Abstract
Background
Secure text messaging systems (STMS) offer HIPAA-compliant text messaging and mobile phone call functionalities that are more efficient than traditional paging. Although some studies associate improved provider satisfaction and healthcare delivery with STMS use, healthcare organizations continue to struggle with achieving widespread and sustained STMS adoption.
Objective
To understand the barriers to adoption of an STMS among physicians and advanced practice providers (APPs).
Design
We qualitatively analyzed free-text comments that clinicians (physicians and APPs) across a large healthcare organization offered on a survey about STMS perceptions.
Participants
A total of 1110 clinicians who provided a free-text comment in response to one of four open-ended survey questions.
Approach
Data were analyzed using a grounded theory approach and constant comparative method to characterize responses and identify themes.
Key Results
The overall survey response rate was 20.5% (n = 1254). Clinicians familiar with the STMS frequently believed the STMS was unnecessary (existing tools worked well enough) and would overburden them with more communications. They were frustrated that the STMS app had to be downloaded onto their personal mobile device and that it drained their battery. Ambiguity regarding who was reachable in the app led to missed messages and drove distrust of the STMS. Clinicians saw the exclusion of other care team members (e.g., nurses) from the STMS as problematic; however, some clinicians at hospitals with expanded STMS access complained of excessive messages. Secondhand reports of several of these barriers prevented new users from downloading the app and contributed to ongoing low use.
Conclusions
Clinicians are reluctant to adopt an STMS that does not offer a clear and trustworthy communication benefit to offset its potential burden and intrusiveness. Our findings can be incorporated into STMS implementation strategies that maximize active users by targeting and mitigating barriers to adoption.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
For years, clinicians have used standard text messaging to coordinate patient-related care.1,2,3 Text messaging is bidirectional and asynchronous, giving clinicians the ability to respond to a message at a time of their choosing, without the disruption of a phone call. However, in 2016, the Joint Commission disallowed standard text messaging to convey patient information, citing the potential for privacy violations.4 Instead, it stipulated that healthcare organizations must use secure text messaging systems (STMS) with key features including a secure sign-on process, encrypted messaging, and delivery and read receipts.5 Demand for these compliant systems subsequently accelerated: there are now dozens of STMS vendors whose products range from simplistic texting apps to complex platforms with electronic health record integration.6
Beyond security advantages, several studies suggest that STMS may improve clinical communication and healthcare delivery as compared to traditional paging systems. Specifically, STMS use has been associated with a decrease in clinicians’ task completion time, improvement in clinicians’ perceived productivity,7 and improvement in clinicians’ ability to communicate thoughts more clearly and effectively.8 Other studies have associated STMS implementation with a shorter length of stay9 and a decrease in communication failure events.10 Conversely, concerns about STMS include text messaging as a form of alarm fatigue, misinterpretation of text messages, and text messaging inappropriately replacing critical verbal communication.11
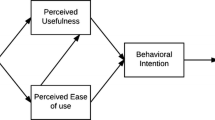
Despite potential benefits, healthcare organizations that have implemented STMS using a traditional, top-down approach (e.g., hospital-wide email communications, dissemination of information through program directors and department chairs) may struggle to achieve widespread and sustained STMS adoption.12 We observed a similar phenomenon within our own organization after the implementation of an STMS, the Vocera Collaboration Suite (Vocera Communications, Inc., San Jose, CA).13 To understand the barriers to STMS adoption (wherein adoption is defined as an individual’s decision to commit to full use of a new technology),14 we administered a survey to clinicians that explored perceptions of the STMS though both quantitative items and free-text prompts. The quantitative results, interpreted through the Technology Acceptance Model15 and reported elsewhere,13 revealed that clinicians who did not think their peers were using the STMS were less likely to adopt it.
However, model-based conclusions on health information technology adoption may overlook more complex socio-technical barriers.16,17 Qualitative methods can clarify the what of quantitative results by providing insight into the how and why—information that is crucial to planning and executing a successful implementation.18,19 In this study, we sought to complement our quantitative results with a qualitative analysis of the free-text responses to our survey. Our goal was to explore and describe barriers to STMS adoption within healthcare organizations.
METHODS
Setting, Study Design, Participants
This study took place at Northwestern Medicine (NM), a large healthcare organization in Illinois. NM implemented the STMS in early 2019, as described previously.13 System leaders announced the availability of the STMS during medical staff meetings and through several emails that encouraged clinicians (defined here as physicians and advanced practice providers [APPs]) to download the secure app onto their personal smartphones.
Clinicians who worked in one of six locations where the STMS had been implemented were eligible to complete our survey (n = 6142) and received an email invitation to participate approximately 8 months after go-live. The survey13 was administered between November and December 2019, with weekly reminders sent to non-respondents. Quantitative scale items explored clinicians’ perceptions and use of the STMS while qualitative items elicited barriers and concerns. We anticipated some clinicians had never downloaded the STMS or used it rarely; therefore, we created questions with branching logic based on level of use. The survey introduction, branching logic, and free-text prompts are depicted in Figure 1.
Analysis
Our research team included members with expertise in qualitative research (KC), communication technology (KO, TB), and internal medicine (KO, TB, PS). We followed standard methodological practices for the analysis and reporting of free-text comments in qualitative research,20,21,22,23 employing a grounded theory approach with constant comparison across cases to interpret responses.24,25 Individual comments were extracted from the survey data, deidentified, and analyzed using an iterative, inductive, team-based approach to coding (in lieu of a priori constructs).
Following initial codebook development (TB, KO, PS, KC), three coders (TB, KO, PS) iteratively coded the remaining comments, collectively modifying the codebook and clarifying definitions and relationships between codes. Each comment was independently coded by two coders; discrepancies were resolved via discussion.
All comments were coded—both code saturation (codebook is stable) and meaning saturation (understanding of issue with no additional insights arising) were met.26 The full team then reviewed the codes, codebook, and coding notes in collective discussion, identifying themes, subthemes, and representative quotations. Thematic coding was performed using Microsoft Excel (2016). This study was deemed not human research by the Northwestern University Institutional Review Board.
RESULTS
A total of 1254 clinicians completed the survey, representing a response rate of 20.5%. Of these, 1110 (88.5%) responded to at least one free-text prompt, resulting in a total of 1536 comments. Demographic characteristics of those who left at least one comment and those who did not are listed in Table 1. Of respondents who left a comment, 49 of 1110 (4.4%) used the STMS greater than once a week, while 884 of 1110 (79.6%) never or almost never used the STMS. We identified six themes that we present in Table 2 along with corresponding subthemes and representative quotations.
Lack of Familiarity with the STMS
Those who had never downloaded the app commonly reported a lack of awareness of the STMS. For many, our survey was the first time they had heard of the STMS. Some recalled seeing educational materials via email but admitted they were unsure of the purpose of the STMS and if it was relevant to their specific practice.
Perception of the STMS as Unnecessary and Burdensome
Many clinicians expressed that existing communication technologies already met their needs, including the traditional one-way paging system, standard text messaging, electronic health record messaging, and email. They questioned how adding the STMS to this milieu would offer additional benefit. Others stated that the plethora of communication technologies in use was already burdensome. Some speculated they would only use the STMS if it replaced one or more existing communication technologies. Clinicians further expressed displeasure at the idea of discursive group STMS messages frequently interrupting them without providing clinically relevant information.
Perception of the STMS as Intrusive
Concerns about the STMS affecting work-life balance were common. Because clinicians were expected to download the app onto their personal phones, many feared that after-hours messages would reach them and necessitate a response. Some preferred pagers and hospital-supplied shift phones because they could be forwarded to a colleague or physically left at work, while others expected financial reimbursement to use the STMS on their personal phone. Clinicians also voiced concerns that the STMS allowed other users to ignore or bypass professional communication boundaries (e.g., the attending was messaged directly through the STMS when the fellow should have been contacted first).
Severe Battery Drain Caused by the STMS App
Battery drain was the most common complaint about the STMS app. Clinicians were annoyed to discover that the app quickly drained their phone battery, with some describing a completely empty battery before the workday was over. The battery drain occurred even when the app was closed, which led many clinicians to delete it after downloading it. Secondhand reports of battery drain kept many clinicians from downloading and trying out the app themselves.
Low Usage by Others Contributed to and Reinforced Low Adoption
Clinicians cited a lack of other users as an enormous barrier to their use of the STMS. Many reported that few of their colleagues were using it, and therefore, they saw no reason to download the app. Those who had downloaded it commented that people who they wanted to contact had not downloaded the app and thus were unreachable.
Some clinicians working in hospitals where nurses did not have STMS access lamented the lack of other care team members on the platform. These clinicians wanted to be able to communicate with nurses, social workers, and therapists through the STMS, but none of these groups had been granted access. Many felt that the absence of an official policy from hospital leadership mandating use of the STMS across all clinical disciplines was further hindering adoption.
Lack of Trust in the STMS to Function as Needed
Clinicians had a hard time identifying which of their colleagues were logged in and available to receive messages in the STMS app. Several reported sending multiple messages but never receiving a response. Others noticed that their STMS accounts continued to receive silent messages even after logging out of or closing the app. Clinicians’ inability to confidently know whether they or their recipients would receive a message as intended eroded trust in the STMS to deliver important clinical care information in a timely fashion.
DISCUSSION
We identified six key themes manifesting as barriers to STMS adoption across a large healthcare organization. These themes include a lack of familiarity with the STMS, perceiving it as unnecessary and burdensome, perceiving it as an intrusion, battery drain, low usage by others, and a lack of trust in it to function as needed.
Undoubtedly, clinicians’ lack of knowledge of a technology or its purpose represents an existential threat to its adoption. We suspect that many clinicians lacked familiarity with the STMS because they had not attended or remembered presentations during medical staff meetings and/or they had not read or remembered the contents of educational materials emailed prior to go-live. There were STMS “champions” at the organizational and hospital level, but not at the departmental or division level, which likely perpetuated lack of STMS familiarity and allowed it to grow into a sizeable barrier to adoption.
The theme that the STMS was unnecessary and burdensome arose from clinicians believing that the STMS did not offer anything beyond what existing communication technologies could do. Their views align with the concept of relative advantage within Rogers’s Diffusion of Innovations, wherein a technology that appears better than existing technology has a greater likelihood of adoption.27 Although STMS promote HIPAA compliance through encryption and password protection, clinicians did not describe these features as advantageous, indicating a lack of perceived relative advantage as compared to existing communication technologies. Our findings are consistent with research demonstrating that clinicians continue to use unencrypted text messaging despite security concerns.28
Battery drain persistently stymied adoption. Even those who never downloaded the STMS had heard secondhand reports of the battery drain issue and anchored on this concern as the primary reason they had not downloaded the app. Their hesitation persisted even after a software patch to improve battery performance was released and publicized by the organization. While battery drain has been noted in other STMS,29 our findings highlight how secondhand reports of such technical issues can spread and persist even if the technical issue is eventually addressed.
A lack of other users on the platform was a tremendous barrier to STMS adoption. Communication technologies require many active users to function efficiently, but not everyone will start using a new communication platform at once. Critical mass theory suggests there is a critical mass of users that must adopt the new platform, allowing for ample communication partners, before everyone else does.30 Once others perceive that a critical mass of users exists, they are more likely to adopt themselves. Perceived critical mass has been shown to heavily influence communication technology adoption.31,32 In our quantitative analysis of these survey data, we found that perceived critical mass influenced STMS adoption even more than perceived usefulness.13 That is, clinicians are unlikely to use an STMS that no one around them seems to be using, even if the STMS seems useful.
We discovered that a lack of trust in the STMS to function as needed was inhibiting sustained adoption among users who had some experience using the app. Clinicians found they could not rely on the app to readily identify which of their colleagues were logged in and able to receive text messages, nor could they rely on the app to alert them in a timely manner to unread sent or received messages. Though the existing web-based paging system could only confirm message delivery, its ubiquity and familiarity seemed to impart more trust than the STMS app. Uncertainty around user availability and message receipt in the app could lead to unnoticed wrong-recipient communication errors, the same dangerous errors that have been shown to occur in traditional paging systems.33
Paradoxically, Hansen et al. showed a 59% reduction in communication failures after STMS implementation—their implementation included ongoing, targeted education and real time assistance.10 We suspect that many of the struggles reported by our clinicians could be resolved with clearer instructions on how to identify and reach active app users. These instructions could be integrated into the app directly by the vendor, delivered to clinicians during ongoing educational sessions, or both.
Beyond highlighting the need for ongoing STMS education, our findings suggest several other strategies for healthcare organizations to improve STMS adoption. To increase familiarity and relevance to the end user, healthcare organizations can initially target their STMS implementation efforts to specific departments that will benefit from a clear use case. For example, discharge planning between internal medicine clinicians and social workers is likely more efficient through STMS than through traditional paging and landline phones. Individuals in both departments stand to benefit from the increased STMS efficiency, and organizations should clearly and consistently make such benefits clear to users (e.g., through ongoing departmental email communications and in-person announcements during daily interdisciplinary rounds).12 The barrier of low usage by others should be lessened when social workers are granted access to and start using the STMS to communicate among themselves and with clinicians.
Widening the pool of potential STMS users is crucial to achieving a self-sustaining critical mass. Healthcare organizations can gain more potential users by giving STMS access to more care team members and by giving work smartphones to those who do not have or prefer not to use a personal smartphone. One study that reported a significant decrease in length of stay in the context of high STMS adoption gave STMS access (and smartphones) not only to physicians and APPs, but also to nurses, pharmacists, social workers, clinical resource coordinators, and unit secretaries.9 Organizations should realize that physicians and APPs use STMS primarily to message non-physician or non-APP members of the care team, most commonly nurses.34
As more healthcare professionals are given STMS access, the risk of excessive communication increases.10,35 Though a small increase in messages after STMS implementation is likely tolerable, our findings suggest that a marked increase in messages, especially those not deemed clinically important, will been seen as burdensome and could become a barrier to STMS adoption. Therefore, healthcare organizations should develop standardized communication policies (e.g., “FYI” or “STAT” text message templates to designate urgency, guidance around group messages, etc.) and continuously surveil the burden of messaging on all clinical roles across the system.11
LIMITATIONS
Our study has several limitations. Although free-text comments represent a valuable type of qualitative data,20,36 participants who choose to leave a comment may not be representative of all survey participants or the population at large. While we found similar demographic distributions between commenters and non-commenters among survey participants, nearly 80% of those invited did not participate in the survey. This response rate is similar on average to other large surveys of clinicians.1,37,38 Those who did not participate in the survey may have differed from the participants in their perceptions of the STMS, possibly leaving additional themes undiscovered.
Most of our participants did not use the STMS frequently. It is possible that greater representation from heavy users would reveal additional barriers that were not reported here. While we did not explicitly account for frequency of STMS use in this qualitative analysis, many comments included verbiage describing use patterns (e.g., “Used it a lot initially but difficult to find who is live on it and it seems not many are.” [1827, internal medicine]). When described, these use patterns were incorporated into coding and thematic analysis.
The use of four distinct prompts must also be considered. Prompts one through three were expansion prompts that focused participants’ attention on specific reasons why they had not adopted the STMS (Why not downloaded? Why not used more? Concerns?). Prompt four (Additional thoughts or comments?) was a general prompt in the classical open-ended format. We felt our research question would be most accurately answered by analyzing the three expansion prompts, in line with a purposive sampling strategy.21 Conceivably, including the general prompt in our analysis could bias our coding with comments unrelated to our research question.22 To reduce this potential bias, we explicitly noted if a comment was left in response to the general prompt during the coding process and cataloged but did not include themes that did not represent a barrier to STMS adoption. Readers should similarly understand that, while this research reports barriers, several clinicians responding to the general prompt described satisfaction with various aspect of the STMS. We did not report these positive comments because our prompts did not specifically ask clinicians to identify STMS benefits; therefore, these comments were unlikely to be representative of the general population. Identifying additional benefits and facilitators of STMS adoption will be an important area for future research.
CONCLUSION
Clinicians identified several reasons why they were resistant to adopting the STMS. The largest barriers to adoption arose from a lack of perceived benefit to be gained by using the STMS, coupled with frustration over having to manage yet another communication tool. Secondhand reports of STMS issues prevented new users from trying the STMS, which led to fewer potential communication partners and perpetuated the perceived lack of benefit. Healthcare organizations seeking to implement STMS should pursue strategies that clearly and repeatedly illustrate STMS’s relative advantage, provide STMS access to the greatest number of healthcare professionals, and minimize communication overload via the creation and dissemination of firm communication policies.
References
O’Leary KJ, Liebovitz DM, Wu RC, et al. Hospital-based clinicians’ use of technology for patient care-related communication: a national survey. J Hosp Med 2017;12(7):530–5.
Shah DR, Galante JM, Bold RJ, Canter RJ, Martinez SR. Text messaging among residents and faculty in a university general surgery residency program: prevalence, purpose, and patient care. J Surg Educ [Internet] 2013 [cited 2020 Jun 7];70(6). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3824151/
Kuhlmann S, Ahlers-Schmidt CR, Steinberger E. TXT@WORK: pediatric hospitalists and text messaging. Telemedicine and e-Health 2014;20(7):647–52.
Freundlich RE, Freundlich KL, Drolet BC. Pagers, smartphones, and HIPAA: finding the best solution for electronic communication of protected health information. J Med Syst 2017;42(1):9.
Texting - Use of Secure Text Messaging for Patient Information | Laboratory | Leadership LD | The Joint Commission [Internet]. [cited 2021 Dec 9];Available from: https://www.jointcommission.org/standards/standard-faqs/laboratory/leadership-ld/000002187/
Liu X, Sutton PR, McKenna R, et al. Evaluation of secure messaging applications for a health care system: a case study. Appl Clin Inform 2019;10(1):140–50.
Jhala M, Menon R. Examining the impact of an asynchronous communication platform versus existing communication methods: an observational study. BMJ Innovations [Internet] 2021 [cited 2021 Jun 26];7(1). Available from: https://innovations.bmj.com/content/7/1/68
Przybylo JA, Wang A, Loftus P, Evans KH, Chu I, Shieh L. Smarter hospital communication: secure smartphone text messaging improves provider satisfaction and perception of efficacy, workflow. Journal of Hospital Medicine 2014;9(9):573–8.
Patel MS, Patel N, Small DS, et al. Change in length of stay and readmissions among hospitalized medical patients after inpatient medicine service adoption of mobile secure text messaging. J Gen Intern Med 2016;31(8):863–70.
Hansen JE, Lazow M, Hagedorn PA. Reducing interdisciplinary communication failures through secure text messaging: a quality improvement project. Pediatr Qual Saf 2018;3(1):e053.
Hagedorn PA, Singh A, Luo B, Bonafide CP, Simmons JM. Secure text messaging in healthcare: latent threats and opportunities to improve patient safety. J Hosp Med 2020;15(6):378–80.
Tsega S, Kalra A, Sevilla CT, Cho HJ. A bottom-up approach to encouraging sustained user adoption of a secure text messaging application. Appl Clin Inform 2019;10(2):326–30.
Byrd IV TF, Kim JS, Yeh C, Lee J, O’Leary KJ. Technology acceptance and critical mass: Development of a consolidated model to explain the actual use of mobile health care communication tools. Journal of Biomedical Informatics 2021;117:103749.
Nadal C, Sas C, Doherty G. Technology acceptance in mobile health: scoping review of definitions, models, and measurement. Journal of Medical Internet Research 2020;22(7):e17256.
Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Quarterly 1989;13(3):319–40.
Sittig DF, Singh H. A new socio-technical model for studying health information technology in complex adaptive healthcare systems. Qual Saf Health Care 2010;19(Suppl 3):i68–74.
Shachak A, Kuziemsky C, Petersen C. Beyond TAM and UTAUT: future directions for HIT implementation research. Journal of Biomedical Informatics 2019;100:103315.
Moullin JC, Dickson KS, Stadnick NA, Rabin B, Aarons GA. Systematic review of the Exploration, Preparation, Implementation, Sustainment (EPIS) framework. Implementation Sci 2019;14(1):1.
Holtrop JS, Rabin BA, Glasgow RE. Qualitative approaches to use of the RE-AIM framework: rationale and methods. BMC Health Serv Res 2018;18(1):177.
Setchell J, Leach LE, Watson BM, Hewett DG. Impact of identity on support for new roles in health care: a language inquiry of doctors’ commentary. Journal of Language and Social Psychology 2015;34(6):672–86.
O’Cathain A, Thomas KJ. “Any other comments?” Open questions on questionnaires – a bane or a bonus to research? BMC Medical Research Methodology 2004;4(1):25.
Garcia J, Evans J, Reshaw M. “Is There Anything Else You Would Like to Tell Us” – methodological issues in the use of free-text comments from postal surveys. Quality & Quantity 2004;38(2):113–25.
Anderson E, Solch AK, Fincke BG, Meterko M, Wormwood JB, Vimalananda VG. Concerns of primary care clinicians practicing in an integrated health system: a qualitative study. J Gen Intern Med 2020;35(11):3218–26.
Glaser BG, Strauss AL. The discovery of grounded theory: strategies for qualitative research. 5. paperback print. New Brunswick: Aldine Transaction; 1967.
Kolb SM. Grounded theory and the constant comparative method : valid research strategies for educators. Journal of Emerging Trends in Educational Research and Policy Studies 2012;3(1):83–6.
Hennink MM, Kaiser BN, Weber MB. What influences saturation? Estimating sample sizes in focus group research. Qual Health Res 2019;29(10):1483–96.
Rogers EM. Diffusion of Innovations, 4th Edition. Simon and Schuster; 2010.
Prochaska MT, Bird A-N, Chadaga A, Arora VM. Resident use of text messaging for patient care: ease of use or breach of privacy? JMIR Medical Informatics 2015;3(4):e4797.
Martin G, Khajuria A, Arora S, King D, Ashrafian H, Darzi A. The impact of mobile technology on teamwork and communication in hospitals: a systematic review. J Am Med Inform Assoc 2019;26(4):339–55.
Lou H, Luo W, Strong D. Perceived critical mass effect on groupware acceptance. Eur J Inf Syst 2000;9(2):91–103.
Van Slyke C, Ilie V, Lou H, Stafford T. Perceived critical mass and the adoption of a communication technology. European Journal of Information Systems 2007;16(3):270–83.
Lou H, Chau PYK, Li D. Understanding individual adoption of instant messaging: an empirical investigation. J AIS 2005;6:5.
Wong BM, Quan S, Cheung CM, et al. Frequency and clinical importance of pages sent to the wrong physician. Archives of Internal Medicine 2009;169(11):1069–81.
Patel N, Siegler JE, Stromberg N, Ravitz N, Hanson CW. Perfect storm of inpatient communication needs and an innovative solution utilizing smartphones and secured messaging. Appl Clin Inform 2016;7(3):777–89.
Vaisman A, Wu RC. Analysis of smartphone interruptions on academic general internal medicine wards. Frequent interruptions may cause a “crisis mode” work climate. Appl Clin Inform 2017;8(1):1–11.
Coombe J, Harris ML, Loxton D. Motivators of contraceptive method change and implications for long-acting reversible contraception (non-)use: a qualitative free-text analysis. Sex Reprod Healthc 2019;19:71–7.
Weaver L, Beebe TJ, Rockwood T. The impact of survey mode on the response rate in a survey of the factors that influence Minnesota physicians’ disclosure practices. BMC Med Res Methodol 2019;19(1):1–7.
Cunningham CT, Quan H, Hemmelgarn B, et al. Exploring physician specialist response rates to web-based surveys. BMC Med Res Methodol 2015;15(1):32.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Byrd, T.F., Speigel, P.S., Cameron, K.A. et al. Barriers to Adoption of a Secure Text Messaging System: a Qualitative Study of Practicing Clinicians. J GEN INTERN MED 38, 1224–1231 (2023). https://doi.org/10.1007/s11606-022-07912-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-022-07912-8