOM use (83%) in this study consisted of orlistat, so weight differences between AOM users and non-users may not generalize to patients taking more recently approved AOMs. As the use of newer AOMs increases, assessment of weight change from these AOMs will be needed. This study also included AOMs available during the study period but were at some point removed from the market (sibutramine in 2010, lorcaserin in 2020), although this may not bias results significantly since their combined prevalence was low (6%).Despite applying MSMs to increase comparability between the two cohorts, there may be unobserved confounding such as patients’ lifestyle behaviors, psychological characteristics, or weight loss expectations at MOVE! initiation. Additionally, when identifying combination AOMs, such as buprenorphine/naltrexone and phentermine/topiramate, we included single-agent prescriptions if filled within 30 days of one another similar to a prior study.3 It is possible that we missed some AOM use if single-agent prescriptions were not filled within 30 days of one another. However, some single agents (i.e., buprenorphine, naltrexone, and topiramate) have other common uses (e.g., depression, seizures). Finally, AOMs that were obtained outside of VA and not paid for by VA were not captured.
Conclusion
This nationwide VA study found that AOM use following MOVE! initiation was uncommon and exposure was time-limited but that AOM + MOVE! was associated with a higher probability of achieving clinically significant weight loss than MOVE! alone.
References
Breland JY, Phibbs CS, Hoggatt KJ, et al. The Obesity Epidemic in the Veterans Health Administration: Prevalence Among Key Populations of Women and Men Veterans. J Gen Intern Med. 2017;32(Suppl 1):11-17. doi:https://doi.org/10.1007/s11606-016-3962-1
National Center for Health Statistics (US). Health, United States, 2016: with chartbook on long-term trends in health 2017 Report No.: 2017–1232.
Thomas DD, Waring ME, Ameli O, Reisman JI, Vimalananda VG. Patient Characteristics Associated with Receipt of Prescription Weight‐Management Medications Among Veterans Participating in MOVE! Obesity. Published online May 15, 2019:oby.22503. doi:https://doi.org/10.1002/oby.22503
Maciejewski ML, Shepherd-Banigan M, Raffa SD, Weidenbacher HJ. Systematic Review of Behavioral Weight Management Program MOVE! for Veterans. Am J Prev Med. 2018;54(5):704-714. doi:https://doi.org/10.1016/j.amepre.2018.01.029
Kahwati LC, Lance TX, Jones KR, Kinsinger LS. RE-AIM evaluation of the Veterans Health Administration’s MOVE! Weight Management Program. Transl Behav Med. 2011;1(4):551-560. doi:https://doi.org/10.1007/s13142-011-0077-4
Gasoyan H, Tajeu G, Halpern MT, Sarwer DB. Reasons for underutilization of bariatric surgery: The role of insurance benefit design. Surg Obes Relat Dis Off J Am Soc Bariatr Surg. 2019;15(1):146-151. doi:https://doi.org/10.1016/j.soard.2018.10.005
Shi Q, Wang Y, Hao Q, et al. Pharmacotherapy for adults with overweight and obesity: a systematic review and network meta-analysis of randomised controlled trials. The Lancet. 2022;399(10321):259-269. doi:https://doi.org/10.1016/S0140-6736(21)01640-8
Pendse J, Vallejo‐García F, Parziale A, Callanan M, Tenner C, Alemán JO. Obesity Pharmacotherapy is Effective in the Veterans Affairs Patient Population: A Local and Virtual Cohort Study. Obesity. 2021;29(2):308-316. doi:https://doi.org/10.1002/oby.23075
Hood S. Evaluation of Pharmacologic Interventions for Weight Management in a Veteran Population. Fed Pract. 2021;(38 No. 5). doi:https://doi.org/10.12788/fp.0117
Pantalone KM, Smolarz BG, Ramasamy A, et al. Effectiveness of Combining Antiobesity Medication With an Employer-Based Weight Management Program for Treatment of Obesity: A Randomized Clinical Trial. JAMA Netw Open. 2021;4(7):e2116595. doi:https://doi.org/10.1001/jamanetworkopen.2021.16595
Garvey WT, Cheng M, Ramasamy A, et al. Clinical and Cost Benefits of Anti-Obesity Medication for US Veterans Participating in the MOVE! Weight Management Program. Popul Health Manag. 2023;26(1):72-82. doi:https://doi.org/10.1089/pop.2022.0227
Saxon DR, Iwamoto SJ, Mettenbrink CJ, et al. Antiobesity Medication Use in 2.2 Million Adults Across Eight Large Health Care Organizations: 2009-2015. Obes Silver Spring Md. 2019;27(12):1975-1981. doi:https://doi.org/10.1002/oby.22581
Obesity Is A Chronic Disease: Instead Of Punishing Patients, Provide Access To Treatment. Published online August 18, 2022. doi:https://doi.org/10.1377/forefront.20220817.855384
Semla TP, Ruser C, Good CB, et al. Pharmacotherapy for Weight Management in the VHA. J Gen Intern Med. 2017;32(S1):70-73. doi:https://doi.org/10.1007/s11606-016-3949-y
Xie Z, Yang S, Deng W, Li J, Chen J. Efficacy and Safety of Liraglutide and Semaglutide on Weight Loss in People with Obesity or Overweight: A Systematic Review. Clin Epidemiol. 2022;14:1463-1476. doi:https://doi.org/10.2147/CLEP.S391819
Maciejewski ML, Arterburn DE, Van Scoyoc L, et al. Bariatric Surgery and Long-term Durability of Weight Loss. JAMA Surg. 2016;151(11):1046-1055. doi:https://doi.org/10.1001/jamasurg.2016.2317
Nosos Risk Adjustment. U.S. Department of Veterans Affairs. Aug 30, 2022. Available from: https://www.herc.research.va.gov/include/page.asp?id=risk-adjustment. Accessed 1 May 2023
Wharton S, Raiber L, Serodio KJ, Lee J, Christensen RA. Medications that cause weight gain and alternatives in Canada: a narrative review. Diabetes Metab Syndr Obes Targets Ther. 2018;11:427-438. doi:https://doi.org/10.2147/DMSO.S171365
Apovian CM, Aronne LJ, Bessesen DH, et al. Pharmacological management of obesity: an endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2015;100(2):342-362. doi:https://doi.org/10.1210/jc.2014-3415
Desalermos A, Russell B, Leggett C, et al. Effect of Obesogenic Medications on Weight-Loss Outcomes in a Behavioral Weight-Management Program. Obes Silver Spring Md. 2019;27(5):716-723. doi:https://doi.org/10.1002/oby.22444
Domecq JP, Prutsky G, Leppin A, et al. Clinical review: Drugs commonly associated with weight change: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2015;100(2):363-370. doi:https://doi.org/10.1210/jc.2014-3421
Leggett CB, Desalermos A, Brown SD, et al. The effects of provider-prescribed obesogenic drugs on post-laparoscopic sleeve gastrectomy outcomes: a retrospective cohort study. Int J Obes 2005. 2019;43(6):1154–1163. doi:https://doi.org/10.1038/s41366-018-0207-x
Verhaegen AA, Van Gaal LF. Drugs That Affect Body Weight, Body Fat Distribution, and Metabolism. [Updated 2019 Feb 11]. In: Feingold KR, Anawalt B, Boyce A, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537590/. Accessed 1 May 2023
Prescription Medications & Weight Gain. Obesity Action Coalition. 2013. Available from: https://www.obesityaction.org/resources/prescription-medications-weight-gain. Accessed 1 May 2023
Robins JM, Hernán MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiol Camb Mass. 2000;11(5):550-560. doi:https://doi.org/10.1097/00001648-200009000-00011
Yao W, Frydman H, Larocque D, Simonoff JS (2020). Ensemble Methods for Survival Data with Time-Varying Covariates. arXiv preprint arXiv:2006.00567 .
Hu L, Li F, Ji J, Joshi H, Scott E (2021). Joint marginal structural models to estimate the causal effects of multiple longitudinal treatments in continuous time with application to COVID-19. arXiv preprint arXiv:2109.13368 .
Cole SR, Hernán MA. Constructing inverse probability weights for marginal structural models. Am J Epidemiol. 2008;168(6):656-664. doi:https://doi.org/10.1093/aje/kwn164
Chan SH, Raffa SD. Examining the Dose-Response Relationship in the Veterans Health Administration’s MOVE!® Weight Management Program: A Nationwide Observational Study. J Gen Intern Med. 2017;32(Suppl 1):18-23. doi:https://doi.org/10.1007/s11606-017-3992-3
Grabarczyk TR. Observational Comparative Effectiveness of Pharmaceutical Treatments for Obesity within the Veterans Health Administration. Pharmacother J Hum Pharmacol Drug Ther. 2018;38(1):19-28. doi:https://doi.org/10.1002/phar.2048
Khera R, Murad MH, Chandar AK, et al. Association of Pharmacological Treatments for Obesity With Weight Loss and Adverse Events: A Systematic Review and Meta-analysis. JAMA. 2016;315(22):2424-2434. doi:https://doi.org/10.1001/jama.2016.7602
VA/DoD Clinical Practice Guideline for the Management of Adult Overweight and Obesity, Version 3.0 (2020). Available from: https://www.healthquality.va.gov/guidelines/CD/obesity/VADoDObesityCPGFinal5087242020.pdf. Accessed 1 May 2023
Del Re AC, Frayne SM, Harris AHS. Antiobesity medication use across the veterans health administration: patient-level predictors of receipt. Obes Silver Spring Md. 2014;22(9):1968-1972. doi:https://doi.org/10.1002/oby.20810
Fujioka K, Harris SR. Barriers and Solutions for Prescribing Obesity Pharmacotherapy. Endocrinol Metab Clin North Am. 2020;49(2):303-314. doi:https://doi.org/10.1016/j.ecl.2020.02.007
Acknowledgements
We thank Natalie Bontrager for editorial support (e.g., creating the patient flow chart). Support for VA/CMS data was provided by the Department of Veterans Affairs, VA Health Services Research and Development Service, VA Information Resource Center (Project Numbers SDR 02-237 and 98-004). The weight-change analysis was conducted in “AWS VA Enterprise Cloud Prospect” enclave and we would like to thank Dr. Siamack Ayandeh for the creation of the analytics study mart environment and the VHA Office of the Research and Development for funding of the Cloud Credits.
Funding
This research was funded by the IIR 18–019 (MLM, EW), AH was supported by a Career Development Award (IK2 HX003359), DB was supported by a Career Development Award (IK2 HX003085) and MLM was supported by a Senior Research Career Scientist award (RCS 10–391), all from VA HSR&D. Additional support by the Center of Innovation to Accelerate Discovery and Practice Transformation (CIN 13–410) at the Durham VA Health Care System is acknowledged.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest:
MLM reports research grants from NIH and VA HSR&D and ownership of Amgen stock due to his spouse’s employment. VAS reports research grants from NIH and VA HSR&D. AH reports research grants from NIH, VA HSR&D, AstraZeneca, and Abbott. All other authors declare no conflicts of interest.
Role of the Sponsor
The Health Services Research and Development Service, Department of Veterans Affairs had no role in the design, conduct, collection, management, analysis, or interpretation of the data; or in the preparation, review, or approval of the manuscript. The opinions expressed are those of the authors and not necessarily those of the Department of Veterans Affairs, the United States Government, Duke University, or the University of Washington.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hung, A., Wong, E.S., Dennis, P.A. et al. Real World Use of Anti-Obesity Medications and Weight Change in Veterans. J GEN INTERN MED 39, 519–528 (2024). https://doi.org/10.1007/s11606-023-08501-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-023-08501-z