Abstract
Importance
In OECD countries, pharmaceutical spending reached around 800 billion USD in 2013, accounting for about 20% of total spending in the retail sector. Pharmaceutical expenditures are steadily increasing in South Korea, necessitating strategies to promote efficiency.
Objective
This study investigated factors associated with high-cost users (HCUs), who account for the majority of outpatient prescriptions in the total South Korean population. The top 20 frequently prescribed therapeutic subgroups were also investigated.
Design
This is an observational study performed using health insurance claims data in 2019.
Participants
In total, 44,744,632 people (including 6,806,339 aged 65 years or older) who were prescribed outpatient medications were included.
Main measures
HCUs were defined as those for whom prescription drug costs were in the top 5%. Multivariate logistic regression analysis was performed using factors including age, insurance type, number of prescription drugs, outpatient visit days, prescription treatment days, and chronic diseases.
Results
HCUs accounted for 3.6 million (5% of the total population) and 1.4 million (21.1% of those 65 years or older). Furthermore, 4.1% of HCUs in the total population had few comorbidities. Male sex, older age, insurance (Medical Aid), comorbidities, chronic diseases, number of prescription drugs, outpatient visit days, and prescription days were all associated with an increased probability of being an HCU. The highest spending was found for B01 (antithrombotic agents) with 0.4 billion USD, followed by C10 (lipid-modifying agents) and A10 (drugs used in diabetes). The proportion of spending for HCUs among the general population was highest in L01 (antineoplastic agents), at 98.2%, and L04 (immunosuppressants), at 87.8%, whereas among the elderly, the highest proportions were found for B01 (antithrombotic agents), at 44.5%, and N06 (antidepressants), at 44.3%.
Conclusion
Age and multiple chronic conditions were strongly associated with HCUs, and it seems necessary to reduce drug prescriptions in patients without complex comorbidities. Several measures should target those without multiple chronic conditions who are nonetheless HCUs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With the increase in the elderly population, multiple chronic conditions have become more prevalent and the introduction of innovative new drugs has contributed to a steady growth in drug expenditures. It has been reported that a small proportion of patients consume a disproportionately large share of health care spending. For example, studies in the USA and Canada have found that 5% of the total population accounted for half of all health care spending.1,2
According to previous studies examining the characteristics of patients with high medical costs, it has been suggested that high-cost patients are not homogeneous, but rather a diverse group with a variety of clinical and social needs. Frequently described characteristics of high-cost users (HCUs) include advanced age, low education level, low income, poor self-perceived health, and multiple chronic conditions.2,3,4,5 Joynt and Khullar suggested that 9.6–10.4% of HCU spending could be more efficiently managed.3,6
As drug spending is expected to increase significantly owing to the aging of the population and the emergence of new expensive drugs, research on efficient drug expenditures is necessary. Weymann referred to those in the top 10% in terms of drug expenditures in Canada as HCUs of prescription drugs,7 Øymoen described those were in the top 1% of usage based on Danish registration data as heavy users of prescription drugs,8 and Saastamoinen defined high-cost patients as those responsible for the top 5% of drug costs based on Finland’s registration data.9
South Korea achieved universal health insurance coverage based on the National Health Insurance (NHI) program in 1989. It is a country witnessing extremely rapid population aging, and there are concerns regarding an insurance fiscal deficit due to the risk of declining premium income. South Korea has also been expanding coverage for new drugs since the introduction of the positive listing system in 2007. In light of the importance of ensuring access to medicines and promoting financial sustainability of the health insurance system, it is important to establish a strategy to curb the inefficient use of drugs.
Rising drug spending has been a constant issue, and several studies have investigated the factors driving increasing drug spending in South Korea. Most research found that the quantity of drugs (number of prescriptions) contributed to increased prescription drug spending.10,11,12 However, few studies have examined factors affecting high drug spending. Further, we investigated factors associated with HCUs and the top 20 most frequently prescribed drugs according to the therapeutic classification.
Methods
This study received review and approval from the Institutional Review Board of the Health Insurance Review & Assessment Service (HIRA).
Data Source and Study Population
This was an observational study using 2019 health insurance claims data. South Korea has a single-payer health insurance system, which provides coverage for all citizens and reimburses providers on a fee-for-service basis. The data include all inpatient and outpatient treatment records. Demographic characteristics, medical conditions, medical service utilization (visit dates, examinations, and operations), and pharmaceutical drugs (ingredient names, number of treatment days, drug costs) are all included in medical claims, and all claims are electronically submitted. Medical conditions are classified according to the International Classification of Diseases, Tenth Revision (ICD-10). Medicines are recorded using the international nonproprietary names and the codes of individual products. In South Korea, most people tend to visit medical institutions to obtain prescriptions rather than purchasing over-the-counter medications at pharmacies, so most medicine use of the total population is recorded through electronic claims in the health insurance database.
The subjects of the analysis were patients who were eligible for National Health Insurance, Medical Aid, and the Veterans Health Service and who received outpatient medication prescriptions from tertiary hospitals, general hospitals, hospitals, or clinics—excluding pharmacies because the dispensing information at the pharmacy overlaps with the prescribing information at the medical institutions—from January through December 2019. For drug spending, we took a social perspective; therefore, drug spending referred to total spending, including patient out-of-pocket costs and the value-added tax (VAT) at the retail price.
Definition of High-Cost Users of Prescription Drugs
We defined HCUs as patients with high drug costs. We used the threshold value for HCU of the top 5%, or 1128 USD, based on a previous study.9
Explanatory variables were classified into predisposing factors (age and sex), enabling factors (insurance eligibility), and need factors (disease). Regarding chronic diseases, the presence or absence of major diseases was investigated, considering the prevalence and incidence, the Elixhauser comorbidity index (ECI),13 and multimorbidity number. The ECI score was calculated to estimate the severity of disease, and categorized as 0, 1, 2, and 3 or more. We also selected as confounders the number of chronic diseases that could influence health care utilization, which included hypertension, ischemic heart disease, stroke, hyperlipidemia, diabetes, stomach ulcer, renal failure, liver failure, chronic obstructive pulmonary disease (COPD), pneumonia, asthma, osteoporosis, dementia, degenerative arthritis, and fracture. Chronic diseases were counted if they were a principal diagnosis or a first secondary diagnosis, and the ECI was calculated for all diagnoses. The average number of drugs prescribed per patient was categorized into 1–4 and ≥ 5; the number of outpatient visits was divided into < 14 days, 14–30 days, and ≥ 31 days; and the sum of prescription days was defined as ≥ 6.75 days (top 5%).
Age was categorized into < 18 years, 18–44 years, 45–64 years, 65–74 years, and ≥ 75 years. The ECI score was classified into 0, 1, 2, and ≥ 3. The multimorbidity variable was divided into 0, 1, 2, and ≥ 3.
Classification of Medicines
Therapeutic subgroups were classified according to the Anatomical Therapeutic Chemical (ATC) classification system of the World Health Organization Collaborating Center (WHOCC).14 We used drug classifications based on ATC level 2 (therapeutic class).
The number of patients using a certain drug was defined as the number of patients who were prescribed a medication from the same therapeutic subgroup in 2019; this did not entail double counting within the same therapeutic group, but allowed for multiple counting across different therapeutic groups if a patient was prescribed multiple therapeutic subgroup drugs. The prevalence proportion ratio was calculated as the ratio of the number of patients with prescriptions divided by the general population.
Statistical Analysis
Multivariable logistic regression was performed to identify the factors affecting HCUs. In order to resolve the multicollinearity problem, model 1 was created using only the ECI, model 2 used only the multimorbidity number, and model 3 used only diagnoses. For the diagnosis dummy model, only the diagnosis dummy variable was used as the explanatory variable, as predisposing factors (sex, age, etc.), enabling factors (insurance eligibility), and need factors (number of prescription drugs, number of outpatient visits, and long-term prescription treatment) were removed from the stepwise method.
Multivariable logistic regression analysis was performed for the entire population and those aged ≥ 65 years. Before performing logistic regression analysis, multicollinearity between explanatory variables was determined, the goodness of fit of the models was verified using the likelihood-ratio test, and the significance of coefficients was tested using the Wald statistic and the corresponding significance level. As a result of the stepwise selection process used to identify the significant variables that affected the dependent variable, all explanatory variables for each model were found to have an effect and therefore were included in the model as final variables. The likelihood-ratio test yielded a p value of < 0.0001, indicating that the models were significantly acceptable.
The top 20 most frequently prescribed therapeutic subgroups in the HCUs were compared with those in the entire population. SAS Enterprise version 7.1 (SAS Institute, Cary, NC, USA) was used for all analyses.
Results
General Characteristics
This study included 44.77 million people (of whom 6.8 million were ≥ 65 years of age) who received outpatient prescriptions in 2019 in South Korea. Table 1 summarizes the distribution of prescription drug spending and prescription drug treatment days. The mean prescription drug expenditure per patient was 246 USD for the entire population and 750 USD for those 65 years or older. The top 3% of the people accounted for 25.5% of the total annual drug costs, the top 10% of the people accounted for half of the total drug costs (53.2%), and the top 25% of the people accounted for 80.5% of the total drug costs. The 25th percentile of total prescription drug costs was 1.6 million USD.
As shown in Table 2, HCUs (prescription drug expenditures ≥ 1128 USD) accounted for 5% of the total population of 44.77 million, whereas among those 65 years or older, 21.1% were HCUs. HCUs were much older than the other prescription drug users, and they predominantly had Medical Aid. The prevalence of HCUs and low-cost users (LCUs) by chronic disease was as follows: 54.3% of HCUs and 14.2% of LCUs had hypertension; 43.4% and 6%, diabetes; 34.9% and 11.3%, hyperlipidemia; and 3% and 1%, cancer. A similar pattern was also observed in those 65 years or older. The proportion of HCUs with an ECI of ≥ 3 was 69%, compared to 9.7% in low-cost users, and the proportion of patients with multimorbidity (≥ 1 chronic disease) was also higher among HCUs. HCUs with an ECI of 0 accounted for 4.1% of the total population and 1.8% of the elderly.
Factors Associated with High-Cost Users
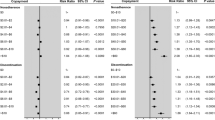
Table 3 summarizes the results of the logistic regression analysis performed to explore variables associated with the probability of being an HCU. In model 1, when patient characteristics were adjusted, sex, age, insurance type, number of prescription drugs, number of outpatient visit days, long-term prescription drug use, and comorbidities were all associated with the increased odds of being an HCU.
In the total population, when compared to those in the age range of 18–44 years, the odds of being an HCU was ≥ 14 times higher for those ≥ 75 years of age (odds ratio [OR], 6.37; 95% CI, 6.32–6.42), and the OR was 4.24 (95% CI, 4.21–4.27) for those 65–74 years of age and 2.38 (95% CI, 2.36–2.40) for those 45–64 years of age. Compared to those covered by National Health Insurance, those who received Medical Aid were 2.23 times more likely to be HCUs (95% CI, 2.36–2.40). A linear increase was also observed with regard to the ECI (OR, 2.63; 95% CI, 2.61–2.66, for a score of 1; OR, 5.68; 95% CI, 5.63–5.73, for a score of 2; and OR, 12.52; 95% CI, 12.43–12.61, for a score of ≥ 3) and the number of outpatient visit days (OR 2.26; 95% CI, 2.25–2.27, for 15–31 days; OR, 3.44; 95% CI, 3.42–3.46 for ≥ 31 days). The odds of being an HCU were 3.94 times higher among those with ≥ 5 prescription drugs, and the odds were 8.79 times higher in those with ≥ 678 prescription days.
In the subgroup consisting of those ≥ 65 years of age, all other factors showed similar patterns, but the number of prescription drugs showed a higher OR in the elderly (OR, 3.94; 95% CI, 3.92–3.95) than in the total population (OR, 4.18; 95% CI, 4.12–4.24). Model 2 showed similar results to those of model 1. Compared to patients without chronic diseases, the OR of being an HCU was 10.94 times higher (95% CI, 10.86–11.03) in patients with ≥ 3 comorbidities, 6.53 times higher (95% CI, 6.49–6.58) in patients with 2 comorbidities, and 3.61 times higher (95% CI, 3.58–3.63) in patients with 1 comorbidity.
In model 3, the odds of being an HCU increased by 10.94 times for patients with stroke, 10.5 times for those with renal failure, 7.31 times for those with dementia, and 6.71 times for with diabetes in the entire population; among those 65 years or older, the probability rose by 5.41 times for those with stroke, 3.85 times for those with diabetes, 3.73 times for those with dementia, and 3.85 times for those with diabetes.
Prevalence and Drug Expenditures According to Therapeutic Subgroups
High prevalence rates (number of HCUs in the entire population who were prescribed outpatient drugs) were found for A02 (drugs for acid-related disorders), M01 (anti-inflammatory and antirheumatic products), N02 (analgesics), A03 (drugs for functional gastrointestinal disorders), and C10 (lipid-modifying agents) according to ATC level 2. The proportions of HCUs were high for therapeutic groups B01 (antithrombotic agents), A10 (drugs used in diabetes), N07 (other nervous system drugs), C10 (lipid-modifying agents), and N06 (psychoanaleptics). A similar pattern was found among ≥ 65-year-old HCUs.
The analysis of drug spending classified according to ATC level 2 showed that the top 20 therapeutic subgroups accounted for 81.1% of total drug expenditures. The highest drug spending of HCUs in the entire population was found for B01 (antithrombotic agents), A10 (drugs used in diabetes), N07 (other nervous system drugs), C10 (lipid-modifying agents), and N06 (psychoanaleptics). The proportion of HCUs based on spending was high for L01 (antineoplastic agents), L04 (immunosuppressants), and B01 (antithrombotic agents). The pattern was somewhat different among ≥ 65-year-old HCUs, who had high usage of B01 (antithrombotic agents), N06 (psychoanaleptics), and N07 (other nervous system drugs) (Table 4).
Discussion
In order to promote access to medications and financial sustainability of health insurance, there is an increasing need to establish measures to curb the inefficient use of medicines, both in South Korea and around the world. To our knowledge, this is the first study to examine HCUs for outpatient prescription drug spending in the general population in South Korea. In this large-population-based study of more than 44.77 million individuals, the top 3% of people accounted for 25.5% of the total drug spending, while the top 10% of people accounted for half. We defined HCUs as those for whom prescription drug costs were in the top 5%, as in a previous study.
We examined the associations of age, multiple chronic diseases, number of physician encounters, and days of therapy with the likelihood of being an HCU in terms of drug spending. In the overall population, we found that 12.52 times as many patients with ECI scores of 3 or higher, and 10.94 times as many with three or more chronic diseases, were HCUs. Patients with stroke, renal failure, and dementia were 10.94, 10.01, and 7.31 times more likely to be HCUs, respectively, than those without these diseases. In people 65 years or older, while other effects (sex, age, type of health insurance, and physician encounters) were similar, a higher number of medications was associated with a higher likelihood of being an HCU in terms of drug spending. Several studies have examined the characteristics of HCUs in terms of health care costs, showing the most costly diseases to be cancer, heart disease, and mental disorders.3,5
HCUs were more likely to be female and older, as reported in previous studies.15,16 In addition, HCUs were more common among those receiving Medical Aid, which is consistent with previous reports.16,17 There is no consensus on how to optimize the spending of HCUs; some researchers have suggested that their expenditures can be reduced, while others are skeptical of the feasibility of such measures.3,6 Considering that HCUs with an ECI of 0 made up 4.1% of the total population, compared to 1.8% of those 65 years or older, there seems to be room to reduce drug spending in patients without complex comorbidities.
This study also investigated factors associated with HCUs and the top 20 most frequently prescribed therapeutic subgroups classified according to ATC level 2, and compared frequently prescribed medicines in the total population and HCUs across the entire South Korean population, both overall and in the subgroup of those 65 years or older. Meanwhile, drug spending of HCUs was the highest in B01 (antithrombotic agents) with 397.7 million USD, followed by C10 (lipid-modifying agents) and A10 (drugs used in diabetes), and the proportion of HCUs among the total population based on drug expenditures was the highest for therapeutic subgroups L01 (antineoplastic agents), at 98.2%, followed by L04 (immunosuppressants), at 87.8%, and B01 (antithrombotic agents), at 60%, in the entire population. For the elderly, the drug expenditures were similar to that of the entire population. Among the elderly population, HCUs had high levels of spending for B01 (antithrombotic agents), N06 (psychoanaleptics), and N07 (other nervous system drugs).
Concerns have been raised regarding economic losses caused by discarding unused medications.18 A substantial amount of pharmaceutical waste has been reported to be generated worldwide. The National Audit Office (NAO) of the UK estimates that at least 10% of medicines are wasted, which translates to 6.7 million Euros.19 In South Korea, the payment system is based on a fee-for-service system, which often results in overlapping prescriptions of digestives to prevent gastrointestinal disorders due to physicians’ prescribing patterns.
In Denmark, the most frequently prescribed medications among the top 1% heavy drug users were C03 (diuretics), A02 (drugs for acid-related disorder), C09 (agents acting on the renin-angiotensin system), and B01 (antithrombotic agents). In the current study, the therapeutic subgroups that accounted for disproportionately large proportions of drug expenditures among HCUs were B01 (antithrombotic agents), C10 (lipid-modifying agents), A10 (drugs used in diabetes), and C09 (agents acting on the renin-angiotensin system) in the entire population and N06 (antidepressants) was added in those 65 years or older.
This is the first study to investigate the characteristics of medications that account for a large proportion of drug expenditures using NHI claims data in South Korea. South Korea’s NHI covers reimbursement to all medical providers on a fee-for-service basis. We used large-population data; therefore, the results of this study are generalizable to the South Korean population. Secondly, above all, this study confirmed the presence or absence of a medical condition in each patient by sorting by patient for all diagnoses that incurred medical expenditures per visit. As we included all medical conditions during the period of 1 year, all chronic diseases of patients are expected to have been included in the analysis. Thirdly, this study attempted to adjust for the influence of age as much as possible by performing a subgroup analysis of those 65 years or older.
Our study has the following main limitation. As only outpatient diagnoses and outpatient prescriptions were analyzed, drug expenditures incurred during hospitalization were not included in the analysis. Secondly, we used claims data for most of our analysis, which may not fully capture clinical risk. Furthermore, although we tried to adjust for as many confounding variables as possible, there was a limitation in terms of internal validity in that unmeasurable variables could not be included. Thirdly, while our dataset covers the entire national population, including foreigners, patients in other countries may differ from our population. For example, access to health care is very high in South Korea; therefore, the number of encounters per person was 16.6 in 2017, which is the highest per capita utilization of health services among OECD countries; in contrast, the average of the 33 OECD member countries was 6.8 encounters.20 In South Korea, even medications for mild illnesses are prescribed at medical institutions, so it can be assumed that most of the medications dispensed are included in the database. Fourthly, we analyzed claims data; therefore, some of the prescriptions might not have actually been dispensed. In addition, this study was conducted in South Korea, which has unique characteristics in terms of the epidemiology of diseases and specific aspects of medical practice, and its health care system (national health insurance). Lastly, we sought to identify multimorbidity-related factors using ECI and the number of comorbidities and chronic diseases. This comparison in terms of measurements of morbidity is a substantial and novel contribution of this study, and multimorbidity was found to be the factor most strongly associated with being an HCU. However, characteristics such as morbidity are non-modifiable factors; therefore, strategies for reducing or limiting the number of medications or days of therapy might be effective as interventions for prescribing behaviors.
Conclusion
This study deepens our understanding of the needs and drug utilization patterns of HCUs. In conclusion, despite this limitation, age, sex, insurance type, and especially multimorbidity were found to be factors that affected the odds of being an HCU. It is of particular note that there seems to be room to reduce drug spending in patients without complex comorbidities. Further research should examine the causes associated with a comorbidity index of 0 among HCUs.
References
Pritchard D, Petrilla A, Hallinan S, Taylor DH, Jr., Schabert VF, Dubois RW. What Contributes Most to High Health Care Costs? Health Care Spending in High Resource Patients. J Manag Care Spec Pharm 2016;22:102-9.
Ronksley PE, McKay JA, Kobewka DM, Mulpuru S, Forster AJ. Patterns of health care use in a high-cost inpatient population in Ottawa, Ontario: a retrospective observational study. CMAJ Open 2015;3:E111-8.
Joynt KE, Gawande AA, Orav EJ, Jha AK. Contribution of preventable acute care spending to total spending for high-cost Medicare patients. JAMA 2013;309:2572-8.
Rosella LC, Fitzpatrick T, Wodchis WP, Calzavara A, Manson H, Goel V. High-cost health care users in Ontario, Canada: demographic, socio-economic, and health status characteristics. BMC Health Serv Res 2014;14:532.
Toxvaerd CG, Benthien KS, Andreasen AH, Nielsen A, Osler M, Johansen NB. Chronic Diseases in High-Cost Users of Hospital, Primary Care, and Prescription Medication in the Capital Region of Denmark. J Gen Intern Med 2019;34:2421-6.
Khullar D, Zhang Y, Kaushal R. Potentially Preventable Spending Among High-Cost Medicare Patients: Implications for Healthcare Delivery. J Gen Intern Med 2020;35:2845-52.
Weymann D, Smolina K, Gladstone EJ, Morgan SG. High-Cost Users of Prescription Drugs: A Population-Based Analysis from British Columbia, Canada. Health Serv Res 2017;52:697-719.
Øymoen A, A. Pottegård, Almarsdóttir AB. Characteristics and drug utilization patterns for heavy users of prescription drugs among the elderly: a Danish register-based drug utilization study. Eur J Clin Pharmacol 2015;71:751-8.
Saastamoinen LK, Verho J. Drug expenditure of high-cost patients and their characteristics in Finland. Eur J Health Econ: HEPAC: Health Economics in Prevention and Care 2013;14:495-502.
Kwon HY, Yang B, Godman B. Key Components of Increased Drug Expenditure in South Korea: Implications for the Future. Value in health regional issues 2015;6:14-21
Jo JS, Kim YM, Paek KW, Bea MH, Chun K, Lee S. Factors Contributing to Increases in Prescription Drug Expenditures Borne by National Health Insurance in South Korea. Yonsei Med J 2016;57:1016-21.
Lee H, Park D, Kim DS. Determinants of Growth in Prescription Drug Spending Using 2010-2019 Health Insurance Claims Data. Front Pharmacol 2021;12:681492.
Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol 1994;47:1245-51.
WHOCC. Anatomical Therapeutic Chemical (ATC)/Defined Daily Dose (DDD) Index. Oslo: WHOCC; 2020.
Hovstadius B, Astrand B, Petersson G. Dispensed drugs and multiple medications in the Swedish population: an individual-based register study. BMC Clin Pharmacol 2009;9:11.
Pappa E, Kontodimopoulos N, Papadopoulos AA, Tountas Y, Niakas D. Prescribed-drug utilization and polypharmacy in a general population in Greece: association with sociodemographic, health needs, health-services utilization, and lifestyle factors. Eur J Clin Pharmacol 2011;67:185-92.
Nielsen MW, Hansen EH, Rasmussen NK. Prescription and non-prescription medicine use in Denmark: association with socio-economic position. Eur J Clin Pharmacol 2003;59:677-84.
OECD. Tackling Wasteful Spending on Health. Paris: OECD; 2017.
Office NA. Prescribing costs in primary care. London: NAO; 2007.
OECD. Health Status - OECD Statistics. Paris: OECD Publishing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Park, D., Lee, H. & Kim, DS. High-Cost Users of Prescription Drugs: National Health Insurance Data from South Korea. J GEN INTERN MED 37, 2390–2397 (2022). https://doi.org/10.1007/s11606-021-07165-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-021-07165-x