Abstract
Background
Clinical trials indicate continuous glucose monitor (CGM) use may benefit adults with type 2 diabetes, but CGM rates and correlates in real-world care settings are unknown.
Objective
We sought to ascertain prevalence and correlates of CGM use and to examine rates of new CGM prescriptions across clinic types and medication regimens.
Design
Retrospective cohort using electronic health records in a large academic medical center in the Southeastern US.
Participants
Adults with type 2 diabetes and a primary care or endocrinology visit during 2021.
Main Measures
Age, gender, race, ethnicity, insurance, clinic type, insulin regimen, hemoglobin A1c values, CGM prescriptions, and prescribing clinic type.
Key Results
Among 30,585 adults with type 2 diabetes, 13% had used a CGM. CGM users were younger and more had private health insurance (p < .05) as compared to non-users; 72% of CGM users had an intensive insulin regimen, but 12% were not taking insulin. CGM users had higher hemoglobin A1c values (both most recent and most proximal to the first CGM prescription) than non-users. CGM users were more likely to receive endocrinology care than non-users, but 23% had only primary care visits in 2021. For each month in 2021, a mean of 90.5 (SD 12.5) people started using CGM. From 2020 to 2021, monthly rates of CGM prescriptions to new users grew 36% overall, but 125% in primary care. Most starting CGM in endocrinology had an intensive insulin regimen (82% vs. 49% starting in primary care), whereas 28% starting CGM in primary care were not using insulin (vs. 5% in endocrinology).
Conclusion
CGM uptake for type 2 diabetes is increasing rapidly, with most growth in primary care. These trends present opportunities for healthcare system adaptations to support CGM use and related workflows in primary care to support growth in uptake.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
Diabetes persists as a major healthcare issue in the United States and worldwide with increasing incidence, management cost, and societal impact.1,2 Diabetes is associated with decreased lifespan and accounts for 1 in every 4 US healthcare dollars.1 Costs are expected to increase as incidence and prevalence continue to rise.1,3 About 1 in 10 Americans have diabetes and approximately 90–95% have type 2 diabetes.4 Despite improvements in medications used to treat diabetes, data from 1999 to 2018 show fewer people with type 2 diabetes meeting glycemic or blood pressure targets over time.5 The most recent data indicate fewer than half are meeting these targets.5 Furthermore, diabetes is associated with a lower quality of life and the prevalence of elevated diabetes-related distress is estimated at 36%.6
A continuous glucose monitor (CGM) is a wearable medical device that measures real-time glucose levels in subcutaneous interstitial fluid. A CGM can provide data on glucose values that can be viewed easily, tracked over time, and virtually monitored to promote behavior change, avoid hyperglycemia and hypoglycemia, and inform dosing for prandial insulin.7,8,9 CGM is already an established standard of care for type 1 diabetes10,11 and is used by approximately 40–50% of people with type 1 diabetes.12 For people with type 2 diabetes, several recent studies indicate CGM use can aid with lowering hemoglobin A1c, improving quality of life, and maintaining longer time in range.7,8,13,14,15,16,17,18,19 Recent randomized controlled trials on CGM efficacy in type 2 diabetes have expanded our understanding of who might benefit to include people in primary care settings and with less intensive medication regimens.16,17,18 Accumulating evidence supporting CGM use in type 2 diabetes has driven calls to revise insurance policies and care standards to improve access and outcomes.13 Alongside the conduct of trials to determine the benefits of using a CGM in type 2 diabetes—and for whom and in what care settings—a confluence of factors have increased the uptake of CGM among people with type 2 diabetes, including CGM accessibility, improved CGM technology, availability of remote support for CGM use from commercial companies, and healthcare provider awareness of benefits.8,20 However, there are no studies on the rates of CGM uptake and use among people with type 2 diabetes in real-world care settings.
Most persons with type 2 diabetes receive care for their diabetes through primary care15,21,22 rather than endocrinology clinics, where CGM support and expertise have historically been housed. Barriers to CGM adoption noted in the literature include the lack of widespread adoption of CGM prescription in primary care compared to endocrinology practices.15,21,23 Lack of access to endocrinologists due to distance and cost along with an overwhelming tendency for primary care management of type 2 diabetes highlights a need to enhance and support CGM uptake in primary care.13,15 Therefore, we sought to characterize CGM users versus non-users and elucidate rates and trends in rates of new CGM prescriptions among adults with type 2 diabetes in a large academic medical center in the Southeastern US.
METHODS
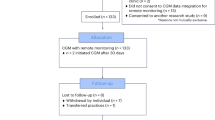
This study was approved by the Vanderbilt University Institutional Review Board (IRB #220962). We used a retrospective cohort observational design. First, we identified a cohort of adults with type 2 diabetes who received outpatient diabetes care at Vanderbilt University Medical Center (VUMC), a large academic medical center in middle Tennessee, during the 2021 calendar year (Jan. 1 to Dec. 31, 2021). All data were extracted using SQL queries from the Epic Clarity database, a data warehouse that is updated nightly from the Epic electronic health record (EHR). The cohort includes adults (age ≥ 18) diagnosed with type 2 diabetes (i.e., E11.* ICD-10 code as an active problem or visit diagnosis) with at least one visit to a primary care or endocrinology clinic in 2021. For the identified cohort, we extracted data regarding type of clinic visits in 2021 (primary care and/or endocrinology clinic visits) and recent demographic and clinical characteristics, including age, gender, race, ethnicity, health insurance type, insulin regimen (none, basal, prandial, or both), and most recent hemoglobin A1c (HbA1c) value as a measure of glycemic management. Next, we retrospectively extracted data on CGM prescriptions to ascertain if cohort members had ever been prescribed a CGM, the date of the first CGM prescription in our system, if the first CGM prescription in our system reflected a new or historical prescription, and the HbA1c value closest to and preceding the date of first CGM prescription. We excluded any HbA1c values over 7 months prior to the date of first CGM prescription.
Analyses
All analyses were conducted using Stata v. 14.2. We used descriptive statistics to characterize the cohort, including the proportion of CGM users (new and historical). We used Wilcoxon rank sum Kruskal–Wallis nonparametric tests of difference to compare cohort members who never had a CGM prescription (no CGM use) with those who had a CGM prescription (CGM use). Next, we sought to characterize the rate of CGM uptake for this cohort. For these analyses, we restricted the sample to new prescriptions (i.e., excluding patients who had used CGM prior to their first prescription within VUMC using the historical medication flag in Epic) and any cohort members who started CGM after 2021. Then we used graphics and summary statistics to describe the rate of new CGM users in our healthcare system. For this examination, we included the clinic type associated with the first CGM prescription and examined insulin regimen across prescribing clinic types.
RESULTS
Correlates of CGM Use
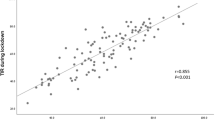
A total of 30,585 adults were seen by primary care or endocrinology for type 2 diabetes from January 1 to December 31, 2021; 12.7% (n = 3893) had CGM use indicated in their EHR (Table 1). CGM use was associated with younger age (users were around 6 years younger than non-users) and having private insurance, an insulin regimen including both basal and prandial insulin (including pre-mixed insulins), and higher HbA1c (Table 1). CGM users had higher most recent HbA1c values, with 32.0% having an HbA1c ≥ 8.5% as compared to 14.8% for non-users. CGM use was not associated with gender, race, or Hispanic ethnicity.
CGM use was also associated with having endocrinology visits in 2021 (vs. primary care only; Table 1). Most CGM users (76.8%) had endocrinology visits as part of their care in 2021, compared to 30.6% of non-users. However, 23.2% of CGM users only had primary care visits in 2021. The majority of CGM users were on an intensive insulin regimen, involving both basal and prandial insulin (72.1%). In our system, approximately 1 in every 4 (23.0%) people with type 2 diabetes who were prescribed prandial insulin (alone or with basal) were using a CGM. However, 12.3% of CGM users were not taking insulin (as compared to 54.0% of non-users).
We then stratified the cohort by type of clinic visits in 2021 (Table 2). Approximately 60% of the cohort had only primary care visits, 20% had only endocrinology visits, and 20% had both. Compared to persons with an endocrinology visit, fewer persons with only primary care visits had private insurance, fewer had an intensive insulin regimen, and more were not using insulin. Five percent of persons seen only in primary care were CGM users, compared with 23.1% with only endocrinology visits and 25.3% with both visit types.
Rates of CGM Uptake, Overall and by Prescribing Clinic
To examine the rate of CGM uptake for the 2021 cohort, we excluded patients who entered our system already using a CGM (i.e., historical users, n = 447) and patients who started CGM after 2021 (n = 282). This resulted in n = 3164 incident (new) CGM users with type 2 diabetes in the cohort. The earliest CGM prescription for the cohort appeared in December 2017. Our results show increasing uptake over time: only n = 1 in 2017, n = 487 in 2018, n = 791 in 2019, n = 799 in 2020, and n = 1086 in 2021 (Fig. 1). The average monthly rate of new CGM prescriptions was 40.6 (SD = 22.8) in 2018, 65.9 (SD = 7.9) in 2019, 66.6 (SD = 16.9) in 2020, and 90.5 (SD = 12.5) in 2021. As seen in Fig. 1, growth may have slowed from 2019 to 2020 due to the COVID-19 pandemic limiting outpatient visits in 2020. Endocrinology was the source of the first CGM prescription for 66.8% of cohort members compared to 27.6% from primary care and 5.6% from other specialties (most commonly cardiology, transplant, and infectious disease). However, despite evidence of an initial lag in CGM prescribing for type 2 diabetes in primary care compared to endocrinology, rates of primary care prescribing made up an increasingly larger proportion of incident users each year (Fig. 1). Primary care more than doubled its average monthly CGM prescriptions to new users in 2021 from the prior year (16.9 per month in 2020 and 38.0 per month in 2021). In contrast, endocrinology’s average monthly prescriptions to new users dropped in 2020 and 2021 (50.6 per month in 2019; 45.3 in 2020; 47.4 in 2021). Figure 2 depicts the percentage of prescriptions for CGM to new users by clinic type and insulin regimen, revealing most (82.2%) people who started CGM in endocrinology used both basal and prandial insulin, whereas nearly 30% of people who start CGM in primary care were not using insulin and approximately half were using both basal and prandial insulin.
DISCUSSION
People with type 2 diabetes may benefit from CGM by gaining a personalized approach to glycemic management with numerous opportunities for feedback, which can lead to lowered diabetes-related healthcare costs and mitigate some diabetes distress.24 In a large academic medical center in the Southeastern US, we found that around 13% of people receiving outpatient care for type 2 diabetes had used a CGM, and nearly 1 in 4 who were prescribed prandial insulin had used a CGM. From 2020 to 2021, the overall growth rate of new CGM users was 36% overall, which was composed of 5% growth rate in endocrinology and 125% growth rate in primary care. New CGM prescriptions among people not taking insulin were more common in primary care than in endocrinology (28% vs. 5%), suggesting that primary care prescribing practices are responding to calls for increased CGM use among adults with type 2 diabetes including those not using insulin.8,13 Despite rapid growth in new CGM prescriptions from primary care, 3 of 4 CGM users had an endocrinology clinic visit in 2021 suggesting primary care providers may prescribe CGM with a subsequent referral to endocrinology (rather than referrals to endocrinology resulting in a new CGM prescription from an endocrinology clinic).
We did not find evidence of CGM use disparities by gender, race, nor ethnicity, but we did find CGM users were younger and more had private insurance as compared to non-users. Age differences could be due to an increased likelihood for younger patients to adopt new technology,25,26 and may dissipate over time as medical specialties shift to managing type 2 diabetes for generations of people who were exposed to technology earlier. We also found CGM users had a more intensive insulin regimen and higher HbA1c. The patient-level factors driving uptake of CGM in type 2 diabetes appear to be a need for additional diabetes management tools (younger age combined with more intensive regimen and higher HbA1c) and accessibility/affordability (private insurance coverage). We are aware of only one other study reporting characteristics of CGM users as compared to non-users among adults with type 2 diabetes. Karter et al.16 conducted a retrospective cohort study among adults with both type 1 and type 2 diabetes in a Northern California–integrated health care delivery system. From 2015 to 2018, less than 1% (344 of 36,080) of adults with type 2 diabetes used CGM. Like our findings, Karter et al. noted that CGM users were younger and found evidence of socioeconomic disparities. However, HbA1c was lower for CGM users than non-users. Our finding that people with type 2 diabetes who initiate CGM have higher HbA1c values may reflect increasing knowledge of the benefits of CGM for HbA1c reduction among physicians and patients, potentially because of the research reporting efficacy of CGM for improving glycemic management.
We did not examine physician- or clinic-level factors driving CGM uptakes; however, there were no system-level efforts to increase CGM prescribing, and our primary care clinics are geographically diverse with local leadership, suggesting this increase is mostly due to patient inquiries about CGM and individual providers using CGM in their clinical practice. Our findings indicate primary care providers may prescribe CGM with a concurrent/subsequent referral to endocrinology for data interpretation and/or medication changes. Vanderbilt also has a Population Health Clinical Pharmacy team that supports patients in procurement of CGM, provides patient education on CGM, and can recommend medication adjustments in communication with prescribing providers. These services are initiated by a prescription for CGM. The availability of these services coincided with increases in CGM prescribing in 2021. Primary care physicians may have prescribed CGM more readily knowing clinical pharmacy and endocrinology referrals were available.
Although our health system is not typical of all primary care settings in important ways and may not reflect widespread practice at present, our findings may be an early indicator of trends as patients and healthcare providers learn about the benefits of CGM and the affordability, design and accuracy of CGM improves. We may see rapid growth in CGM uptake among adults with type 2 diabetes, mirroring the growth seen in type 1 diabetes—from 12% in 2014 to 38% in 2018.27 Our findings in the context of the existing literature indicate the following efforts could support growth in CGM use among adults with type 2 diabetes: (a) expanded government insurance coverage for CGM and decreased costs of devices to support uptake among persons without private insurance coverage, (b) increased awareness among primary care providers of CGM benefits for persons with type 2 diabetes regardless of medication regimen, and/or (c) supportive services in partnership with primary care settings where most persons with type 2 diabetes receive their care. There are several potential models to support CGM use in primary care.13 For instance, primary care clinics could follow models used in clinical trials on CGM efficacy to partner with endocrinology and/or clinical pharmacists via telehealth17 and/or mobile health programs.19 This may be particularly helpful for persons on intensive insulin regimens, who may benefit from iterative medication adjustments based on CGM data viewed remotely. For persons not on intensive insulin regimens, CGM may be used for the purposes of supporting lifestyle changes and/or avoiding fingerstick methods.28 CGM initiation could be paired with evidence-based lifestyle interventions—delivered as an adjunct to clinical care and reimbursed by insurance—to maximize benefit.14,18 The presence of these supportive partnerships may enable primary care providers to increase CGM prescribing in type 2 diabetes. Research on models to support CGM uptake in primary care settings is needed.14
Limitations of our study include reliance on data from a single academic medical center that serves insured patients and lower percentages of people from minoritized racial and ethnic groups, limiting generalizability and our ability to detect disparities. Like many academic medical centers, our population may have more advanced diabetes than national populations as indicated by the higher percentage of people using insulin (51% at VUMC as compared to 36% nationally as of 2019). Many primary care settings do not have easy access/integration with endocrinology, which may make the identified trends less generalizable to all primary care settings. Primary care physicians may be more willing to start patients with CGM if endocrinology and/or clinical pharmacist support is available as needed. Furthermore, because we used data collected as part of regular care, we were not able to examine who sustains CGM use nor reasons for use/non-use, which are important areas to examine in type 2 diabetes given the rapid increase in uptake documented here. Finally, we were unable to reliably determine which CGM users were also using an insulin pump with EHR data.
This study is the first to examine trends in CGM uptake among adults with type 2 diabetes in real-world care settings, and findings reveal rapid increases driven by CGM prescribing in primary care. More persons not using insulin were prescribed CGM in primary care than in endocrinology. People who were younger, with private insurance coverage and higher HbA1c values, were more likely to use CGM. Primary care may drive growth in CGM use among persons with type 2 diabetes with appropriate supports in place for patients to procure CGM, understand CGM data, and make appropriate behavioral or medication changes in response to CGM data.
Data Availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
American Diabetes Association. Economic costs of diabetes in the U.S. in 2017. Diabetes Care. 2018;41(5):917-28. https://doi.org/10.2337/dci18-0007. PubMed PMID: 29567642; PubMed Central PMCID: PMC5911784.
Lin X, Xu Y, Pan X, Xu J, Ding Y, Sun X, et al. Global, regional, and national burden and trend of diabetes in 195 countries and territories: an analysis from 1990 to 2025. Sci Rep. 2020;10(1):14790. https://doi.org/10.1038/s41598-020-71908-9. PubMed PMID: 32901098; PubMed Central PMCID: PMC7478957.
Chen L, Islam RM, Wang J, Hird TR, Pavkov ME, Gregg EW, et al. A systematic review of trends in all-cause mortality among people with diabetes. Diabetologia. 2020;63(9):1718-35. Epub 20200706. https://doi.org/10.1007/s00125-020-05199-0. PubMed PMID: 32632526.
Center for Disease Control and Prevention. Type 2 Diabetes 2021. Available from: https://www.cdc.gov/diabetes/basics/type2.html. Accessed 26 Sept 2022
Fang M, Wang D, Coresh J, Selvin E. Trends in diabetes treatment and control in US adults, 1999–2018. N Engl J Med. 2021;384(23):2219-28.
Perrin N, Davies M, Robertson N, Snoek F, Khunti K. The prevalence of diabetes‐specific emotional distress in people with type 2 diabetes: a systematic review and meta‐analysis. Diabet Med. 2017;34(11):1508-20.
Beck RW, Riddlesworth TD, Ruedy K, Ahmann A, Haller S, Kruger D, et al. Continuous glucose monitoring versus usual care in patients with type 2 diabetes receiving multiple daily insulin injections: a randomized trial. Ann Intern Med. 2017;167(6):365-74. https://doi.org/10.7326/M16-2855. PubMed PMID: 28828487.
Kompala T, Neinstein A. A new era: increasing continuous glucose monitoring use in type 2 diabetes. Am J Manag Care. 2019;25(4 Spec No.):Sp123-sp6. PubMed PMID: 30933461.
Chamberlain JJ, Doyle-Delgado K, Peterson L, Skolnik N. Diabetes technology: review of the 2019 American Diabetes Association Standards of Medical Care in Diabetes. Ann Intern Med. 2019;171(6):415-20. https://doi.org/10.7326/M19-1638. PubMed PMID: 31404925.
Peters AL, Ahmann AJ, Battelino T, Evert A, Hirsch IB, Murad MH, et al. Diabetes technology—continuous subcutaneous insulin infusion therapy and continuous glucose monitoring in adults: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2016;101(11):3922-37.
American Diabetes Association. 7. Diabetes technology: standards of medical care in diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S71-S80.
DeSalvo DJ, Noor N, Xie C, Corathers SD, Majidi S, McDonough RJ, et al. Patient demographics and clinical outcomes among type 1 diabetes patients using continuous glucose monitors: data from T1D Exchange Real-World Observational Study. J Diabet Sci Technol. 2021;0(0):19322968211049783. https://doi.org/10.1177/19322968211049783. PubMed PMID: 34632823.
Peek ME, Thomas CC. Broadening access to continuous glucose monitoring for patients with type 2 diabetes. JAMA. 2021;325(22):2255-7. https://doi.org/10.1001/jama.2021.6208. PubMed PMID: 34077505; PubMed Central PMCID: PMC8649865.
Oser TK, Litchman ML, Allen NA, Kwan BM, Fisher L, Jortberg BT, et al. Personal continuous glucose monitoring use among adults with type 2 diabetes: clinical efficacy and economic impacts. Curr Diab Rep. 2021;21(11):49. https://doi.org/10.1007/s11892-021-01408-1. PubMed PMID: 34882273; PubMed Central PMCID: PMC8655087.
Warman M, Filippi M, Manning B, Oser T, Nease D, Hall T, et al. Continuous glucose monitoring for primary care patients with diabetes: barriers, facilitators, & resources to support access. Ann Fam Med. 2022;20(Supplement 1):2689. https://doi.org/10.1370/afm.20.s1.2689.
Karter AJ, Parker MM, Moffet HH, Gilliam LK, Dlott R. Association of real-time continuous glucose monitoring with glycemic control and acute metabolic events among patients with insulin-treated diabetes. JAMA. 2021;325(22):2273-84. https://doi.org/10.1001/jama.2021.6530. PubMed PMID: 34077502; PubMed Central PMCID: PMC8173463.
Martens T, Beck RW, Bailey R, Ruedy KJ, Calhoun P, Peters AL, et al. Effect of continuous glucose monitoring on glycemic control in patients with type 2 diabetes treated with basal insulin: a randomized clinical trial. JAMA. 2021;325(22):2262-72. https://doi.org/10.1001/jama.2021.7444. PubMed PMID: 34077499; PubMed Central PMCID: PMC8173473.
Cox DJ, Banton T, Moncrief M, Conaway M, Diamond A, McCall AL. Minimizing glucose excursions (GEM) with continuous glucose monitoring in type 2 diabetes: a randomized clinical trial. J Endocr Soc. 2020;4(11):bvaa118. https://doi.org/10.1210/jendso/bvaa118. PubMed PMID: 33094208; PubMed Central PMCID: PMC7566397.
Bergenstal RM, Layne JE, Zisser H, Gabbay RA, Barleen NA, Lee AA, et al. Remote application and use of real-time continuous glucose monitoring by adults with type 2 diabetes in a virtual diabetes clinic. Diabetes Technol Ther. 2021;23(2):128-32. https://doi.org/10.1089/dia.2020.0396. PubMed PMID: 33026839; PubMed Central PMCID: PMC7868574.
Kravarusic J, Aleppo G. Diabetes technology use in adults with type 1 and type 2 diabetes. Endocrinol Metab Clin North Am. 2020;49(1):37-55. https://doi.org/10.1016/j.ecl.2019.10.006. PubMed PMID: 31980120.
Isaacs DB, Natalie. Diabetes dialogue: optimizing CGM uptake in primary care, 2022. HCP Live Network. Accessible here: https://www.hcplive.com/view/diabetes-dialogue-optimizing-cgm-uptake-in-primary-care. Accessed 26 Sept 2022.
Shrivastav M, Gibson W, Jr., Shrivastav R, Elzea K, Khambatta C, Sonawane R, et al. Type 2 diabetes management in primary care: the role of retrospective, professional continuous glucose monitoring. Diabetes Spectr. 2018;31(3):279-87. https://doi.org/10.2337/ds17-0024. PubMed PMID: 30140145; PubMed Central PMCID: PMC6092883.
Oser T, Hall T, Warman MK, Filippi MK, Manning B, Callen E, et al. 651-P: Continuous glucose monitoring in primary care: explaining characteristics associated with CGM prescription. Diabetes. 2022;71(Supplement_1). https://doi.org/10.2337/db22-651-P.
Laiteerapong N, Cooper JM, Skandari MR, Clarke PM, Winn AN, Naylor RN, et al. Individualized glycemic control for U.S. adults with type 2 diabetes: a cost-effectiveness analysis. Ann Intern Med. 2018;168(3):170-8. https://doi.org/10.7326/M17-0537. PubMed PMID: 29230472; PubMed Central PMCID: PMC5989575.
Eiland L, Thangavelu T, Drincic A. Has technology improved diabetes management in relation to age, gender, and ethnicity? Curr Diab Rep. 2019;19(11):111. https://doi.org/10.1007/s11892-019-1231-5. PubMed PMID: 31686221.
Mahajan S, Lu Y, Spatz ES, Nasir K, Krumholz HM. Trends and predictors of use of digital health technology in the United States. Am J Med. 2021;134(1):129-34. Epub 20200724. https://doi.org/10.1016/j.amjmed.2020.06.033. PubMed PMID: 32717188.
Foster NC, Beck RW, Miller KM, Clements MA, Rickels MR, DiMeglio LA, et al. State of type 1 diabetes management and outcomes from the T1D Exchange in 2016–2018. Diabet Technol Ther. 2019;21(2):66-72.
Edelman SV, Argento NB, Pettus J, Hirsch IB. Clinical implications of real-time and intermittently scanned continuous glucose monitoring. Diabetes Care. 2018;41(11):2265-74.
Funding
This study was supported by the Center for Health Behavior and Health Education at Vanderbilt University Medical Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Author Mayberry has served as a consultant for Cecelia Health, Inc. and has research support from the National Institute of Diabetes and Digestive and Kidney Diseases and Helmsley Charitable Trust for intervention development and evaluation in diabetes.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mayberry, L.S., Guy, C., Hendrickson, C.D. et al. Rates and Correlates of Uptake of Continuous Glucose Monitors Among Adults with Type 2 Diabetes in Primary Care and Endocrinology Settings. J GEN INTERN MED 38, 2546–2552 (2023). https://doi.org/10.1007/s11606-023-08222-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-023-08222-3