Abstract
Background
High-need, high-cost Medicare patients can have difficulties accessing office-based primary care. Home-based primary care (HBPC) can reduce access barriers and allow a clinician to obtain valuable information not obtained during office visit, possibly leading to reductions in hospital use.
Objective
To determine whether HBPC for high-need, high-cost patients reduces hospitalizations and Medicare inpatient expenditures.
Design
We conducted a matched retrospective cohort study using a difference-in-differences analysis to examine patients 2 years before and 2 years after their first home visit (HBPC group).
Participants
The study included high-need, high-cost fee-for-service Medicare patients without prior HBPC use, of which 55,303 were new HBPC recipients and 156,142 were matched comparison patients.
Intervention
Receipt of at least two HBPC visits and, within 6 months of the index HBPC visit, a majority of a patient’s primary care visits in the home.
Main Measures
Total and potentially avoidable hospitalizations and Medicare inpatient expenditures.
Key Results
HBPC reduced total hospitalization rates, but the marginal effects were not statistically significant: a reduction of 11 total hospitalizations per 1000 patients in the first year (− 0.6%, p = 0.19) and 14 in the second year (− 0.7%, p = 0.16). However, HBPC reduced potentially avoidable hospitalization rates in the second year. The estimated marginal effect was a reduction of 6 potentially avoidable hospitalizations per 1000 patients in the first year (− 1.6%, p = 0.16) and 11 in the second (− 3.1%, p = 0.01). The estimated effect of HBPC was a small decrease in inpatient expenditures of $24 per patient per month (− 1.1%, p = 0.10) in the first year and $0 (0.0%, p = 0.99) in the second.
Conclusions
After high-need, high-cost patients started receiving HBPC, they did not experience fewer total hospitalizations or lower inpatient spending but may have had lower rates of potentially avoidable hospitalizations after 2 years.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
The rate of hospitalizations for high-need, high-cost patients—those with multiple chronic conditions and at least one functional limitation—is five times as high as the rate for the overall adult population and more than three times as high as the rate for those with multiple chronic conditions but no functional limitations.1 Medicare patients in the top decile of total spending account for almost 80% of all inpatient Medicare spending, about 10% of which is potentially preventable.2 Many high-need, high-cost patients may not receive timely primary care because traveling to an office presents substantial physical demands and, in some cases, a financial burden.
Clinicians can provide evaluation and management (E&M) services at home to any patient enrolled in the fee-for-service (FFS) Medicare program. As of 2023, reimbursement for E&M visits at home was lower than in an office, yet some clinicians may be motivated to offer home-based primary care (HBPC) to reduce access barriers for high-need, high-cost patients. HBPC allows a clinician to see a patient’s home environment, which may provide advantages such as opportunities to mitigate risks of falls and improve how medications are stored and organized. Furthermore, HBPC may encourage the development of a trusting relationship and effective communication among the patient, any caregiver, and the clinician.3,4,5 For these reasons, HBPC may reduce hospital utilization, avoiding potential negative consequences of hospitalization that can lead to permanent loss of function and nursing home entry.6,7 Yet HBPC is uncommon; in 2017, only 7.4% of homebound Medicare FFS patients received at least two home visits within 6 months.8 According to a survey of high-need, high-cost Medicare FFS patients who received HBPC in 2015 or 2016, patients tend to begin HBPC based on the recommendation of their doctor, home health agency, or social worker.9
Previous research focusing on high-need, high-cost patients has found that HBPC reduces hospitalizations in specialized care delivery models.3,10 These studies have typically focused on well-defined models of team-based HBPC offered by clinicians who provide only (or mostly) home visits and assume the role of primary care provider, such as those provided by the Department of Veterans Affairs or some academic medical centers. However, many clinicians who offer home visits do not do so for the majority of their time. In 2013, about 80 percent of clinicians who offered any home visits to FFS Medicare patients averaged fewer than 10 home visits per week.11
Given that many HBPC visits are provided by clinicians who do not specialize in HBPC, it is not known whether HBPC delivered by any clinician to high-need, high-cost patients reduces hospitalizations and inpatient expenditures. The objective of this study is to determine whether high-cost, high-need FFS Medicare patients who received HBPC had fewer hospitalizations and less inpatient Medicare expenditures than those who did not receive HBPC.
METHODS
Study Design
We designed a retrospective, intent-to-treat cohort study of FFS Medicare patients who received HBPC, comparing changes in their outcomes against a matched group that did not receive HBPC. Patients remained in the HBPC (or comparison) group for the entire post-intervention period, even if they switched modes of care; patients dropped out of the sample if they died or exited FFS Medicare.
This study was conducted using research-identifiable Medicare enrollment, claims, and assessment files (Appendix Table 1) as part of an independent evaluation for the Centers for Medicare and Medicare Services (CMS). It was exempt from Institutional Review Board review under 45 CFR 46.101(b).
Setting
We included patients who resided in a ZIP code where at least two FFS Medicare patients received HBPC in 2016. For HBPC recipients, we refer to the date of the first HBPC visit in 2017 as the index date (Fig. 1).
This figure shows the sample selection criteria applied before and after the index date to identify HBPC recipients and comparison patients and the two post-intervention years during which we measured outcomes. Notes: see the Appendixfor more information about sample selection criteria. Abbreviations: ADL, activities of daily living; FFS, fee-for-service; HBPC, home-based primary care.
We observed patients for 24 months before and up to 24 months after their index date. For example, for a HBPC recipient whose index date was in August 2017, the two pre-intervention years would be August 2015 to July 2017, while August 2017 to July 2019 were the two post-intervention years. We used a 24-month post-intervention period to provide adequate time for HBPC to affect outcomes yet reduce attenuation bias that may increase over time as more recipients stop receiving HBPC and some comparison patients begin HBPC. We estimated effects separately for each post-intervention year since the effectiveness of HBPC may change over time.
Patients and Study Size
We retained high-need, high-cost patients according to the HBPC patient eligibility criteria from CMS’ Independence at Home Demonstration. Patients needed to meet the following as of the index date: enrollment in FFS Medicare; two or more chronic conditions; two or more activities of daily living requiring assistance from another person as measured by assessment data; not in hospice or institutional long-term care; and hospitalization or observation stay and rehabilitation services within the prior 12 months.
To create a HBPC group, we identified eligible patients for whom HBPC was the dominant mode of primary care for at least 6 months following their index date. Patients were eligible for the HBPC group if they met the following criteria: (1) continuous enrollment in FFS Medicare and no home visits from a primary care clinician or specialist physician throughout the 2 years before their index date and (2) were alive at least 1 day and continuously enrolled in FFS Medicare during the 6-month period following the index date, and (3) received at least two HBPC visits during the 6-month period following the index date, where the majority of E&M visits from primary care clinicians must have taken place at home. HBPC visits were defined as E&M visits from a primary care clinician in a private home or domiciliary. After the initial 6-month period, patients were observed until exiting FFS Medicare, dying, or after 18 additional months.
Patients in the comparison group were identified using the same criteria, except they must have had no HBPC visits and at least one office-based E&M visit from a primary care provider during the 6-month period starting with their simulated index date. Given the likely endogeneity of entry into HBPC (sicker patients enter HBPC and have more hospitalizations and spending), it is essential that selected comparison patients be at a point in their health trajectory similar to the HBPC patients when they began HBPC. To align these trajectories, we created a series of simulated index dates for patients in the comparison group: we included each month in which a patient met the eligibility criteria to create a different version in the potential comparison pool. A potential comparison patient could have up to 12 versions, each with a different index date used to better match with a HBPC patient.
Since utilization and expenditure patterns vary across geographic areas, we matched each HBPC recipient to potential comparison patients who resided in the same Public Use Microdata Area. We used propensity score matching to ensure that the comparison group and HBPC recipients had similar demographic characteristics, functional status, and health status. We defined all matching variables for potential comparison patients relative to each simulated index date in the potential comparison pool so that variables like the HCC score would reflect the patient’s characteristics at each simulated index date. In the Appendix, we explain the sample identification and matching approach in detail.
Outcomes
The primary outcomes were total hospitalizations, potentially avoidable hospitalizations, and Medicare inpatient expenditures. Potentially avoidable hospitalizations occur when ambulatory care may have avoided or reduced the need for hospitalization. We based our measure on the Agency for Healthcare Research and Quality’s Prevention Quality Indicator 90, which includes diabetes, hypertension, heart failure, dehydration, bacterial pneumonia, and urinary tract infection. Inpatient expenditures include spending for hospitals and rehabilitation facilities. For detailed definitions, see the Appendix.
Statistical Methods
We used a difference-in-differences analysis. We measured outcomes in each of the 2 years following the index date, comparing the change over time for the HBPC group with the change for the comparison group. The effect reflects the difference between (1) the change in outcomes for patients after starting HBPC for the first time and (2) the change in outcomes of patients in the matched comparison group who did not receive HBPC over the same time period. Because the health status and expenditures of our sample changed considerably during the year before the index date from the health shock of hospitalization and rehabilitation, our baseline was limited to the year before the index date. However, we examined whether the HBPC and comparison groups had parallel trends over the two pre-intervention years.
We used linear regression for inpatient expenditures and zero-inflated negative binomial regressions for the hospitalization outcomes. The regressions controlled for variables we used for matching plus area-level fixed effects and standard errors clustered at the patient level. Because our outcome variables were monthly averages and annualized counts and patients could drop out of the sample due to death or exiting FFS Medicare, we used weights for the number of months we observed each patient in each post-intervention year.
We performed all statistical analyses with Stata (version 17.1) and considered a p value < 0.10 from two-tailed tests to be statistically significant.
RESULTS
Patients Included in the Study Sample
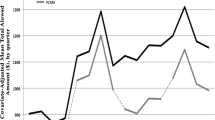
After applying the eligibility criteria described above, the study included 55,303 HBPC recipients. We identified 7,640,481 potential comparison patient versions, of whom 156,142 were selected as matched comparison patients. In the year before the index date, the HBPC and comparison groups had similar characteristics (Table 1 and Appendix Table 2) and similar levels of outcomes (Table 2). In addition, the two groups did not have a statistically significant differential change in any of the outcomes between the 2 years before the index date (Appendix Table 4). Because of the health shock the sample experienced in the year before the index date, hospitalizations and inpatient expenditures peaked in that year and declined in the two post-intervention years (Fig. 2).
This figure shows the total hospitalization and potentially avoidable hospitalization rates and Medicare inpatient expenditures for HBPC recipients and comparison patients 2 years before the index date and 2 years after the index date. The estimates are regression-adjusted to control for differences between the HBPC and comparison groups in the year prior to the index date. Source: Medicare claims and enrollment data for 2015 through 2019. Abbreviation: HBPC, home-based primary care.
Of the HBPC recipients who remained alive and in FFS Medicare 6 months following the index date, 63% continued to receive HBPC and did not enter hospice or die during months 7 to 12. By the last 6 months of the 24-month post-intervention period, 53% continued to receive HBPC and did not enter hospice or die during this period (Appendix Table 3). Only 3% of the comparison group received HBPC in months 7 to 12, which increased slightly in months 13 through 18 (5%) and months 19 through 24 (6%).
Estimates for Hospitalizations
In the year before the index date, HBPC recipients had a mean of 1921 total hospitalizations per 1000 patients per year and comparison patients had a mean of 1991 total hospitalizations per 1000 patients per year (Table 3). According to our difference-in-differences models, HBPC reduced total hospitalizations in both years, but the effects were not statistically significant. Specifically, in the first year, HBPC recipients had a mean of 1094 total hospitalizations per 1000 patients per year and comparison patients had a mean of 1176 total hospitalizations per 1000 patients per year. The estimated effect of HBPC was a reduction of 11 total hospitalizations per 1000 patients per year in the first year (− 0.6%, p = 0.19), which reflects the difference between the change over time for HBPC recipients (a reduction of 827 total hospitalizations) and for comparison patients (a reduction of 815 total hospitalizations). The observed decline in hospitalizations in the comparison group suggests that comparison patients had experienced similarly acute health events in the baseline period from which they began to recover in the follow-up period, bolstering our confidence in the match. In the second year, HBPC recipients had a mean of 982 total hospitalizations per 1000 patients per year and comparison patients had a mean of 1067 total hospitalizations per 1000 patients per year. The estimated effect of HBPC was a reduction of 14 total hospitalizations per 1000 patients per year in the second year (− 0.7%, p = 0.16).
However, HBPC reduced potentially avoidable hospitalizations in the second year after starting HBPC. In the year before the index date, HBPC recipients had a mean of 362 potentially avoidable hospitalizations per 1000 patients and comparison patients had a mean of 366 potentially avoidable hospitalizations per 1000 patients per year. Potentially avoidable hospitalizations declined to 234 and 208 potentially avoidable hospitalizations per 1000 patients per year among HBPC recipients in the first and second years, respectively, and to 244 and 224 per 1000 patients per year among comparison patients. The estimated effect of HBPC was a reduction of 6 potentially avoidable hospitalizations per 1000 patients per year in the first year (− 1.6%, p = 0.16) and 11 in the second year (− 3.1%, p = 0.01).
Estimates for Medicare Inpatient Expenditures
Average inpatient expenditures per patient per month among HBPC recipients were $2052 in the year before the index date, $1098 in the first year, and $1008 in the second year. Among comparison patients, they were $2118 in the year before the index date, $1189 in the first year, and $1073 in the second year. We found little evidence that HBPC reduced Medicare inpatient expenditures. The estimated effect of HBPC was a small decrease in Medicare inpatient expenditures per patient per month of $24 (− 1.1%, p = 0.10) in the first year and $0 (0.0%, p = 0.99) in the second year.
DISCUSSION
This analysis provides evidence about the extent to which HBPC affects hospitalizations and inpatient expenditures for high-need, high-cost Medicare patients—the group for whom HBPC might best be able to reduce hospitalizations and inpatient expenditures. All patients had multiple chronic conditions, hospitalization, and rehabilitation services in the prior 12 months and needed assistance from another person with multiple activities of daily living. HBPC did not reduce total hospitalizations or inpatient expenditures among this group of chronically ill, functionally impaired patients; however, there was some evidence that HBPC reduced potentially avoidable hospitalizations in the second year after starting HBPC.
In this study, HBPC was associated with reductions in potentially avoidable hospitalizations over time, suggesting that the setting in which a high-need, high-cost patient receives ambulatory care may affect some inpatient utilization and that the impacts of HBPC may be lagged or take time to accrue. For example, developing a trusting relationship and effective communication through HBPC can allow providers to become aware of acute issues and chronic condition exacerbations and address them early. However, this relationship and communication take time to develop. Unlike findings from other published studies,3 the estimated reduction in potentially avoidable hospitalizations in this study was fairly small (3.1% in the second year), and we did not find evidence that HBPC reduced total hospitalizations.
One factor that could have contributed to the difference in findings is that many previous studies used a pre-post-intervention group design or post-period intervention-comparison group design, whereas our study used a stronger design that compared changes in outcomes for HBPC and comparison patients. One published randomized clinical trial of a specialized HBPC program that used similar patient eligibility criteria found that HBPC led to a reduction in total hospitalizations but was ended early due to a higher death rate among HBPC recipients.12
A second factor that could have contributed to the difference in findings is differences in the delivery model of HBPC. Most of the existing literature focuses on a comprehensive, well-defined model of HBPC offering longitudinal care from an interdisciplinary team with 24/7 access to a primary care clinician.3 However, our study includes all HBPC providers and their FFS Medicare patients in the USA, including the thousands of clinicians for whom home visits do not account for most of the clinical care they provide and capturing the substantial variation in structure and care delivery approaches of practices that specialize in HBPC.4,11,12
This study has three main limitations. First, because the study design is quasi-experimental, we cannot assert a causal relationship between HBPC and hospitalizations. Unmeasured factors could affect a patient’s decision to begin HBPC and outcomes, and changes in those unmeasured factors or their relationship to outcomes could cause confounding. A randomized clinical trial that includes clinicians who specialize in HBPC and those who offer HBPC much less often would be the ideal study design. Second, although using an intent-to-treat study design reduces the risk of selection bias by following the same patients after they started receiving HBPC, it could have biased results toward zero since some patients stopped receiving HBPC. However, only a small share (15%) of the HBPC group remained alive and in FFS in month 7 and had zero HBPC visits between months 7 and 24. Therefore, it is unlikely that patients switching from HBPC to office-based care would have driven the results. Also, few patients in the comparison group began receiving HBPC. Finally, the HBPC group had to remain alive from the index date until the second HBPC visit, while the comparison group did not; however, the comparison group had to remain alive for up to 6 months until having an office-based primary care visit.
This study shows that, for high-need, high-cost FFS Medicare patients, HBPC reduced potentially avoidable hospitalizations by a small amount after 2 years but not total hospitalizations or Medicare inpatient expenditures. Given the limited supply of clinicians who offer HBPC13 and likely increases in the demand for HBPC because older adults are more likely to become homebound than to enter institutional long-term care,14 researchers ought to examine which characteristics of the HBPC delivery model are most likely to lead to improved outcomes. Additional research could examine whether the effects of HBPC differ based on characteristics of the HBPC delivery model, such as whether the provider offers only or mostly HBPC, rather than office visits. For example, clinicians who specialize in HBPC may more effectively identify unmet needs and build relationships in the home environment than those who provide HBPC less frequently, which could have implications for how HBPC is structured and reimbursed. Since home visits for FFS Medicare patients are more common and growing faster in assisted living facilities than in private residences,15 future research could compare the effectiveness of HBPC in these two settings.
Data Availability
The data sets used to create the analysis file for the current study are available through a data use agreement with the Centers for Medicare & Medicaid Services.
References
Hayes SL, Salzberg CA, McCarthy D, et al. High-need, high-cost patients: who are they and how do they use health care? 2016. Available at: https://www.commonwealthfund.org/publications/issue-briefs/2016/aug/high-need-high-cost-patients-who-are-they-and-how-do-they-use. Accessed 9 June 2023.
Joynt KE, Gawande AA, Orav J, Jha AK. Contribution of preventable acute care spending to total spending for high-cost medicare patients. JAMA. 2013;309:2572–78.
Zimbroff RM, Ornstein KA, Sheehan OC. 2021. Home-based primary care: a systematic review of the literature, 2010-2020. J Am Geriatr Soc. 2021;69:2963–72.
Leff B, Weston CM, Garrigues S, et al. Home-based primary care practices in the United States: current state and quality improvement approaches. J Am Geriatr Soc. 2015;63:963–69.
Hulen M, Laliberte A, Ono S, Saha S, Edwards ST. “Eyes in the home”: addressing social complexity in Veterans Affairs home-based primary care. J Gen Int Med. 2021;36:894–900.
Creditor MC. Hazards of hospitalization of the elderly. Ann Intern Med. 1993;118:161–240.
Covinsky KE, Palmer, RM, Fortinsky RH, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age. J Am Geriatr Soc. 2003;51:451–58.
Reckrey, JM, Yang M, Kinosian B, et al. Receipt of home-based medical care among older beneficiaries enrolled in Fee-for-Service Medicare. Health Aff. 2020;39:1289-96.
Kimmey, L, Anderson, M, Cheh V, et al. “Evaluation of the Independence at Home Demonstration: an examination of the first four years.” Washington, DC: Mathematica. 2019. Available at https://innovation.cms.gov/initiatives/independence-at-home/. Accessed 9 June 2023.
Federman, AD, Brody A, Ritchie CS, et al. Outcomes of home-based primary care for homebound older adults: a randomized clinical trial. J Am Geriatr Soc. 2023;71:334–454.
Yao N, Rose K, LeBaron V, Camacho F, Boling P. Increasing role of nurse practitioners in house call programs. J Am Geriatr Soc. 2017;65:847–2.
Klein S, Hostetter M, McCarthy D. An overview of home-based primary care: learning from the field. 2017. Available at: https://www.commonwealthfund.org/publications/issue-briefs/2017/jun/overview-home-based-primary-care-learning-field. Accessed 5 October 2022.
Yao N, Mutter JB, Berry JD, Yamanaka T, Mohess DT, Cornwell T. In traditional Medicare, modest growth in the home care workforce largely driven by nurse practitioners. Health Aff. 2021:40;478–86.
Ornstein KA, Garrido MM, Bollens-Lund E, et al. Estimation of the incident homebound population in the US among older Medicare beneficiaries, 2012 to 2018. JAMA Intern Med. 2020;180:1022–25.
Liu B, Ritchie CS, Ankuda CK, et al. Growth of fee-for-service Medicare home-based medical care within private residences and domiciliary care settings in the U.S., 2012–2019. J Am Med Dir Assoc. 2020;23:1614–20.
Acknowledgements:
The authors acknowledge the significant contributions to a predecessor of this study that were provided by the following former Mathematica employees: Valerie Cheh and Catherine McLaughlin.
Funding
This study was funded by the Centers for Medicare & Medicaid Services under contract number HHSM-500–2014-00034I/HHSM-500-T0018. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the Department of Health and Human Services or any of its agencies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest:
The authors declare that they do not have a conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information:
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kimmey, L., Wysocki, A., Forrow, L.V. et al. Effects of Home-Based Primary Care on Hospital Use for High-Need Medicare Patients: an Observational Study. J GEN INTERN MED 39, 19–26 (2024). https://doi.org/10.1007/s11606-023-08328-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-023-08328-8