Abstract
The problem of unaffordable prescription medications in the United States is complex and can result in poor patient adherence to therapy, worse clinical outcomes, and high costs to the healthcare system. While providers are aware of the financial burden of healthcare for patients, there is a lack of actionable price transparency at the point of prescribing. Real-time prescription benefit (RTPB) tools are new electronic clinical decision support tools that retrieve patient- and medication-specific out-of-pocket cost information and display it to clinicians at the point of prescribing. The rise in US healthcare costs has been a major driver for efforts to increase medication price transparency, and mandates from the Centers for Medicare & Medicaid Services for Medicare Part D sponsors to adopt RTPB tools may spur integration of such tools into electronic health records. Although multiple factors affect the implementation of RTPB tools, there is limited evidence on outcomes. Further research will be needed to understand the impact of RTPB tools on end results such as prescribing behavior, out-of-pocket medication costs for patients, and adherence to pharmacologic treatment. We review the terminology and concepts essential in understanding the landscape of RTPB tools, implementation considerations, barriers to adoption, and directions for future research that will be important to patients, prescribers, health systems, and insurers.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
BACKGROUND
The rise in healthcare costs in the United States (US) has been a major driver for efforts to increase price transparency in medical care. This narrative review aims to describe the issues related to the high cost of prescription medications, discuss the evidence for electronic clinical decision support in providing cost information to prescribers, and contextualize the role of real-time prescription benefit (RTPB) tools in the current healthcare landscape in the US.
Unaffordable prescription medications are associated with many detrimental downstream effects, including poor adherence to therapy, worse patient outcomes, and high healthcare system costs.1–4 While prescription medications account for nearly 17% of US healthcare expenditures, one-fifth of Americans report the inability to fill prescriptions, and one-third report that prescription medication costs pose a significant financial burden.5 Out-of-pocket (OOP) costs, or the amount that a patient is responsible for at the time of purchase, are a function of prescription drug coverage, deductible (amount patients pay for health services before their insurance plan starts to pay), co-payments (fixed costs paid for health services after paying the deductible), and co-insurance (the percent of costs paid for health services after paying the deductible).6 Medications with high OOP costs are more likely to be abandoned at the pharmacy, and restrictive medication coverage may lead to decreased medication utilization.7–10 Overall, the cost of medication nonadherence to the healthcare system is estimated to be between $100 and $289 billion annually.10
Retail outpatient medication prices in the US are determined by a complex cost-sharing relationship between manufacturers, wholesalers, health insurance plans, pharmacy benefit managers (PBMs), and pharmacy retailers.11, 12 While manufacturers set medication list prices, PBMs leverage their market share to negotiate rebates with pharmaceutical manufacturers on behalf of health plans.11, 12 In exchange, PBMs place specific medications on tiered formularies with the stated intention of passing the savings from rebates to insurers, employers, and patients.11, 13 However, due to a lack of transparency surrounding the negotiation process, the rebate size is rarely disclosed publicly and PBMs can retain a significant portion of the rebate as profit.11–14 There are also indications that manufacturer rebates are not as significant as claimed, that rebate size is associated with increased OOP cost, and that savings are not ultimately passed on to patients.5, 13, 14 Findings suggest that higher rebates are associated with increased list prices and that individuals without insurance are disproportionately affected by higher OOP costs.14 The rise in high-deductible health plans has also contributed to increases in deductibles, premiums, and co-insurance.5 Ultimately, this complexity manifests at the point of sale, where the medication and its coverage tier, the PBM arrangements, the patient’s plan, and the deductible position make costs difficult to predict.
Although clinicians are aware of the burden of prescription costs and willing to consider treatment options based on patient affordability, a major barrier to engaging in effective conversations about medication costs with patients has been the lack of price transparency at the point of prescribing.5, 15, 16 Studies have shown that even with some information about patients’ health plans, clinicians have great difficulty accurately estimating OOP medication costs.17, 18 Although formulary decision support (FDS) with e-prescribing provides clinicians with information regarding formulary tier, they lack details on the OOP costs of medications.19–24 Contacting pharmacies or insurance plans directly is often the only way prescribers can access prescription cost or coverage restrictions information, a time-consuming task that busy clinicians often cannot accomplish within the confines of a brief office visit. The current electronically available OOP price information is piecemeal; patient-specific medication coverage data exists among PBMs, insurers, or pharmacy systems while patient-agnostic pharmacy price comparison data is available through consumer-facing services such as GoodRx.15 But, these disparate data could be consolidated, in line with the American College of Physicians recommendations to increase the availability of “accurate, understandable, and actionable information on the price of prescription medication” at the point of prescribing to promote shared decision-making and cost-conscious care.11
There has been increasing evidence that FDS with information on cost, formulary tier, or medication substitutions during e-prescribing can lead to changes in prescribing behavior and cost reduction.19, 20 In a 2019 study, prescriber alerts for several high-cost medication classes provided medication substitutions and resulted in a 32% decrease in the prescribing volume of those classes in ambulatory practices.21 In the inpatient setting, both institution-specific and commercial formulary decision support improved formulary adherence in select medication classes.22, 23 Regarding cost savings, a study done within a single health system with 45,000 health plan members found that medication substitution alerts for just four medication classes resulted in an annual savings of more than $800,000 for the health plan.24 Another study of two insurers showed that e-prescribing with formulary support increased tier 1 prescribing and estimated savings of $845,000 per 100,000 patients.16, 25
Studies on the impact of FDS on medication adherence are mixed. In a propensity score–matched study of prescribers using e-prescribing with FDS versus those using paper prescriptions, there was increased medication adherence to initial fill and 30- and 90-day refills in those using FDS.26 However, in another study evaluating the effect of prescribing preferred tier medications on patient OOP medication costs, the change in prescribing behavior with formulary support only modestly reduced co-payments and was not associated with increased medication adherence.27
THE ROLE OF REAL-TIME PRESCRIPTION BENEFITS
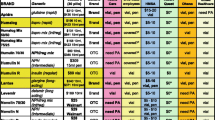
RTPB tools are new electronic clinical decision support tools that retrieve patient- and medication-specific information from the PBM, payors, or retail pharmacy, and display it to clinicians at the point of prescribing. A step beyond the medication tier information available with traditional FDS, RTPB tools display information on the OOP cost of a medication, coverage restrictions, and the cost of medication substitutions. This information would normally only be seen by pharmacists when submitting a claim, so RTPB tools add new value by displaying it to the clinician during the prescribing workflow. In line with efforts to increase price transparency, the Centers for Medicare & Medicaid Services (CMS) mandated that Medicare Part D plan sponsors (employers or insurance plans that provide Part D prescription drug coverage) adopt RTPB tools that are capable of integrating with at least one prescriber’s e-prescribing system or electronic health record (EHR) by January 1, 2021.28, 29 Despite this mandate, RTPB tools have not been uniformly adopted at the level of health systems and practices, and while they have the potential to improve cost-informed prescribing, they are not well utilized or understood. To date, there is only a report in the gray literature30 and two published studies on the impact of RTPB tools.31, 32 The first was a retrospective cohort study conducted at a single health system which compared the fill rates between prescriptions whose orders triggered RTPB activation vs those that did not trigger RTPB activation. Orders that did not trigger RTPB activation were for patients whose prescription drug plans were not compatible with the RTPB tool or who had no verified prescription drug plan. RTPB activation was associated with a higher prescription fill rate (79.8% vs 71.7%) and lower cancelation rate (9.34% vs 14.89%).31 The second study was a cluster-randomized trial at practices in an urban academic health system that showed an adjusted 11.2% OOP cost reduction for medications with RTPB recommendations. However, only a small percentage of medications (4.2%) had recommendations for medication substitutions.32 This narrative review aims to introduce important concepts related to RTPB tools (Table 1.), examine the factors that influence their adoption and impact, and discuss their limitations and implications for clinical practice and future research.
RTPB tools serve as intermediaries in the flow of prescription medication information between EHRs and PBMs. These instruments perform the following functions: (1) determine the patient’s eligibility for prescription medication coverage; (2) check medication tier and potential coverage restrictions such as prior authorization; (3) obtain patient OOP cost for the prescribed quantity and at the selected pharmacy; (4) recommend alternative medications and/or pharmacies with lower OOP costs; and (5) display this information electronically to the prescriber at the point of prescribing and/or to patients on an after-visit summary. RTPB tools are offered as either standalone products by RTPB vendors or add-on products of e-prescribing vendors.
HOW DO RTPB TOOLS WORK?
For clinicians to trust the accuracy of the information provided by RTPB tools and to understand the limitations of these tools, it is important for them to understand how they work. To obtain prescription medication information at the point of prescribing, RTPB tools complete a sequence of electronic messages called “RTPB transactions” (Fig. 1). In the predominant type of transaction, the EHR sends a request for prescription benefit information to the RTPB vendor, which forwards the message to the patient’s PBM. The PBM determines eligibility by cross-referencing enrollment data from the EHR with the PBM’s insurance and prescription coverage information. If the patient has medication coverage through the PBM, it returns prescription benefits information (specific to that patient) to the RTPB vendor, which forwards the information to the EHR where it can be reviewed in real time by a clinician. For an RTPB transaction to occur, the patient’s insurance and pharmacy benefit information must be documented and transmitted in the correct EHR fields for each electronic message. Although user interfaces may differ by EHR vendor, the prescription benefit estimates generally show information on OOP costs, coverage restrictions, and lower cost options based on days’ supply, pharmacy practice setting, and medication substitutions. RTPB tools are designed to return the true patient-facing OOP cost. However, since they do not submit an actual claim to the PBM, there remains the rare possibility of error. While most RTPB vendors retrieve information directly from PBMs, there are vendors that have direct connections with payors or pharmacies to obtain RTPB information. An example of the information that may be displayed by an RTPB to the prescriber is shown in Figure 2. Ideally, this information presents an opportunity for prescribers and patients to discuss OOP medication cost at the point of prescribing.
For a health system that adopts RTPB tools, prescribers will be able to access prescription benefit information for only a proportion of their patients. RTPB patient coverage, or the percent of patients for whom RTPB information is available, is determined by a set of relationships between different stakeholders illustrated in Figure 3. Health systems may contract with one or more RTPB vendors, each of which has contractual relationships with different PBMs. Figure 3 illustrates a hypothetical example in which the health system is contracted with two RTPB vendors which can obtain prescription benefit information from PBMs, including the OOP cost estimates based on the medication price, patient’s copay, and deductible. These contractual relationships determine the RTPB patient coverage for the subset of the insured patients seen in the health system. In the figure, RTPB vendor 1 is contracted with and is able to obtain RTPB information for the patients covered by PBM 1 and PBM 2. The health system can obtain additional RTPB patient coverage through RTPB vendor 2, which is contracted to PBMs 3–5. However, health systems also provide care for patients who do not have RTPB coverage, such as those whose PBMs do not have a relationship with an RTPB vendor or uninsured patients. This gap in RTPB coverage is illustrated in Figure 3 by patients covered by PBM 6 or who do not have prescription medication coverage.
RTPB patient coverage: relationship between EHR vendors, RTPB vendors, and PBMs. A hypothetical health system’s RTPB patient coverage, or the percent of patients for whom RTPB information is available, is illustrated by the patient groups outlined in black who are covered by PBMs that have relationships with the health system’s RTPB vendors. The gaps in patient coverage are highlighted by patients in gray, which include patients whose PBM does not have a relationship with the health system’s RTPB vendor (solid outline) and patients who do not have insurance (hashed outline).
In addition to the stakeholder relationships that determine whether RTPB information is available for individual patients, institutional implementation decisions will influence prescribers’ interactions with RTPB information. Implementation decisions include whether RTPB alerts display automatically or if clinicians must “opt-in” by clicking a button to retrieve an estimate during e-prescribing. Institutions may also present RTPB information as passive decision support tools that display information without interrupting workflow versus an interruptive alert. It is important to note that for most prior studies examining alert type, alerts were designed to either display automatically or as interruptive alerts. This distinction may be pertinent, as Pevnick et al. found no difference in prescribing behavior for preferred tier medications with only non-interruptive formulary support alerts.27 Health systems can suppress RTPB alerts based on thresholds for the cost difference between the substitutions and the original prescription or allow their providers to “opt-out” of seeing RTPB information when prescribing medications. These institutional implementation decisions can influence the amount and content of prescription benefit information that prescribers interact with, and the degree of effort or clicks needed to navigate RTPB tools. As institutions adopt RTPB instruments, they would benefit from evidence on how different implementation choices affect the quality of the information retrieved and prescriber usability.
RESEARCH AGENDA
RTPB tools have the potential to provide timely prescription benefit information and decision support in choosing the most financially appropriate medication for patients. The need to control healthcare costs and efforts like the CMS mandate for the adoption of RTPB tools will likely spur greater implementation in the future. However, just because these tools exist does not necessarily mean that they are equally accessible in the care of all populations, utilized by clinicians, or have the intended clinical impact. For future research evaluating the impact of RTPB tools, we suggest careful consideration of the measured outcomes, focusing on key stakeholders such as patients, prescribers, health systems, and insurers.
Outcomes with RTPB Tools
Evidence on the effect of clinical decision support to promote medication price transparency is mostly limited to studies of FDS. Most studies focus on specific medication classes or outcomes related to formulary adherence or cost savings for health systems rather than patient-centered outcomes. With the adoption of RTPB tools, it will be essential to evaluate outcomes meaningful to patients and families such as OOP cost and determinants of adherence to prescribed medication therapy. It also opens the possibility of studying the effect of cost-effective prescribing on clinical outcomes, such as management of chronic diseases that require long-term medications. For example, outcomes that may impact clinical practice might include the effect of RTPB patient coverage and tool utilization in medication adherence in diabetes or heart failure, where cost is known to impact adherence.33, 34 Health equity is an additional area of concern. These tools are only available in the care of patients who are insured and have prescription medication coverage and may potentially widen disparities in healthcare delivery. It will be essential to assess RTPB patient coverage to identify systemic gaps and patients who cannot receive the benefits of RTPB tools in their care. Although RTPB tools will play an important role in increasing price transparency for a subset of insured patients, studying the gaps in RTPB coverage may also highlight the need to integrate other players with electronic drug pricing information such as the retail pharmacies and health technology companies that track, compare pricing, and offer discount coupons to patients.
Clinician Adoption
At face value, prescribers should embrace RTPB tools as relevant and timely information at an appropriate point in the clinical workflow. However, studies have shown that the availability of clinical decision support tools does not necessarily predict end-user adoption.35–38 Multiple factors may affect tool use, including clinician confidence in the accuracy of information, prescriber burden, and lack of training.39, 40 Prior studies have shown that while helpful, FDS is not always completely accurate,41 which may deter clinicians from trusting RTPB information and recommendations. As with any other information used in decision-making, prescribers should understand where the data is coming from and how these tools work, which is the motivation underlying this narrative review. For prescribers, RTPB tools currently offer a more accurate, granular, and real-time window into OOP costs for their insured patients than has previously existed. Starting January 1, 2023, the CMS Final Rule will require availability of RTPB comparison tools to patients for obtaining information on cost and alternative medications, which will empower patients to engage in discussions with prescribers around cost.42,43,44 RTPB tools have the potential to change the shared decision-making dynamic between prescribers and their patients by making conversations about medication costs possible. However, prescriber burden must also be considered, as meaningful use of RTPB tools necessitates shared decision-making with patients on the most medically appropriate and cost-effective medication options. Given the time constraints of clinical interactions, these important but potentially lengthy discussions may add further non-reimbursed burden during patient interactions.45 As clinicians are equipped with more information on the cost of treatments, additional training and tools will be necessary to improve the prescriber skills and the quality of communication in shared decision-making discussions around cost.46, 47 Prescriber education of RTPB tools will need to be multifaceted, from the fundamental knowledge of the prescription coverage data being provided to the practical application of the information in clinical settings.
As RTPB tools become more widely available, there will be ample opportunities, as well as challenges, for research on prescriber adoption patterns. Defining appropriate measures will be essential, and utilization of electronically captured metrics may aid in standardizing research. The prescription adjustment rate, or the percent of RTPB information displayed where a prescriber accepted a recommendation for an alternative, is measurable, but it is unclear what the optimal rate is to promote the best patient outcomes across a set of different disease conditions. Quantitative evaluation of added prescriber burden with RTPB tool utilization may be assessed by measuring clicks or time spent in navigating the tool or ordering medications, and must be weighed against the potential benefits of these tools. Evaluating prescribing patterns by different specialties may show whether some specialties such as primary care are disproportionately affected. Also, given that RTPB tools provide medication substitutions based on cost and do not account for the efficacy or side effects of therapeutic alternatives, medication efficacy and safety with RTPB tool recommendations should be evaluated. Qualitative research will also be needed to assess clinician’s and patients’ perceptions of these tools, how using the tools affect workflow, and how these tools impact curriculum on cost-effectiveness in medical education.
System-Level Outcomes and Pharmacoeconomics
As healthcare organizations implement RTPB tools, standard system-level metrics must be also developed to evaluate their performance in adoption and the impact of the tools. Although conceptually important, RTPB patient coverage may be difficult to measure as the patient population treated by the health system, or the denominator, often presents an attribution challenge. For a more easily measurable proxy, health systems could use the RTPB data retrieval rate, or the percent of prescription benefit inquiries retrieved divided by all electronic prescriptions, which can be obtained from EHR data. It will also be important to understand what types of recommendations are being made by RTPB tools, such as alternative recommendations for the actual medication, pharmacy, or days supply. There may be unintended economic consequences of the recommendation types; for example, if most of the recommendations are for less expensive pharmacy practice settings, RTPB tools could simply be steering prescription routing away from retail and toward PBM-owned mail-order pharmacies. Future studies should evaluate the impact of RTPB tools on prescription routing and potential downstream effects, such as reduction in pharmacy-level competition and potential consequences for decreased patient access. These types of consequences may be relevant as decisions regarding financing of these tools are made, and whether RTPB tools are paid for by health systems or PBMs. Regarding the issue of providers’ ability to opt out of alerts, and whether interruptive alerts achieve better adoption than non-interruptive alerts, researchers could leverage the difference in implementation patterns across institutions to evaluate the effect of these decisions. For example, it would be interesting to evaluate whether the option for provider opt-out would affect measures such as RTPB retrieval rate, or whether alert interruptiveness affects the prescription adjustment rate toward more cost-effective medications. As RTPB tools are adopted across the US, research using standard evaluation metrics will be important to better understand the impact of RTPB implementation patterns and to compare performance across health systems.
CONCLUSION
With the CMS mandate, US prescribers and health systems will likely see widespread integration of RTPB tools into EHRs in the future. This stands to radically alter the landscape of price transparency at the point of prescribing by providing timely information on medication coverage for insured patients with participating PBMs. Currently, RTPB tools are widely available as vendor products and mandated by CMS, yet poorly understood, heterogeneously implemented, and suboptimally adopted. While they hold the promise to lower prescription costs, the evidence for the costs and benefits of implementing these tools is unclear, and they do not cover all patients. More work is needed to optimize these tools, increase adoption, and monitor unintended consequences such as decreasing access to affordable retail medications or worsening disparities for uninsured patients. RTPB tools thus hold a promise for the future price transparency with careful guidance from the clinical community and better understanding of the impact of these tools on patient-, provider-, and system-related outcomes.
References
Iuga AO, McGuire MJ. Adherence and health care costs. Risk Manag Healthc Policy 2014;7:35–44.
Herkert D, Vijayakumar P, Luo J, Schwartz JI, Rabin TL, DeFilippo E, et al. Cost-related insulin underuse among patients with diabetes. JAMA Intern Med 2019;179(1):112–4.
Mojtabai R, Olfson M. Medication costs, adherence, and health outcomes among Medicare beneficiaries. Health Aff 2003;22(4):220–9.
Cutler RL, Fernandez-Llimos F, Frommer M, Benrimoj C, Garcia-Cardenas V. Economic impact of medication non-adherence by disease groups: a systematic review. BMJ Open 2018;8(1):e016982.
Mello MM. Barriers to ensuring access to affordable prescription drugs. Annu Rev Pharmacol Toxicol 2020;60:275–89.
HealthCare.gov, Glossary, n.d. URL: https://www.healthcare.gov/glossary/co-insurance/ (Accessed 10/19/2022)
Shrank WH, Choudhry NK, Fischer MA, Avorn J, Powell M, Schneeweiss S, et al. The epidemiology of prescriptions abandoned at the pharmacy. Ann Intern Med 2010;153(10):633–40.
Doshi JA, Li P, Huo H, Pettit AR, Armstrong KA. Association of patient out-of-pocket costs with prescription abandonment and delay in fills of novel oral anticancer agents. J Clin Oncol 2018;36(5):476–82.
Gleason PP, Starner CI, Gunderson BW, Schafer JA, Sarran HS. Association of prescription abandonment with cost share for high-cost specialty pharmacy medications. J Manag Care Pharm 2009;15(8):648–58.
Shenolikar R, Burch S, Gilmore A, Eaddy M PHP39 sensitivity of medication use and outcomes to formulary controls in the elderly: a review of the literature. Vol. 13, Value in Health 2010 p. A88. Available from: https://doi.org/10.1016/s1098-3015(10)72420-7
Daniel H, Bornstein SS, Health and Public Policy Committee of the American College of Physicians. Policy recommendations for pharmacy benefit managers to stem the escalating costs of prescription drugs: a position paper from the American College of Physicians. Ann Intern Med 2019;171(11):823–4.
Bai G, Sen AP, Anderson GF. Pharmacy benefit managers, brand-name drug prices, and patient cost sharing. Ann Intern Med 2018;168(6):436–7.
Shepherd J. Pharmacy benefit managers, rebates, and drug prices: conflicts of interest in the market for prescription drugs. Yale L & Pol’y Rev 2019;38:360.
Yeung K, Dusetzina SB, Basu A. Association of branded prescription drug rebate size and patient out-of-pocket costs in a nationally representative sample, 2007-2018. JAMA Netw Open 2021;4(6):e2113393.
Perez SL, Weissman A, Read S, Smith CD, Colello L, Peter D, et al. U.S. internists’ perspectives on discussing cost of care with patients: structured interviews and a survey. Ann Intern Med 2019;170(9_Suppl):S39–45.
Gorfinkel I, Lexchin J. We need to mandate drug cost transparency on electronic medical records. CMAJ. 2017;189(50):E1541–2.
Sloan CE, Millo L, Gutterman S, Ubel PA. Accuracy of physician estimates of out-of-pocket costs for medication filling. JAMA Netw Open 2021;4(11):e2133188.
Shrank WH, Fox SA, Kirk A, Ettner SL, Cantrell CH, Glassman P, et al. The effect of pharmacy benefit design on patient-physician communication about costs. J Gen Intern Med 2006;21(4):334–9.
McMullin ST, Lonergan TP, Rynearson CS, Doerr TD, Veregge PA, Scanlan ES. Impact of an evidence-based computerized decision support system on primary care prescription costs. Ann Fam Med 2004;2(5):494–8.
McMullin ST, Lonergan TP, Rynearson CS. Twelve-month drug cost savings related to use of an electronic prescribing system with integrated decision support in primary care. J Manag Care Pharm 2005;11(4):322–32.
Monsen CB, Liao JM, Gaster B, Flynn KJ, Payne TH. The effect of medication cost transparency alerts on prescriber behavior. J Am Med Inform Assoc 2019;26(10):920–7.
Helmons PJ, Coates CR, Kosterink JGW, Daniels CE. Decision support at the point of prescribing to increase formulary adherence. Vol. 72, Am J Health Syst Pharm. 2015. p. 408–13. Available from: https://doi.org/10.2146/ajhp140388
Teich JM, Merchia PR, Schmiz JL, Kuperman GJ, Spurr CD, Bates DW. Effects of computerized physician order entry on prescribing practices. Arch Intern Med 2000;160(18):2741–7.
Stenner SP, Chakravarthy R, Johnson KB, Miller WL, Olson J, Wickizer M, et al. ePrescribing: reducing costs through in-class therapeutic interchange. Appl Clin Inform 2016;7(4):1168–81.
Fischer MA, Vogeli C, Stedman M, Ferris T, Alan Brookhart M, Weissman JS. Effect of electronic prescribing with formulary decision support on medication use and cost. Vol. 168, Arch Intern Med. 2008. p. 2433. Available from: https://doi.org/10.1001/archinte.168.22.2433
Joseph SB, Sow M. E-prescribing with decision support is associated with improvements in medication adherence. Am J Pharm 2016;8(4):133–40.
Pevnick JM, Li N, Asch SM, Jackevicius CA, Bell DS. Effect of electronic prescribing with formulary decision support on medication tier, copayments, and adherence. BMC Med Inform Decis Mak 2014;14:79.
Centers for Medicare & Medicaid Services. Medicare advantage and part D drug pricing final rule (CMS-4180-F). Fact Sheet 2019. Available from: https://www.cms.gov/newsroom/fact-sheets/medicare-advantage-and-part-d-drug-pricing-final-rule-cms-4180-f
Everson J, Frisse ME, Dusetzina SB. Real-time benefit tools for drug prices. JAMA. 2019;322(24):2383–4.
Davison A, Merrey J. NCPDP Foundation RTPB grant: final report. Available from: https://ncpdpfoundation.org/pdf/NCPDPFoundationRTPBGrant_FinalReport.pdf
Bhardwaj S, Merrey JW, Bishop MA, Yeh HC, Epstein JA. Impact of real-time benefit tools on patients’ access to medications: a retrospective cohort study. Am J Med 2022:S0002-9343(22)00528-9. https://doi.org/10.1016/j.amjmed.2022.06.017
Desai SM, Chen AZ, Wang J, Chung WY, Stadelman J, Mahoney C, et al. Effects of real-time prescription benefit recommendations on patient out-of-pocket costs: a cluster randomized clinical trial. JAMA Intern Med. 2022 Available from: https://doi.org/10.1001/jamainternmed.2022.3946
Gourzoulidis G, Kourlaba G, Stafylas P, Giamouzis G, Parissis J, Maniadakis N. Association between copayment, medication adherence and outcomes in the management of patients with diabetes and heart failure. Vol. 121, Health Policy. 2017. p. 363–77. Available from: https://doi.org/10.1016/j.healthpol.2017.02.008
Thornton Snider J, Seabury S, Lopez J, McKenzie S, Goldman DP. Impact of type 2 diabetes medication cost sharing on patient outcomes and health plan costs. Am J Manag Care 2016;22(6):433–40.
Nanji KC, Slight SP, Seger DL, Cho I, Fiskio JM, Redden LM, et al. Overrides of medication-related clinical decision support alerts in outpatients. J Am Med Inform Assoc 2014;21(3):487–91.
Kawamoto K, McDonald CJ. Designing, conducting, and reporting clinical decision support studies: recommendations and call to action. Ann Intern Med 2020;172(11_Supplement):S101–9.
Greenes RA, Bates DW, Kawamoto K, Middleton B, Osheroff J, Shahar Y. Clinical decision support models and frameworks: Seeking to address research issues underlying implementation successes and failures. J Biomed Inform 2018;78:134–43.
Nanji KC, Seger DL, Slight SP, Amato MG, Beeler PE, Her QL, et al. Medication-related clinical decision support alert overrides in inpatients. J Am Med Inform Assoc 2018;25(5):476–81.
Sutton RT, Pincock D, Baumgart DC, Sadowski DC, Fedorak RN, Kroeker KI An overview of clinical decision support systems: benefits, risks, and strategies for success. Vol. 3, npj Digital Medicine. 2020 Available from: https://doi.org/10.1038/s41746-020-0221-y
Laka M, Milazzo A, Merlin T. Factors that impact the adoption of clinical decision support systems (CDSS) for antibiotic management Vol. 18, International Journal of Environmental Research and Public Health 2021. p. 1901. Available from: https://doi.org/10.3390/ijerph18041901
Andrus MR, Forrester JB, Germain KE, Eiland LS. Accuracy of pharmacy benefit manager medication formularies in an electronic health record system and the Epocrates mobile application. J Manag Care Spec Pharm 2015;21(4):281–6.
Centers for Medicare & Medicaid Services. Changes to medical advantage and part D will provide better coverage, more access and improved transparency for medicare beneficiaries. Press Release. 2021 Available from: https://www.cms.gov/newsroom/press-releases/changes-medicare-advantage-and-part-d-will-provide-better-coverage-more-access-and-improved
Viswanathan M, Golin CE, Jones CD, Ashok M, Blalock SJ, Wines RCM, et al. Interventions to improve adherence to self-administered medications for chronic diseases in the United States: a systematic review. Ann Intern Med 2012;157(11):785–95.
Feldman R, Feldman N, Seoane-Vazquez E. A patient price guide for prescription medication. Ann Intern Med 2022. Available from: https://doi.org/10.7326/M21-4755
Campbell EM, Sittig DF, Ash JS, Guappone KP, Dykstra RH. Types of unintended consequences related to computerized provider order entry. J Am Med Inform Assoc 2006;13(5):547–56.
Yahanda AT, Mozersky J. What’s the role of time in shared decision making? AMA J Ethics 2020;22(5):E416–22.
Elwyn G, Frosch DL, Kobrin S. Implementing shared decision-making: consider all the consequences. Implement Sci 2016;11:114.
Acknowledgements
The authors thank Dylan Fink and DJ Butala for providing research support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
FAW, JIS, BHC, NK and ES were supported by a Donaghue Foundation Greater Value Portfolio research grant relating to this work. JAE received grant funding for related work from the Pharmacy Quality Alliance and the National Pharmaceutical Council. JL is supported by grants from NIDDK, NIDA and The Leona M. and Harry B. Helmsley Charitable Trust, unrelated to this work.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wong, R., Mehta, T., Very, B. et al. Where Do Real-Time Prescription Benefit Tools Fit in the Landscape of High US Prescription Medication Costs? A Narrative Review. J GEN INTERN MED 38, 1038–1045 (2023). https://doi.org/10.1007/s11606-022-07945-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-022-07945-z